Knee surgery can feel like a monumental event on the horizon, but the truth is, a successful recovery starts long before you ever see the inside of an operating room. The weeks leading up to your procedure are a critical window—an opportunity to get your body, mind, and home ready for a smooth, swift healing process.
This isn’t just about waiting for the date to arrive. It’s about proactively taking control of every variable you can, from your physical conditioning to your logistical planning, to set the stage for the best possible outcome.
Your Pre-Surgery Timeline: A Week-by-Week Guide
Think of the time before your surgery not as a waiting period, but as an active preparation phase. A structured timeline helps break down what can feel like an overwhelming process into manageable, bite-sized tasks. It ensures nothing is left to chance, preventing that last-minute scramble and stress.
This strategic approach is what separates a good recovery from a great one. You’ll methodically address medical appointments, lifestyle tweaks, and home arrangements, building a solid foundation for success.
Key Milestones on Your Path to Surgery
As your surgery date gets closer, your focus will naturally shift. You’ll move from big-picture health optimization to the finer details of preparing for your hospital stay and a comfortable return home.
- 6-8 Weeks Out: The Big Picture. This is your planning phase. It’s the time to lock in medical clearances, meet with any necessary specialists, and begin a gentle prehabilitation (prehab) exercise routine.
- 2-4 Weeks Out: Getting Your House in Order. Now the focus turns to practicalities. You’ll start modifying your home for easy navigation post-op, line up friends or family to help out, and make any nutritional adjustments your team recommends.
- 1 Week Out: Final Preparations. The last few days are all about finalizing the details. This is when you’ll pack your hospital bag, confirm your transportation, and get yourself mentally squared away for the procedure.
A visual guide can help keep all these moving parts organized.
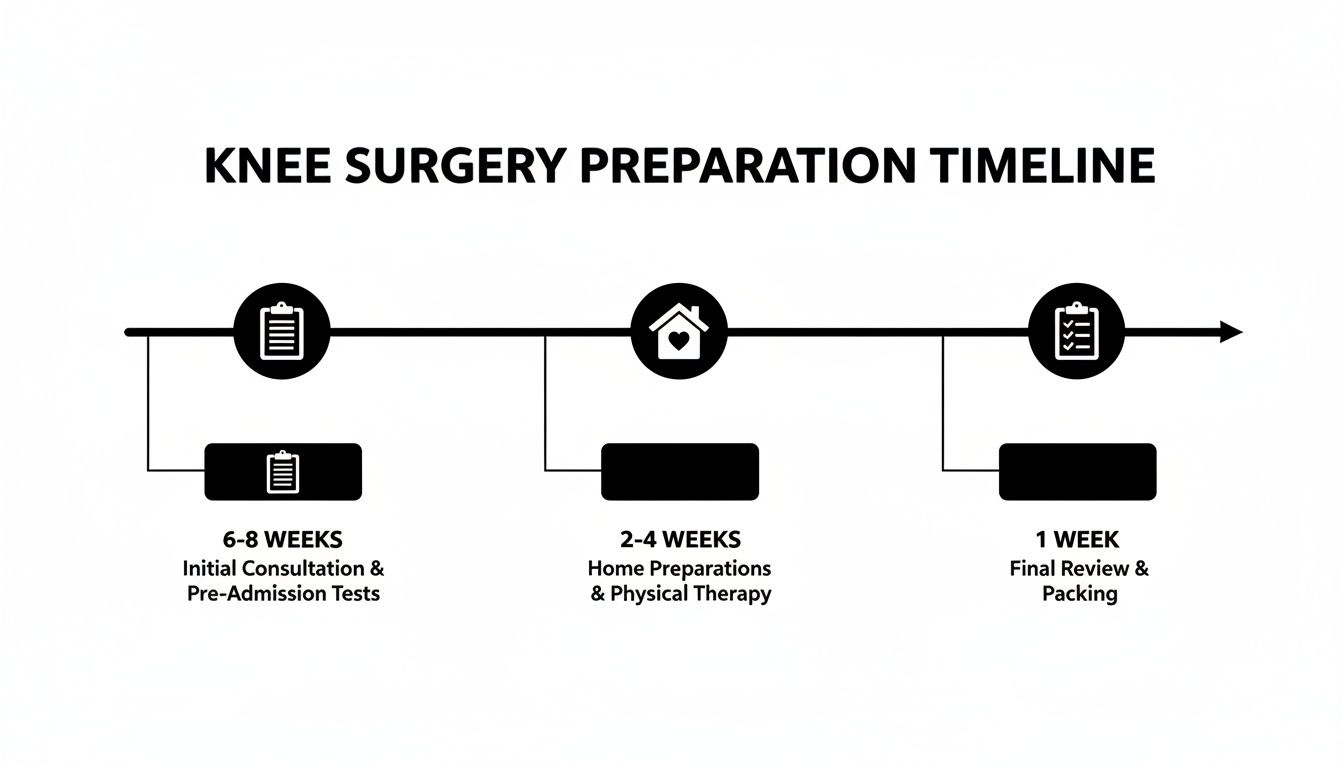
This kind of roadmap breaks the preoperative period into clear, distinct stages, helping you prioritize what needs to be done and when.
This preparatory work is far from trivial. A staggering 3.6 million knee replacements were performed worldwide in 2023, and research shows that inadequate preparation can contribute to complications in up to 15% of cases. The data is compelling: smokers have a 55% higher risk of surgical site infections, while patients who lose just 10% of their excess body weight before surgery can see mobility outcomes improve by as much as 50% six months later.
To help you visualize this, here’s a quick overview of how your priorities will shift as your surgery date approaches.
Pre-Surgery Preparation Timeline At a Glance
| Timeframe Before Surgery | Medical & Lifestyle Focus | Physical & Home Preparation |
|---|---|---|
| 6-8 Weeks | Schedule all pre-op appointments & medical clearances. Begin smoking cessation and alcohol reduction. | Start your prehab exercise program. Arrange for any necessary time off work. |
| 4 Weeks | Finalize medication plan with your surgeon. Focus on a nutrient-dense, anti-inflammatory diet. | Modify your home for safety & accessibility. Arrange for post-op care and support. |
| 2 Weeks | Confirm all pre-op testing is complete. Increase hydration and prioritize quality sleep. | Practice using crutches or a walker. Begin organizing items for your recovery space. |
| 1 Week | Attend your final pre-op appointment. Follow all pre-surgery instructions regarding food, drink, & meds. | Pack your hospital bag. Confirm your ride to and from the hospital. |
This table provides a simple, at-a-glance checklist to ensure you’re hitting the key milestones at the right time, making the entire process feel more controlled and less chaotic.
Think of this preoperative period as an investment. The work you put in now directly influences the speed and quality of your recovery, paying dividends in your future mobility and comfort.
Ultimately, your surgeon is your most important partner in this journey. Clear, open communication is absolutely essential. We recommend keeping a running list of questions for every appointment. Our guide on the crucial questions to ask an orthopedic surgeon is a great resource to make sure you cover all your bases and feel completely confident in your care plan.
Fine-Tuning Your Health for Surgery
Think of the weeks leading up to your surgery as an athlete’s training camp. Your body is the engine, and the goal is to get it running in peak condition for a high-performance event. This isn’t just about getting medical clearance; it’s an active strategy to minimize complications and set the stage for a smoother, more predictable recovery.
Your surgical team will kick off a series of pre-operative evaluations to get a crystal-clear picture of your overall health. These are non-negotiable steps designed to flag and address any underlying issues before they have a chance to become problems.
Your Medical Optimization Checklist
You can expect a thorough workup that gives your team a vital piece of the puzzle, ensuring your body is ready for both the stress of surgery and the demands of healing.
- Comprehensive Blood Work: This is the baseline. It screens for things like anemia, hidden infections, and clotting abnormalities that need to be addressed.
- Electrocardiogram (EKG): An EKG is standard procedure for assessing your heart’s health and rhythm, especially if you have a cardiac history or are over a certain age.
- Specialist Consultations: If you’re managing a chronic condition like heart disease, lung problems, or diabetes, you absolutely will need to get clearance from your specialist. They’ll work in concert with your surgeon to create a unified game plan.
This whole process ensures every member of your medical team is on the same page and that any potential risks are managed proactively, not reactively.
Managing Medications and Supplements
One of the most critical aspects of preparing for knee surgery is managing what you put into your body. So many common medications and even “natural” supplements can interfere with anesthesia, blood clotting, or the healing process itself.
Your surgeon will provide a detailed list of what to stop and when, but it’s on you to be completely transparent about everything you take.
Common culprits that often need to be paused include:
- Blood Thinners: Medications like aspirin, warfarin (Coumadin), and clopidrel (Plavix) must be managed with precision to prevent excessive bleeding during the procedure.
- Anti-Inflammatory Drugs (NSAIDs): This includes both prescription and over-the-counter NSAIDs like ibuprofen, which can affect clotting.
- Certain Supplements: Vitamin E, fish oil, garlic, and ginkgo biloba are well-known for their blood-thinning properties and are usually stopped one to two weeks before surgery.
You must have this conversation with your surgeon. Never stop taking a prescribed medication without explicit instructions from your doctor. The objective is to create the safest possible internal environment for your procedure.
Optimizing your health isn’t a passive waiting game. It’s an active partnership between you and your medical team. Your diligence in managing chronic conditions, medications, and lifestyle choices directly impacts your surgical outcome.
Addressing Hidden Health Risks
Beyond the standard medical workup, there are a few often-overlooked areas that can have a massive impact on your success. Tackling these “hidden” risks is a hallmark of truly elite-level preparation.
For instance, managing blood sugar is absolutely critical, especially for patients with diabetes. Uncontrolled glucose levels can severely impair your body’s ability to fight off infection. In fact, pre-operative blood sugar levels above 180 mg/dL have been shown to double the risk of post-surgical infection. You can get ahead of this by learning how to improve your metabolic health.
Similarly, your oral health is directly linked to your joint health—something many people find surprising. A pre-surgical dental check-up is non-negotiable. Untreated infections in your mouth are a shocking contributor to as many as 20% of prosthetic joint infections. Any necessary dental work must be completed two to four weeks before your knee surgery.
And while only about 5-10% of patients require a blood transfusion, discussing the possibility of pre-donating your own blood (an autologous transfusion) can be a wise move. This simple step can cut the associated risks by 50%.
Building Strength Before Your Surgery
The work you put in before your knee surgery has a direct and profound impact on how quickly and how well you recover. Think of this period as prehabilitation, or “prehab.” It’s not about crushing it in the gym; it’s a strategic approach to building up the muscles around the knee, creating a powerful, stable support system for your new joint.
Going into surgery with stronger, more resilient muscles means you’ll regain function faster on the other side. This isn’t just theory—study after study shows that patients who commit to prehab experience less post-operative pain, require less help from others, and hit their recovery milestones well ahead of schedule. You’re essentially preparing your body to handle the stress of the procedure and the demands of rehabilitation that follow.
The entire focus is on the key muscle groups that act as the scaffolding for your knee. By strengthening them now, you give yourself a massive head start on healing.
Targeting Key Muscles for a Faster Recovery
The goal here is simple: isolate and strengthen the muscles that will be doing the heavy lifting after your operation. If that support system is weak, your new joint is forced to work harder, leading to a much tougher recovery. While your physical therapist will design a specific program for you, it will almost certainly focus on three critical areas.
- Quadriceps: These muscles on the front of your thigh are absolutely crucial for straightening your leg and providing stability. Weak quads are a notorious problem after knee surgery, making it a top priority to build them up beforehand.
- Hamstrings: Located on the back of your thigh, these muscles help you bend your knee and control your movements. Strong hamstrings provide a critical counterbalance to the strength of your quads.
- Glutes: Your gluteal muscles are the powerhouse of your entire lower body. They stabilize your pelvis and, most importantly, take a significant amount of pressure off the knee joint—a huge advantage when you’re re-learning how to walk.
Simple, low-impact exercises are the cornerstone of a great prehab routine. Stationary cycling, for example, is fantastic for building quad strength without putting any undue stress on the joint. Other common movements include straight leg raises, glute bridges, and gentle hamstring curls, all designed to build resilience without causing pain.
Prehabilitation isn’t about pushing through pain. It’s about smart, consistent effort. The strength you build in the weeks before your surgery becomes the very foundation your entire recovery is built on.
Fueling Your Body for Optimal Healing
Just as vital as the physical conditioning is your nutritional strategy. The food you eat in the weeks leading up to surgery can dramatically impact your body’s ability to heal, manage inflammation, and fight off infection. Think of it as supplying your body with the premium raw materials it needs to repair itself.
A diet rich in high-quality protein is non-negotiable. Protein is the building block for tissue repair and for rebuilding muscle that is inevitably lost during the initial recovery. Make it a goal to include a lean protein source with every single meal.
Excellent sources of pre-surgery protein include:
- Grilled chicken or turkey breast
- Fish, especially fatty fish like salmon which also provides anti-inflammatory omega-3 fats
- Eggs and low-fat Greek yogurt
- Legumes, tofu, and quinoa for excellent plant-based options
On top of that, focusing on a diet packed with anti-inflammatory foods can help manage the post-operative swelling that everyone experiences. Load up on colorful fruits and vegetables, nuts, and seeds. Berries, leafy greens like spinach, and broccoli are particularly powerful.
Proper hydration is another simple yet critical piece of the puzzle. Staying well-hydrated helps transport all those vital nutrients to your cells, flushes out toxins, and can even improve your body’s response to anesthesia. Ditch the sugary drinks and excessive caffeine, and make a conscious effort to drink plenty of water all day long. Your preparation for surgery is just as much about what happens in the kitchen as it is in your prehab sessions.
Setting Up Your Recovery Environment
Your home should be a sanctuary for healing, not an obstacle course. Think of it this way: the preparations you make to your living space before surgery are just as critical as the physical prehab you perform.
When you transform your home into a safe, efficient recovery zone, you dramatically minimize the risk of falls—a significant concern post-op. It also cuts down on the physical and mental stress of just trying to get through the day with limited mobility. A well-prepared environment gives you back a sense of independence and lets you focus on the one thing that matters: your recovery.

Creating Safe Passageways
First things first: eliminate every single tripping hazard. Walk through your home with a critical eye, imagining you’re navigating it with a walker or crutches for the very first time. You’ll be surprised how your usual pathways suddenly present new challenges.
Start by securing or completely removing all throw rugs and area rugs. Tape down any electrical cords that run across the floor, or better yet, reroute them along the wall. Move the small stuff—ottomans, floor plants, decorative baskets—that could obstruct your path. Your goal is to create wide, clear lanes from your bed to the bathroom and kitchen.
Equipping Your Recovery Command Center
For the first week or two, you’ll want to minimize movement as much as possible, especially any trips up and down stairs. I always advise my patients to designate a “command center” on their main living floor. This will be your hub for rest, recovery, and just about everything else.
Set up a comfortable recliner or a sturdy chair with solid armrests you can use to push yourself up. Next to it, place a table with everything you’ll need within arm’s reach.
Here’s a checklist for your command center essentials:
- Medications: Keep your prescribed pain relievers and any other daily meds in a labeled organizer.
- Hydration and Snacks: A large water bottle with a straw is a game-changer. Add some simple, non-perishable snacks.
- Communication: Your phone, a long charging cable, and a physical list of important contact numbers.
- Entertainment: Books, a tablet, the TV remote, and headphones.
A “reacher” or “grabber” tool is an invaluable piece of gear for your command center. This inexpensive device will save you from the painful and difficult act of bending or stretching for dropped items. Trust me, you’ll use it constantly.
Fortifying the Bathroom for Safety
The bathroom is one of the highest-risk areas for falls after surgery. Between the slippery surfaces and the need to sit and stand, it’s a top priority for safety modifications.
First, install a shower chair or bench. Standing for a shower will be nearly impossible at first, and this provides a stable, secure place to sit. Next, place a non-slip mat both inside and outside the tub or shower.
Crucially, install temporary grab bars. Suction-cup models are easy to put up and can be placed exactly where you need them—one inside the shower and another near the toilet to help you stand up. A raised toilet seat with handles can also dramatically reduce the strain on your new knee.
Arranging Your Support System
Even with a perfectly prepared home, you are going to need help. Trying to manage everything alone isn’t just difficult; it’s a genuine risk to your recovery. Finalize your support plan well before you even head to the hospital.
This might mean having a family member or friend stay with you for the first few days. Alternatively, you can pre-arrange meal delivery services to handle cooking or hire a short-term caregiver for a few hours each day. Understanding the typical knee replacement surgery recovery timeline can help you game-plan how long you’ll need this elevated level of support. The key is to have this system locked in place before you leave for the hospital, ensuring a seamless and stress-free return home.
Your Surgical Day: A Step-by-Step Guide to a Calm, Confident Experience
The morning of your surgery is the final step in a journey of careful preparation. After weeks of getting your body and mind ready, this isn’t a day for last-minute stress. It’s a day to execute the plan. With the right mindset and a clear understanding of what’s ahead, you can walk into the hospital feeling focused and in control, ready to confidently hand the reins to your surgical team.
From the moment you check in, a well-practiced sequence of events begins. Knowing what to expect demystifies the process, transforming you from a passive patient into an active, engaged partner in your own care.

What to Expect When You Arrive
Your arrival time is precise for a reason. Once you’re there, you’ll move through a straightforward admissions process—have your ID and insurance card ready. The staff will run through a final verification: your identity, your scheduled procedure, and any known allergies. This is a critical safety check.
Soon after, you’ll be guided to a preoperative area. Here, you’ll change into a hospital gown, and a nurse will record your baseline vital signs. This is also when an IV line will likely be started in your arm, a routine step to deliver fluids and medication. It’s the first tangible step in preparing you for a smooth, safe surgery.
The Anesthesia Huddle: Your Final Pre-Op Conversation
Before you go to the operating room, you will have a crucial meeting with your anesthesiologist. This is the specialist responsible for your safety and comfort throughout the entire procedure. They’ll review your medical history, current medications, and any past experiences you’ve had with anesthesia.
Be completely transparent. This is the time to mention everything, including vitamins or supplements you’ve taken. They will confirm the plan—whether it’s general anesthesia, a spinal block, or a nerve block—and answer any lingering questions. This conversation ensures the anesthesia strategy is perfectly matched to your physiology.
Think of your interactions on surgery day as a final, critical checkpoint. Being an active participant—asking questions and confirming details with your nurses, surgeon, and anesthesiologist—empowers you and reinforces the safety and precision of your care plan.
Your Hospital Go-Bag: A Minimalist Packing List
Even for a short hospital stay, a small, well-packed bag can make a world of difference to your comfort. The goal isn’t to move in; it’s to bring a few key items that make the clinical environment feel a bit more personal and manageable.
Here’s a practical list of what to bring:
- Loose Clothing: Pack loose-fitting pants or shorts with an elastic waistband. You’ll need something that can easily slide over a bulky knee dressing for the ride home.
- Slip-On Shoes: Tying laces is off the table. A pair of sturdy, rubber-soled slip-on shoes or slippers is non-negotiable for those first few assisted steps.
- Personal Items: While the hospital provides the basics, having your own toothbrush, toothpaste, or face wash can be a huge psychological boost.
- Distractions: Load a tablet with movies or bring a book. Most importantly, pack headphones and an extra-long charging cable—hospital outlets are notoriously out of reach.
- Key Documents: Keep your ID, insurance card, and any required hospital paperwork together in a single folder for easy access.
The Final Pre-Flight Check: Empowering Questions for Your Team
The moments just before your procedure are your last opportunity to gain clarity and ensure everyone is perfectly aligned. Asking targeted questions isn’t about being difficult; it’s about being an engaged and informed member of your own team.
Before any procedure, I advise my clients to have a short list of final confirmation questions ready. This small step provides immense peace of mind.
| Question Category | Specific Questions to Ask |
|---|---|
| For the Surgeon | “Could you walk me through the key steps of the procedure one more time?” “What is the specific pain management protocol for my first 24 hours?” |
| For the Anesthesiologist | “What are the most common side effects of our chosen anesthesia, and how will you manage them?” |
| For the Nursing Team | “What should I expect in terms of pain and mobility when I first wake up in recovery?” “What are the key milestones I need to hit before discharge?” |
These questions do more than just get you answers—they confirm the pain strategy, set clear post-op expectations, and reinforce that you are the central figure in a well-coordinated plan for a successful outcome.
Common Questions About Preparing for Knee Surgery
Even with a detailed plan, questions always pop up. They’re the practical, “what-if” scenarios you think about in the quiet moments before your procedure. Getting clear answers to these common concerns provides an extra layer of confidence, making sure you feel fully informed and ready for what’s ahead.
Think of this as a focused look at the details that patients ask about most as they finalize their prep for knee surgery.

How Soon Should I Start Prehabilitation Exercises?
Ideally, you want to start a structured prehab program four to six weeks before your surgery date. This gives you enough time to build meaningful strength in the key muscles around the knee—your quads, hamstrings, and glutes—without overdoing it and causing inflammation.
Starting early makes a huge difference. Research consistently shows that patients who go into surgery stronger have a faster recovery, less pain afterward, and often shorter hospital stays. Of course, you should always talk to your orthopedic surgeon and a physical therapist first. They’ll help create a safe, personalized plan that’s right for your specific condition and fitness level.
What Are the Most Critical Home Modifications?
When it comes to your home, the game is all about safety and accessibility. Your single most important goal is to minimize the risk of a fall. That risk is highest in the first few weeks after surgery when your mobility is shaky at best.
Here’s your non-negotiable checklist:
- Clear All Pathways: Get rid of tripping hazards. This means rolling up throw rugs, securing electrical cords, and clearing any clutter from the walkways you’ll be using.
- Optimize the Bathroom: This is a high-risk area. Install grab bars in the shower and next to the toilet. A shower chair and a raised toilet seat are also absolute must-haves for both safety and comfort.
- Create a Recovery Station: Set up a “command center” on your main living floor, whether that’s your bed or a comfortable recliner. Keep everything you need within arm’s reach: medications, phone, water, TV remote. The less you have to use the stairs, the better.
These simple changes can dramatically reduce physical strain and give you significant peace of mind as you move around your home during recovery.
Can I Continue My Usual Supplements Before Surgery?
This is a critical question, and the answer is almost always no—at least not without a thorough review from your medical team. You must discuss every single supplement, vitamin, and herbal remedy with your surgeon and anesthesiologist at least two weeks before your procedure.
Many common supplements, even the “natural” ones, can cause serious problems during surgery. For instance:
- Fish Oil & Vitamin E: Both have blood-thinning properties that can increase bleeding risk.
- Garlic & Ginkgo Biloba: These are also known to interfere with blood clotting.
- St. John’s Wort: Can mess with how your body metabolizes anesthesia drugs.
Your surgical team will give you a specific list of what to stop and when. Don’t stop taking any prescribed medications unless they tell you to, but be ready with a complete list of everything you take, including all over-the-counter products.
Key Takeaway: Full transparency is non-negotiable. What might seem like a harmless vitamin can create serious complications. Your medical team needs a complete picture to ensure your safety.
What Is a Realistic Pain Management Plan?
Let’s be clear: you will have some pain after surgery. It’s an expected part of the process. But modern pain management is a sophisticated strategy designed to keep you as comfortable as possible. Your team will almost certainly use a “multimodal” approach, combining different medications and techniques to attack pain from multiple angles. This strategy also helps minimize the need for opioids.
A typical plan might look like this:
- Nerve Blocks: Often given before surgery, these numb the area for the first 12-24 hours, providing a fantastic head start on pain control.
- Local Anesthetics: Your surgeon might inject long-acting numbing medication directly into the tissues around the new joint.
- Scheduled Medications: You’ll likely be on a regular schedule of non-opioid pain relievers, like anti-inflammatories (NSAIDs) and acetaminophen.
- Opioids for Breakthrough Pain: Stronger opioid medications are typically reserved for those moments of more intense, or “breakthrough,” pain that isn’t controlled by the other methods.
Discuss your pain management plan in detail with your surgeon and anesthesiologist beforehand. Understanding the strategy and having realistic expectations is the key to managing post-operative discomfort effectively and with confidence.
At Haute MD, we connect discerning patients with the nation’s most distinguished, board-certified specialists. Discover an elite network of physicians who deliver precision, innovation, and unparalleled care. Find a trusted orthopedic expert near you and ensure your surgical journey is guided by the best in the field by exploring our network at https://www.hauteliving.com/hautemd.

