Hormone replacement therapy (HRT) is a medical strategy that replenishes hormones your body has stopped producing in adequate amounts. It’s a precise, data-driven approach used to relieve symptoms and counter health risks tied to hormonal decline—most commonly seen with menopause in women, andropause in men, or as part of gender-affirming care.
At its core, HRT is about restoring your body’s natural equilibrium.
A Modern Approach to Hormonal Balance

Imagine your body’s hormonal system as a finely tuned orchestra. For decades, key hormones—like estrogen, progesterone, and testosterone—play their parts perfectly, contributing to your energy, mood, cognitive function, and physical strength. But as we age, some of these crucial instruments can start to fall out of tune, creating a discordant effect that we feel as disruptive symptoms.
So, what is hormone replacement therapy in this context? It’s the conductor stepping in to restore harmony. By reintroducing specific hormones in carefully measured doses, a specialist can help bring the entire system back into balance, quieting the noise and supporting your long-term wellness.
Moving Beyond Symptom Management
Not too long ago, HRT was seen almost exclusively as a fix for menopausal hot flashes. And while it remains highly effective for that purpose, its modern application is far broader and more sophisticated.
Today, leading physicians view HRT as a key component of proactive, preventive medicine. The goal is to optimize your healthspan—the years of life spent in good health, not just your lifespan. This shift in perspective treats hormonal balance as a cornerstone of peak performance, focusing on goals like:
- Sustaining mental sharpness: Cutting through the debilitating “brain fog” that often accompanies hormonal shifts.
- Maintaining physical vitality: Protecting muscle mass, bone density, and metabolic health against age-related decline.
- Enhancing overall quality of life: Radically improving sleep, stabilizing mood, and restoring energy levels.
The demand for this advanced approach is surging. The global HRT market was valued at $23.02 billion in 2023 and is projected to hit $38.47 billion by 2032. This isn’t just a trend; it signals a fundamental shift in how we approach aging. For a growing number of patients, HRT is a calculated strategy for longevity and sustained performance. You can read more about these market trends and their implications for personalized medicine.
Modern hormone replacement therapy isn’t about chasing youth; it’s about preserving health. It’s a calculated medical strategy to ensure the biological systems that drive your energy, focus, and resilience continue to function at their best, regardless of age.
Ultimately, understanding HRT today means seeing it not as a simple patch, but as a sophisticated, highly personalized medical program. It demands expert guidance, detailed diagnostic testing, and continuous monitoring to ensure both safety and effectiveness, turning what was once seen as an inevitable decline into an opportunity for continued vitality.
Who Uses HRT and Why

Hormone replacement therapy isn’t a one-size-fits-all solution. It’s a sophisticated medical strategy, customized to an individual’s unique biology and life stage. The choice to start HRT is deeply personal, usually driven by a need to manage disruptive symptoms, head off long-term health risks, or simply maintain an edge during periods of major hormonal shifts.
Three distinct groups stand to gain the most from expertly managed hormone therapy. While each journey is different, they all share a common goal: using HRT to achieve specific, life-enhancing outcomes.
Navigating Menopause with Menopausal Hormone Therapy
For women, the transition into perimenopause and menopause is one of the most significant biological events of their lives. As the ovaries slow their production of estrogen and progesterone, a cascade of symptoms can follow, disrupting everything from cognitive function to physical well-being. This isn’t a minor inconvenience; it’s a fundamental change that demands a strategic response.
Women turn to Menopausal Hormone Therapy (MHT)—often just called HRT—to get control over symptoms that directly impact their day-to-day performance.
- Vasomotor Symptoms: These are the infamous hot flashes and night sweats that can completely derail sleep and cause profound discomfort. MHT is hands-down the most effective treatment for getting them under control.
- Cognitive and Mood Changes: Many women describe a persistent “brain fog,” trouble concentrating, and a shorter fuse. Restoring estrogen levels can bring back mental clarity and stabilize mood.
- Physical and Urogenital Health: Declining estrogen can lead to vaginal dryness, painful intercourse, and even recurrent urinary tract infections. This hormone is also essential for bone density, and its absence puts women at a much higher risk for osteoporosis.
For high-achieving women, MHT is a powerful tool for maintaining momentum. By addressing the root hormonal cause, it allows them to preserve their energy, focus, and vitality through a challenging—but entirely manageable—transition.
Restoring Vitality Through Testosterone Replacement Therapy
Men undergo their own age-related hormonal decline, a gradual process known as andropause or late-onset hypogonadism. While it’s less abrupt than menopause, the steady drop in testosterone can take a serious toll on a man’s health, confidence, and overall sense of drive.
Testosterone Replacement Therapy (TRT) is designed to bring this critical hormone back to an optimal range, fighting back against the telltale symptoms of low testosterone.
By correcting the hormonal deficit, TRT empowers men to reclaim their physical strength, mental edge, and overall sense of well-being. It’s a proactive strike against the slow erosion of vitality that often comes with age.
Men often seek TRT to address a frustrating constellation of symptoms:
- Persistent Fatigue and Low Energy: A deep-seated lack of drive that sleep just doesn’t seem to fix.
- Loss of Muscle Mass and Strength: Finding it harder to build or even maintain muscle, no matter how hard they work in the gym.
- Reduced Libido and Sexual Function: A clear drop in sex drive and overall performance.
- Mental and Emotional Shifts: Experiencing more irritability, apathy, or a general lack of motivation.
For men navigating demanding careers, getting on TRT can feel like flipping a switch back on. If you’re looking for a deeper dive, this overview of testosterone replacement therapy options is a great resource.
Aligning Identity with Gender-Affirming Hormone Therapy
A third, and profoundly important, use of hormone therapy is for transgender and gender non-conforming individuals. Here, gender-affirming hormone therapy is a medically necessary intervention that helps align a person’s physical body with their core gender identity. This isn’t about performance or anti-aging; it’s about fundamental well-being and allowing someone to live as their authentic self.
The therapy involves administering hormones to encourage the secondary sex characteristics of the affirmed gender.
- Feminizing Hormone Therapy: This typically involves estrogens and anti-androgens to promote breast development, soften the skin, and shift body fat to a more feminine pattern.
- Masculinizing Hormone Therapy: This uses testosterone to deepen the voice, stimulate facial and body hair growth, and build muscle mass.
The goal is deeply personal and absolutely essential. This therapy is a cornerstone of care for reducing gender dysphoria—the significant distress caused by the mismatch between one’s gender identity and assigned sex at birth. The results are life-changing, leading to dramatic improvements in mental health, social functioning, and overall quality of life.
Balancing The Benefits And Risks Of HRT

Any serious conversation about what hormone replacement therapy is has to honestly weigh the good against the bad. For many, that discussion is still haunted by the ghosts of outdated studies from decades ago, which painted HRT with a broad, scary brush. But let’s be clear: the landscape has fundamentally changed. We’ve moved into an era of precision medicine, and our understanding of hormonal science is lightyears ahead of where it was.
The decision to start HRT is a partnership between you and your physician, centered on a deep dive into your unique health profile, goals, and risk factors. The objective isn’t just to write a prescription. It’s to design a meticulously managed health protocol that maximizes the profound, life-enhancing benefits while actively—and intelligently—minimizing potential risks.
This modern, data-driven strategy has completely flipped the old risk-benefit equation. The HRT market is growing by 5.8–6.7% every year, not because people are ignoring the risks, but because the medical community has responded with a smarter approach: lower, personalized doses, safer delivery methods, and constant monitoring.
The Clear And Compelling Benefits
When managed by a true expert, optimized hormones do far more than just quiet down symptoms. They become a foundational part of your long-term health strategy, safeguarding your body’s most critical systems against the typical decline that comes with aging.
- Protecting Bone Density: Estrogen is the guardian of your skeleton. HRT is one of the most powerful tools we have to prevent osteoporosis and dramatically cut the risk of a debilitating fracture later in life.
- Enhancing Cognitive Sharpness: That “brain fog” that comes with hormonal shifts isn’t just in your head. By restoring balance, HRT helps bring back mental clarity, focus, and memory, keeping you at the top of your game.
- Stabilizing Mood And Well-being: Hormonal chaos can wreak havoc on your emotions, fueling irritability, anxiety, and even depressive symptoms. Rebalancing those levels often brings a remarkable improvement in mood and emotional resilience.
- Supporting Cardiovascular Health: This is a big one. For many people, especially women who start HRT within 10 years of menopause, the therapy can have a protective effect on the heart by improving cholesterol profiles and vascular function.
A Modern Strategy For Mitigating Risks
The secret to safe and effective HRT isn’t pretending risks don’t exist. It’s about proactive, intelligent risk management. The one-size-fits-all approach is dead. Top-tier physicians now use a multi-layered strategy to build a program that’s as safe as it is effective for your specific biology.
The question isn’t whether HRT has risks—every effective medical treatment does. The real question is how an expert physician can systematically minimize those risks through personalization, advanced delivery methods, and vigilant monitoring, making the benefits overwhelmingly favorable for the right candidate.
This modern safety protocol is built on several key pillars:
1. Personalized Dosing Your treatment starts with the lowest effective dose. From there, it’s carefully fine-tuned based on how you feel and what your follow-up lab work shows. This ensures you get all the benefits without any unnecessary exposure.
2. Bioidentical Formulations Many specialists now prefer using bioidentical hormones. These are molecularly identical to the hormones your own body produces, which often leads to better tolerance and more predictable, natural-feeling results. To dive deeper, check out this comprehensive bioidentical hormone replacement therapy guide.
3. Advanced Delivery Methods How a hormone gets into your body is critically important. Transdermal methods—like patches, gels, or creams—allow hormones to absorb directly into the bloodstream, completely bypassing the liver. This simple change in delivery significantly lowers the risk of blood clots that was associated with older, oral estrogen pills.
4. Continuous Biomarker Monitoring Your HRT journey doesn’t stop after the first prescription. Regular blood tests and check-ins are non-negotiable. They allow your physician to track your hormone levels, monitor key health markers, and make precise, ongoing adjustments to your protocol. This ensures your therapy remains both safe and perfectly optimized for the long haul.
Your Diagnostic Journey to Hormone Optimization
Starting a hormone optimization program with an elite physician isn’t a casual affair. It’s a meticulous, data-driven process designed from the ground up for maximum safety and unparalleled results. This journey begins long before a single prescription is written. It starts with a deep dive into your unique biology, your personal health history, and exactly what you want to achieve.
Think of this diagnostic phase like creating a detailed blueprint for a custom-built home. A master builder wouldn’t break ground without one, and a top-tier physician won’t design a hormone protocol without a complete picture of your body’s inner workings. This rigorous approach is what separates standard care from true optimization.
The Comprehensive Initial Consultation
Your first step is an in-depth consultation that goes far beyond a routine check-up. This conversation is the absolute cornerstone of your treatment. Here, your doctor will listen—really listen—to understand not just your symptoms, but your lifestyle, daily stressors, family history, and what you’re truly aiming for with HRT.
This dialogue is everything. Are you looking to eliminate brain fog and reclaim your cognitive edge? Do you want to restore the relentless energy needed to excel in your career and still have something left for your family? Or is your focus on the long-term prevention of age-related decline? Your answers steer the entire strategy.
A truly personalized HRT plan is built on a foundation of hard data. The initial consultation and lab work aren’t just formalities; they are the essential first steps that allow a physician to map your unique hormonal landscape and craft a precise, effective, and safe path forward.
After this conversation, it’s time to gather the objective data that will illuminate your body’s current hormonal status. This is where comprehensive lab work becomes indispensable.
Uncovering the Data with Extensive Lab Work
To understand what hormone replacement therapy can actually do for you, your doctor first needs to see exactly what’s happening at a molecular level. A comprehensive blood panel provides this critical insight. We’re not just talking about checking one or two hormone levels; it’s about assessing the entire endocrine system and related health markers that tell the full story.
This detailed testing provides the raw data for your personalized blueprint. Key biomarkers that are almost always measured include:
- Sex Hormones: This includes levels of estradiol (the primary estrogen), total and free testosterone, and progesterone. Measuring both total hormone levels and the “free” (biologically active) portion is critical for getting an accurate picture.
- Binding Globulins: Sex Hormone-Binding Globulin (SHBG) is a protein that binds to sex hormones and makes them inactive. High or low SHBG can dramatically change how much active hormone your body can actually use, regardless of total levels.
- Thyroid Panel: Thyroid hormones (like TSH, Free T3, and Free T4) are the master regulators of your metabolism. An imbalance here can perfectly mimic the symptoms of sex hormone decline, so it’s essential to rule out or address thyroid issues first.
- Metabolic and Inflammatory Markers: Your physician will also look at indicators like fasting insulin, glucose, HbA1c, and C-reactive protein (CRP) to get a clear view of your metabolic health and any underlying systemic inflammation.
Ongoing Monitoring for Long-Term Success
The diagnostic journey doesn’t end after your first set of labs. Far from it. Once your personalized HRT plan is in motion, ongoing monitoring is the key to ensuring long-term safety and success. You can expect follow-up testing at regular intervals—typically a few months after starting and then annually or semi-annually after that.
This continuous stream of data allows your doctor to make precise micro-adjustments to your dosages, ensuring your hormone levels stay squarely in the optimal range. It’s a dynamic process of fine-tuning that confirms the therapy is working as intended while actively safeguarding your health. This vigilant, proactive management is the hallmark of elite-level hormone optimization, turning your treatment into a sustained strategy for peak wellness.
How to Find a Top Physician for Hormone Therapy
Let’s be clear: choosing the right physician is the single most important decision you’ll make on your hormone optimization journey. The quality of your doctor directly dictates the quality of your results and your long-term safety.
Plenty of practitioners now offer hormone replacement therapy, but not all of them have the specialized training required to design a truly personalized, safe, and effective protocol. Your health deserves an expert who lives and breathes this science, not a generalist who treats it as a side service.
The real specialists are committed to evidence-based care. That means they rely on rigorous testing and continuous monitoring—not guesswork. They understand the intricate nuances of hormonal pathways and can craft a plan that aligns precisely with your unique biochemistry.
Vetting Your Potential Doctor
When you meet with a potential physician, you’re not just a patient; you’re the interviewer. It’s absolutely essential to ask pointed questions to gauge their expertise and philosophy. Your goal is to find a partner in health, someone who sees you, not just another file.
Here are the critical questions to get you started:
- What are your credentials and specific training in hormone therapy? You’re looking for board certifications and fellowship training in fields like endocrinology, metabolic health, or age management medicine.
- What is your approach to diagnostic testing and ongoing monitoring? A top doctor will insist on a comprehensive initial lab panel and regular follow-ups to fine-tune your treatment. There’s no room for a “set it and forget it” mentality.
- How do you personalize treatment plans? Their answer should be a detailed discussion about your biomarkers, lifestyle, symptoms, and specific goals—not a one-size-fits-all protocol.
- Which delivery methods and hormone types do you prefer and why? This question reveals their knowledge of modern options like transdermal creams, injections, and bioidentical hormones. You can learn more by reading our guide to finding the right endocrinologist and metabolism expert.
The process with a true specialist should follow a clear, data-driven pathway. It’s never random.
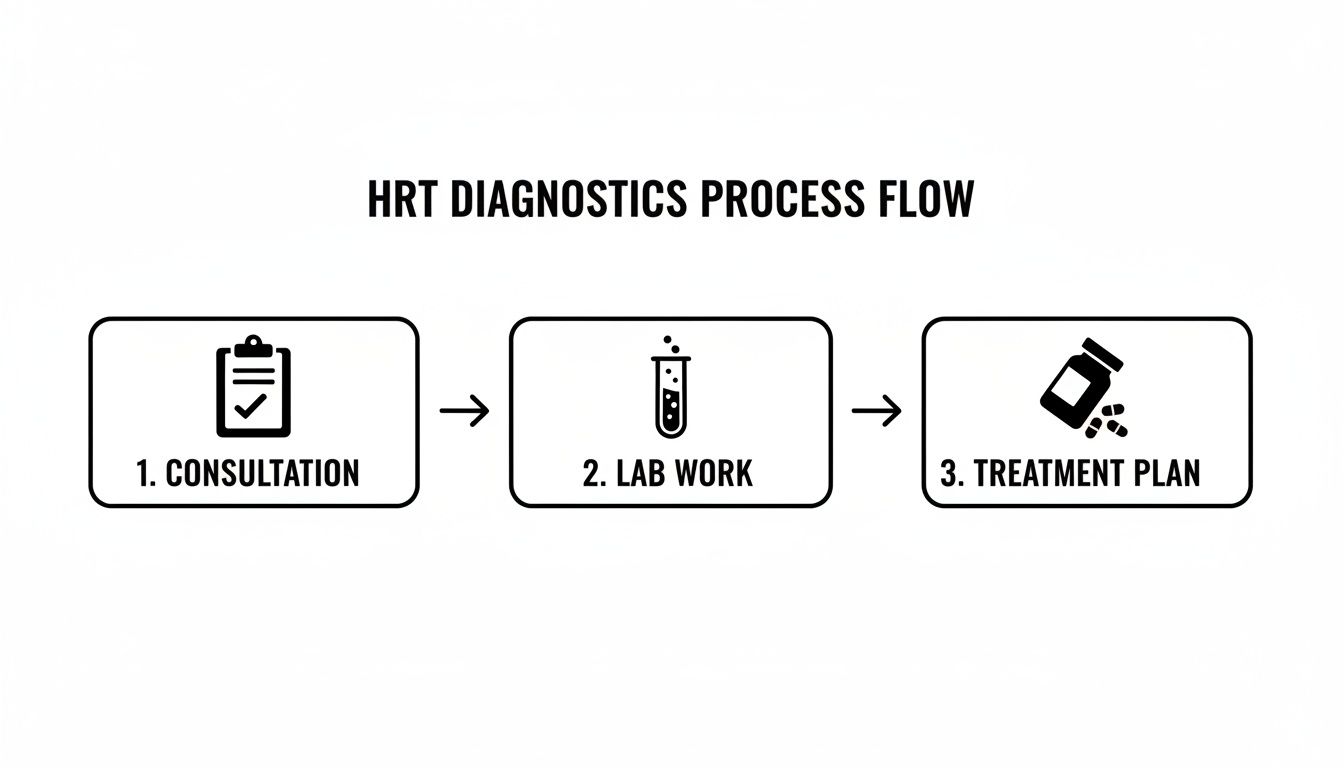
As this shows, it all begins with a deep-dive consultation. That informs the comprehensive lab work, which then provides the data needed to build your unique treatment protocol.
Simplifying Your Search with a Vetted Network
Finding this level of expertise can feel like searching for a needle in a haystack. That’s where a curated network like Haute MD becomes invaluable.
Haute MD removes the uncertainty by pre-vetting physicians for their credentials, patient outcomes, and commitment to cutting-edge, evidence-based care. This ensures you’re connected directly with elite specialists in longevity and hormone therapy who meet the absolute highest standards.
The healthcare ecosystem in North America, which accounted for 52.4% of the global HRT market in 2023, is sophisticated enough to support this advanced level of care. For discerning patients, this means access to concierge-level physicians who use remote monitoring and virtual follow-ups, making geography irrelevant when you want to connect with the best. This approach is what’s driving major trends in the global HRT market. Platforms like Haute MD leverage this powerful network to pair top-tier doctors with patients seeking superior care, no matter where they are.
Common Questions About Hormone Replacement Therapy
Stepping into the world of hormone replacement therapy can feel like navigating a maze. There’s a ton of information out there—some of it is great, and some of it is dangerously outdated. Getting clear, straightforward answers is the only way to make a smart decision about your health.
Here, we’ll cut through the noise and tackle the most common questions we hear, providing the kind of evidence-based insight you should demand from any expert.
Are Bioidentical Hormones Safer Than Synthetic Hormones?
This is easily one of the most important questions patients ask. Many people hear “bioidentical” and automatically assume it means safer or more natural, but the truth is a lot more nuanced than that.
Bioidentical hormones are, by definition, molecularly identical to the ones your body makes. That’s a good thing. However, the real safety of any hormone therapy hinges on three other, more critical factors:
- The Delivery Method: How a hormone gets into your system is a massive deal. For instance, estrogen delivered through the skin (transdermally) via a patch or cream carries a significantly lower risk of blood clots than oral estrogen pills. This is true whether the estrogen is bioidentical or not.
- The Dosage: True safety lies in using the lowest effective dose that gets the job done. A world-class physician will always start low and make precise adjustments based on your symptoms and lab work. It’s about finesse, not brute force.
- Personalization: The safest protocol is the one built specifically for you—your unique biology, your risk factors, and your medical history.
A skilled physician doesn’t just rely on the “bioidentical” label. They build a complete safety strategy around you, choosing the right hormone, the right dose, and the best delivery system for your individual needs.
How Long Until I Feel the Effects of HRT?
The timeline for feeling the benefits of HRT is different for everyone and depends on what symptoms you’re trying to fix. Think of it as a gradual restoration, not an overnight miracle.
Some of the most disruptive symptoms often improve surprisingly fast. Many people report that night sweats and hot flashes calm down within just a few weeks. That alone leads to better sleep, which has an immediate ripple effect on your mood and energy.
Other benefits, however, take a bit more time to fully emerge as your body recalibrates its new normal.
- 1-3 Months: This is often when people start noticing a sharper mind, a more stable mood, and more consistent energy throughout the day. The brain fog starts to lift.
- 3-6 Months: Physical changes tend to become more obvious in this window. You might see improvements in skin quality, muscle tone, or body composition as your metabolism finds its footing again.
Your doctor will be your partner through this initial phase, monitoring your progress and fine-tuning your protocol to make sure you’re heading toward your goals safely and efficiently.
What Is the Difference Between HRT and BHRT?
This one trips a lot of people up, but the distinction is actually pretty simple.
Hormone Replacement Therapy (HRT) is the big-picture medical term. It’s the umbrella that covers any treatment designed to replace or supplement hormones.
Bioidentical Hormone Replacement Therapy (BHRT) is a specific type of HRT. It’s a subcategory that uses only hormones that are chemically identical to what your body produces on its own.
An easy analogy: “HRT” is like the general category of “cars.” “BHRT” is a specific type, like “electric cars.” All BHRT is HRT, but not all HRT is bioidentical. The right choice for you has nothing to do with marketing terms and everything to do with your body, your goals, and your doctor’s expert guidance.
Can I Use HRT with a Family History of Cancer?
This is a critical conversation, and it demands a highly personalized risk assessment with a true specialist. A family history of hormone-sensitive cancers, like breast or ovarian cancer, doesn’t automatically rule out HRT, but it absolutely requires a more cautious and strategic plan.
A top-tier physician will dive deep into your personal and family medical history. This evaluation might involve:
- Suggesting genetic screening to see if you carry any predisposing markers.
- Choosing lower-risk delivery methods, like transdermal (skin-based) or localized hormones.
- Creating a plan for more rigorous and frequent monitoring, including regular imaging.
In these situations, the partnership you have with your physician is everything. You need an expert who can weigh the intricate risks and benefits and co-create a plan you feel confident in.
Finding a physician with the expertise to navigate these complexities is the most important step in your journey. Haute MD connects you with a curated network of the nation’s top, pre-vetted specialists in hormone optimization and longevity medicine, ensuring you receive the highest standard of personalized care. Discover a trusted expert who can design a safe and effective plan for you.

