
Figuring out your optimal testosterone levels by age isn’t about chasing some universal magic number. It’s about aligning your hormonal health with your own goals for vitality, drive, and performance. Standard lab reports give you a “normal” range, but true optimization often means aiming for the upper end of that spectrum, especially for men in their 20s (700-1,000 ng/dL) and 30s (600-900 ng/dL).
This guide will cut through the noise of “average” and give you a clear framework for what optimized T levels really look like at every stage of a man’s life.
Charting Your Hormonal Blueprint
Getting a handle on your testosterone levels is the first real step toward taking control of your long-term health, energy, and mental sharpness. The key is understanding the massive difference between what’s considered “normal” and what’s truly optimal.
Standard lab ranges are incredibly broad because they’re based on a general population that includes plenty of people in suboptimal health. For high-achievers, just being “not deficient” is a pretty low bar. The real goal is to operate at your absolute peak potential.
This means aiming for levels that support:
- Sustained Energy and Drive: The kind you need to power through demanding workdays and still have gas in the tank for intense training.
- Mental Clarity and Focus: Maintaining that sharp cognitive function and competitive edge that sets you apart.
- Physical Strength and Body Composition: The ability to build and hold onto lean muscle while keeping body fat in check.
This chart gives you a quick visual of how testosterone levels naturally shift over a man’s life, showing the peak in the 20s and the steady decline that follows.
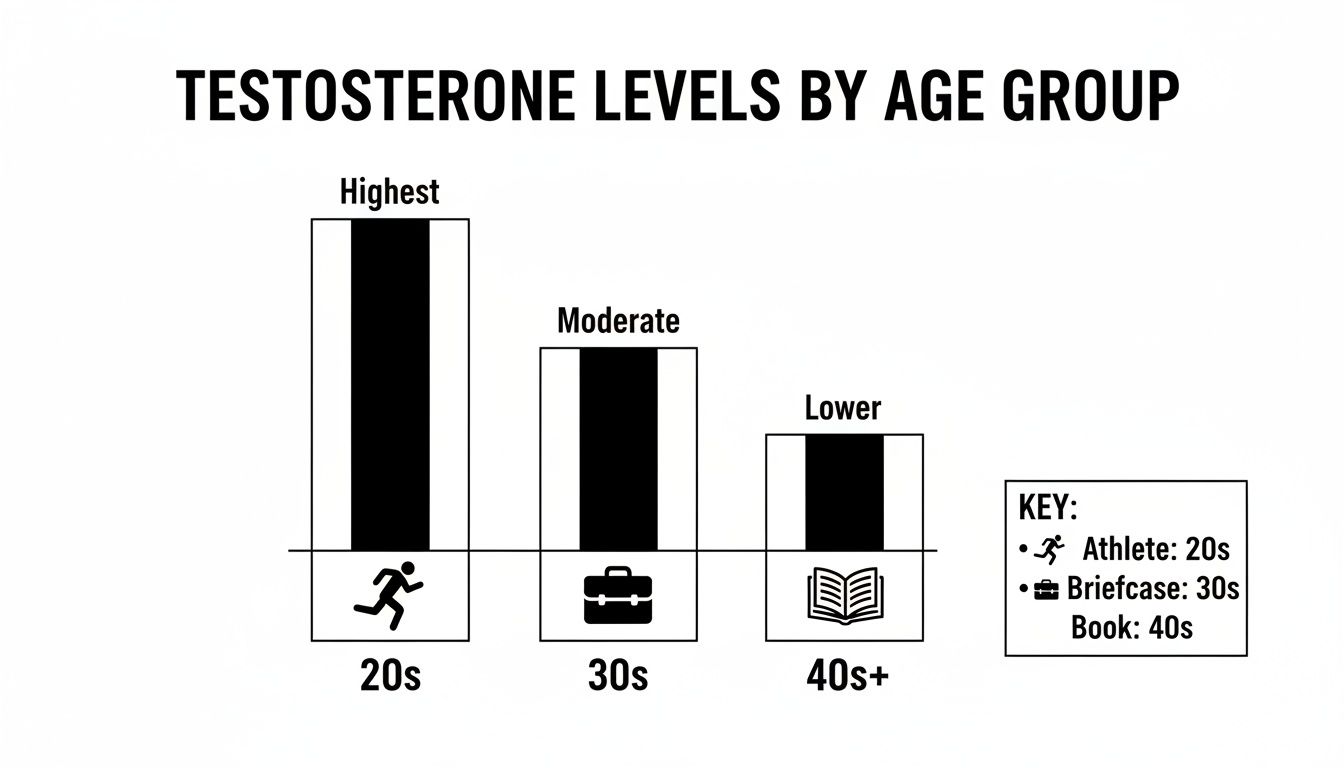
You can see the natural hormonal curve right there—the highest potential in your youth, a steady and strong level in your 30s, and a more noticeable drop-off as you hit your 40s and beyond.
A Quick Guide to Testosterone Levels by Age
To make this more concrete, it’s helpful to see the wide “average” lab ranges next to the “optimal” targets that specialists in performance medicine and longevity actually shoot for. Think of these numbers as the starting point for a productive conversation with a qualified doctor.
Key Distinction: The “average” range just means you fall within a statistical norm—a norm that, by the way, has been sliding downward for decades. “Optimal,” on the other hand, refers to the level required to feel and perform your best, without the nagging symptoms of a hormonal imbalance.
Here’s a quick-reference table summarizing total testosterone ranges in nanograms per deciliter (ng/dL), giving you a clear comparison for different stages of life.
Quick Guide to Total Testosterone Levels by Age (ng/dL)
| Age Group (Years) | Average Total Testosterone Range (ng/dL) | Optimal Total Testosterone Range (ng/dL) |
|---|---|---|
| 20–29 | 400–600 | 700–1,000 |
| 30–39 | 350–500 | 600–900 |
| 40–49 | 250–900 | 500–800 |
| 50+ | 200–800 | 450–750 |
Remember, these optimal ranges aren’t rigid rules; they’re strategic goals. Your ideal number will always depend on personal factors like your genetics, lifestyle, and any symptoms you’re experiencing. This data is here to empower you, so you can have a much more informed discussion about what your personal health objectives should be.
Understanding Your Complete Hormone Picture
A single number on a lab report rarely tells the whole story of your hormonal health. While total testosterone is the most common number people look at, it’s just the headline. To really understand what’s going on inside your body and how it’s affecting your performance, you have to dig deeper into the difference between total, free, and bioavailable testosterone.
Think of your total testosterone as your entire financial net worth. It’s a big, impressive number that includes all your assets—cash, investments, real estate, the works. But how much of that can you actually spend today to buy groceries or fill up your car? Not much of it.
This distinction is absolutely critical for figuring out your true hormonal status and what your optimal testosterone levels should be for your age.
The Difference Between Bound and Free Testosterone
Most of the testosterone floating around in your bloodstream isn’t actually available for your body to use right away. A huge chunk of it, usually 40% to 60%, is tightly latched onto a protein called Sex Hormone-Binding Globulin (SHBG).
You can think of SHBG as a secure vault. Once testosterone is locked inside, your cells can’t get to it. It’s part of your total “wealth,” but it’s not liquid cash. It can’t help you build muscle, boost your energy, or sharpen your focus.
Another big piece of your testosterone is loosely attached to a different protein, albumin. Because this bond is much weaker, your body can easily break it apart to access the hormone when it needs it.
That leaves a tiny, but incredibly powerful, fraction that is completely unbound and ready for action.
- Free Testosterone: This is your “cash on hand.” It only makes up about 1-4% of your total testosterone, but it’s the form that does all the heavy lifting. It’s ready to jump into your cells and carry out all the vital jobs we associate with testosterone.
- Bioavailable Testosterone: This is the total amount of hormone your body can actually use. It includes your free testosterone plus the testosterone that’s weakly bound to albumin.
This is why two men could have the exact same total testosterone level of 600 ng/dL and feel completely different. If one has high SHBG, his free testosterone might be scraping the bottom of the barrel, leaving him with all the classic symptoms of deficiency. The other guy, with lower SHBG, could feel fantastic. Just looking at that total number is often incredibly misleading.

Why SHBG Levels Matter So Much
Getting a handle on your SHBG level is crucial because it’s the gatekeeper that controls how much of your testosterone is actually usable. A number of factors can influence SHBG, effectively tightening or loosening its grip on your hormones.
Things that can drive SHBG up (and therefore push free testosterone down) include:
- Aging: It’s a simple fact of life—SHBG levels naturally tend to climb as men get older.
- Certain medical conditions: Things like liver disease and an overactive thyroid can send SHBG soaring.
- Diet: Very low-calorie or extremely low-fat diets have been shown to increase SHBG.
On the flip side, things like insulin resistance and obesity can sometimes lower SHBG. That might sound like a good thing, but it’s usually a sign of other serious metabolic problems.
A high total testosterone level with a high SHBG is like having a million dollars locked in a trust fund you can’t touch for 30 years. It’s technically yours, but it does you no good today. True hormonal optimization focuses on increasing the “cash on hand”—your free and bioavailable testosterone.
This more detailed view allows for a much smarter, more effective approach to your health. It helps explain why you might feel terrible even when your doctor says your total testosterone is “normal.”
For a deeper dive into this subject, you can explore detailed resources about hormone optimization and its role in longevity. Armed with this knowledge, you can have a far more productive conversation with your physician, moving beyond a single number to discuss what your lab results truly mean for your symptoms, performance, and overall well-being.
The Natural Ebb and Flow of Testosterone
Testosterone isn’t a static number on a lab report; it’s the driving force behind a man’s biological journey, marked by a powerful surge, a sustained peak, and a slow, predictable decline. Understanding this natural lifecycle is the first step toward moving beyond “normal” ranges and into true optimization.
Think of it like an athlete’s career arc—an explosive rise in the early years, a period of peak performance, followed by a gradual tapering that requires smart management to stay in the game.
This journey kicks off with one of the most dramatic hormonal shifts in biology. After remaining low through childhood, testosterone production ignites at puberty. This exponential increase is what builds the foundational muscle, bone density, and vitality that define a man’s physical prime.
The Peak Years of Hormonal Vigor
The late teens and twenties are the pinnacle of a man’s natural testosterone output. Levels are at their highest, fueling peak physical strength, rapid muscle recovery, relentless ambition, and a powerful libido. This is the biological engine that drives competitive success, whether on the field or in the boardroom.
For men in this age group, “optimal” isn’t about scraping by within the reference range—it’s about operating at the upper end of it. This is the body’s natural state of high performance, and maintaining these levels is key to maximizing potential during these formative years.
As men move into their thirties, testosterone levels begin a slow but steady decline. While still robust, the effortless energy and bounce-back recovery of the early twenties might start to feel a bit more distant. This is often the first time men notice subtle shifts that get them thinking about their long-term health and performance.
Navigating the Gradual Decline
By the time a man hits his forties and fifties, this hormonal decline becomes much more noticeable. The data is clear: after age 30, total testosterone can drop by roughly 1% per year. That might not sound like much, but over decades, it adds up, contributing to many common age-related complaints.
This downward trend often shows up in a few key ways:
- It gets harder to maintain muscle mass, even with a consistent training schedule.
- Metabolism noticeably slows down, and stubborn abdominal fat starts to accumulate.
- That “mental edge” or cognitive sharpness isn’t quite what it used to be.
- Energy reserves feel lower, and it takes longer to recover from physical exertion.
It’s this slow, creeping decline that makes understanding the entire hormonal timeline so critical. Recognizing these changes not as an inevitable part of aging but as a manageable biological process is the first step toward taking control.
The goal isn’t to fight aging; it’s to manage it intelligently. By understanding the expected hormonal shifts decade by decade, you can build a sophisticated, long-term strategy to mitigate decline and sustain a high quality of life for years to come.
This perspective shifts the conversation from a passive question—”Are my levels normal?”—to a much more powerful one: “Are my levels optimized for my goals and my age?”
The Full Lifetime Spectrum
To really grasp the scale of this journey, it helps to see the numbers mapped out from the very beginning. The fluctuations start right after birth, settle down in childhood, and then explode during the teenage years.
Data on typical hormone ranges shows a male infant’s testosterone can be between 75-400 ng/dL, dropping to just 7-130 ng/dL by age 10. Puberty flips the switch, with early teens (12-13) hitting 7-800 ng/dL, and late teens (17-18) peaking anywhere from 300-1,200 ng/dL. From adulthood on, the widely accepted range is 300-1,000 ng/dL. You can explore these typical age-related testosterone ranges to see the full lifecycle.
This lifelong arc provides the essential backdrop for any meaningful discussion about optimizing your health. Knowing where you are on this timeline empowers you to have a much more informed, strategic conversation with a specialist about maintaining your peak performance for the long haul.
Why ‘Normal’ Testosterone Is No Longer Normal
The standard lab ranges for testosterone are a trap. They’re based on population averages, but what happens when the entire population’s average has been plummeting for decades? This isn’t a hypothetical—it’s the reality we’re living in.
A 30-year-old man today likely has significantly lower testosterone than a man of the same age just a few generations ago. This means that hitting a “normal” number on your lab report might actually place you in a category that would have been considered deficient by historical standards.
For ambitious professionals and athletes who demand peak physical and cognitive output, this trend is a massive blind spot in the health puzzle. Simply being average in an increasingly unhealthy population isn’t a strategy for success. The goal isn’t to be “normal”; it’s to achieve the robust, historically healthy benchmarks that truly define optimization.
The Modern Assault on Male Hormones
This generational decline isn’t some mystery. It’s the predictable outcome of a profound shift in our environment and lifestyles—a perfect storm of factors conspiring to crush male hormones.
Chronic, unrelenting stress is at the top of the list. The high-stakes, always-on culture of modern professional life keeps cortisol, the primary stress hormone, perpetually elevated. Cortisol and testosterone exist in a ruthless seesaw relationship; when one is high, the other is forced low. Your body simply cannot be in a state of “fight or flight” and “rest and build” at the same time.
Then there’s sleep—or the lack of it. Your body’s testosterone factory runs the night shift, with peak production happening during deep sleep. Consistently getting less than seven hours of quality rest can slash testosterone production, in some cases by as much as 15%.
Environmental and Dietary Culprits
Beyond the daily grind, our environment and food supply are laced with hormonal landmines. The modern diet, packed with processed foods, sugar, and industrial fats, fuels inflammation and obesity—two conditions that directly tank testosterone.
Worse, we are swimming in a sea of chemicals known as endocrine disruptors. These are synthetic compounds lurking in everything from plastics and pesticides to soaps and lotions. They mimic, block, or otherwise scramble the hormonal signals your body relies on for optimal testosterone production.
You’re exposed to them every day from sources like:
- Plastics: Chemicals like BPA and phthalates leach from food containers and water bottles.
- Pesticides: Residues on non-organic produce can throw your hormones out of whack.
- Industrial Chemicals: Compounds used in manufacturing and common household products are now widespread in our environment.
The cumulative effect of these modern pressures means that achieving optimal testosterone is no longer a given. It requires a deliberate, strategic effort, even for young, otherwise healthy men.
This isn’t just theory; the data is alarming. Research consistently confirms a steady, troubling decline in testosterone levels among young American men, leading some experts to warn of a “testosterone deficiency epidemic.” A 2022 study of nearly 1,500 men aged 20-44 found a shockingly low mean total testosterone of just 466 ng/dL, with the cutoff for “low T” set as low as 350 ng/dL for men in their early 40s. Discover more about this steady decrease in testosterone among U.S. men.
This data drives home a critical point: your personal optimal level is very likely far higher than the population’s new normal. Understanding this distinction is the first step toward reclaiming your hormonal edge and truly priming your body for peak performance.
How to Interpret Your Lab Results Like an Expert
Getting your lab report can feel like someone handed you a page of cryptic code. But learning to read these numbers is the first step in having a real, strategic conversation with your doctor about your health, energy, and performance.
The first rule is simple: timing is everything. Your testosterone production isn’t a flat line; it follows a natural daily rhythm, peaking in the early morning. To capture this peak accurately, your blood draw must be scheduled between 7 AM and 10 AM.
If you test in the afternoon, you’re almost guaranteed to get a falsely low number, which can lead to a lot of confusion or even a wrong diagnosis. Consistency matters, too. For any follow-up tests, always aim for the same time and under similar conditions, like after a normal night’s sleep.
Moving Beyond the Numbers
Here’s the most important thing to understand: your lab results are a critical piece of the puzzle, but they are not the whole picture. Two men can have the exact same testosterone level on paper and live in completely different realities. Why? Because numbers don’t have symptoms, but people do.
Truly effective hormone optimization isn’t about chasing a number. It’s a partnership where your real-world experience is just as valuable as any clinical data. Your doctor should be looking at your lab work through the lens of how you actually feel day-to-day.
Think of it like this:
- The Data: Your lab report gives the objective facts—your total, free, and bioavailable testosterone, plus SHBG and other key markers.
- The Experience: You provide the subjective context—the fatigue, brain fog, low motivation, disappearing libido, or stalled workout recovery.
A total testosterone level of 450 ng/dL might be flagged as “normal” by the lab’s reference range. But if you’re battling all the classic symptoms of low T, that number clearly isn’t optimal for you. An expert physician treats the patient, not just the lab slip. They connect the dots between your hormonal profile and your personal health goals.
The Art and Science of Interpretation
Reading a hormone panel is both an art and a science. A skilled specialist doesn’t just look at one number in isolation; they see the relationships between all the values to understand the complete story. For instance, a man could have high total testosterone, but if his SHBG is sky-high, it could be binding up all that testosterone, leaving him with low free T and significant symptoms.
Your lab results are the “what,” but your symptoms are the “so what.” True optimization happens when a physician combines both to create a personalized strategy that restores your vitality and performance, regardless of what a generic reference range says is “normal.”
This mindset is the core of a health strategy that actually works. It ditches the one-size-fits-all model and hones in on what’s needed to get you feeling and performing at your absolute best. This principle of using data to create a personalized plan isn’t unique to hormones. To see how specialists apply this to other areas, check out our guide on metabolic testing for weight loss, which is built on the same foundation of deep, personalized analysis.
Ultimately, your lab results are just the starting point of a dialogue. They provide the map, but you and your doctor have to chart the course together. When you understand the right way to get tested and recognize the immense value of your own experience, you can step into that conversation not just as a patient, but as an informed expert on your own health.
Achieving and Maintaining Optimal Levels
Once you have the data—the clear picture of where your testosterone levels actually are—the real work begins. Moving from insight to action is what separates the serious from the merely curious. Knowing your numbers is the starting point; actively managing them is how you sustain peak performance for the long haul.
This isn’t about finding a quick fix. It’s about integrating hormonal health into your overall strategy for success with a two-pronged approach: mastering powerful lifestyle modifications and, when necessary, leveraging advanced medical support.

Building Your Foundation with Lifestyle Strategies
Before even thinking about medical interventions, you have to master the fundamentals. Think of these strategies as the non-negotiable bedrock of hormonal health. They work by sending powerful signals to your body that it’s safe, strong, and primed to thrive—which directly supports robust testosterone production.
Here are the absolute pillars:
- Intelligent Resistance Training: Nothing signals your body to produce more testosterone quite like lifting heavy weights. The key is to focus on big, compound movements like squats, deadlifts, and bench presses that recruit massive amounts of muscle and trigger a significant hormonal cascade. Consistency beats sporadic intensity every time; 3-4 sessions per week is the sweet spot.
- Strategic Nutrition: Your diet is literally the raw material for your hormones. You need to prioritize healthy fats from sources like avocados, nuts, and olive oil, alongside high-quality protein and a ton of micronutrient-dense vegetables. Just as important is what you don’t eat. Cut out the testosterone killers—processed sugar and excessive alcohol—which fuel inflammation and throw your hormonal balance into chaos.
- Prioritizing Restorative Sleep: This is where the magic happens. Your body produces the vast majority of its daily testosterone while you’re in deep sleep. Consistently getting fewer than 7 hours a night will crush your production. Get disciplined. Set a non-negotiable bedtime, kill all screens an hour beforehand, and make your bedroom a dark, cool, quiet sanctuary.
- Mastering Stress Management: Chronic stress is the arch-nemesis of healthy testosterone. When the stress hormone cortisol is constantly elevated, it directly suppresses testosterone production. You have to actively fight back. Build stress-reduction tactics into your daily routine, whether it’s meditation, simple deep breathing exercises, or just taking short walks outside to disconnect.
Exploring Medical Interventions with a Specialist
For some men, even perfect lifestyle execution isn’t enough to get back to optimal. This is especially true if you’re dealing with a significant, clinically diagnosed deficiency. This is where medical interventions, guided by a board-certified specialist, become an incredibly powerful tool for restoring vitality.
The gold standard here is Testosterone Replacement Therapy (TRT). The goal of TRT isn’t to push your levels into some superhuman range; it’s about restoring your testosterone to the optimal levels you likely had in your prime, wiping out symptoms and dramatically improving your quality of life.
TRT is a precision medical protocol, not a casual supplement. It requires a formal diagnosis of hypogonadism (clinically low testosterone) and must be managed by an experienced physician who can monitor your progress and ensure your health markers remain in a safe and healthy range.
It’s a biological reality that testosterone declines by about 1% per year after age 35. A man aged 20-39 might have an average total testosterone range of 300–1000 ng/dL, but by the time he’s 50-59, that range can drop to 215–878 ng/dL. Advanced medical interventions can halt and even reverse this decline.
This is where working with the right expert is everything. Top endocrinologists and men’s health specialists use advanced testing to tailor TRT protocols, often restoring levels to the upper end of youthful ranges—like 800-1000 ng/dL—to support executive health and high performance.
Several methods exist for administering TRT, and a specialist will help you find the best fit for your body and lifestyle. You can learn more about the different options for Testosterone Replacement Therapy in our guide.
Let me be clear: working with a board-certified specialist is non-negotiable. A true expert will run a full hormone panel, listen to your symptoms, understand your goals, and build a personalized plan that looks far beyond a single testosterone number. This is how you ensure your journey to optimization is safe, effective, and perfectly aligned with your long-term health.
Your Questions, Answered
When you start digging into hormone optimization, a lot of practical questions come up. Here are some straight answers to the most common things men ask when they start thinking about their testosterone levels.
What Are the Real Symptoms of Low Testosterone?
It’s about a lot more than just a dip in your sex drive. One of the biggest tells is a deep, persistent fatigue that sleep just doesn’t seem to fix. You might also notice your ambition and competitive edge fading, or a constant mental haze that people often call ‘brain fog.’
Other big red flags are losing muscle mass even though you’re still hitting the gym, gaining body fat (especially around your midsection), and finding yourself more irritable or just feeling down. If a few of these sound familiar, it’s a strong signal that you need to get comprehensive blood work done with a specialist.
How Do I Find the Right Doctor for This?
This is the most critical step. You can’t just go to any doctor; you need a genuine expert to get the best results safely. Look for a board-certified physician who specializes in Endocrinology, Urology, or the fields of Longevity and Age Management Medicine. These are the doctors who live and breathe this stuff.
A true specialist won’t just glance at your total testosterone and call it a day. They’ll order a complete panel of biomarkers and, more importantly, they’ll listen to you. Their goal isn’t just to nudge you into some generic “normal” lab range—it’s to partner with you, optimizing your health based on your specific symptoms and what you want to achieve.
Is TRT Safe for the Long Haul?
When it’s prescribed for a diagnosed deficiency and managed by a skilled physician, Testosterone Replacement Therapy (TRT) is considered a very safe and effective long-term treatment. A proper, professional protocol isn’t a “set it and forget it” approach; it involves regular, detailed monitoring of your key health markers.
This means your doctor will be keeping a close eye on your testosterone levels, estradiol, and red blood cell counts to make sure everything stays in a healthy, optimal zone. The whole point is to restore your vitality without compromising your long-term health, which is why the expertise of your doctor makes all the difference. The right physician ensures your journey to optimize your testosterone is both successful and safe.
Finding a physician who operates at this level is the single most important decision you’ll make for your health. Haute MD has already done the legwork, creating a curated network of the nation’s top, board-certified specialists in hormone optimization and executive health. Connect with a vetted expert dedicated to precision, performance, and proactive care by visiting the Haute MD Network.

