
So, what’s the real story with red meat and gout? Let’s cut to the chase. While eating a steak doesn’t directly cause the underlying condition, it is a major trigger for agonizing flare-ups in anyone who’s susceptible. If you’re prone to gout, red meat dramatically increases the odds of a painful attack.
The Real Link: Why a Burger Can Trigger a Flare
To get a clear picture of what’s happening, think of your body as a bathtub. A compound called uric acid is the water.
Red meat is loaded with substances called purines. When your body metabolizes these purines—from a burger, a steak, or lamb chops—it produces uric acid as a byproduct. Eating a large portion of red meat is like cranking the faucet on full blast, rapidly filling the tub.
Now, for most people, the kidneys act like a highly efficient drain, filtering out this excess uric acid without any trouble. But if you’re predisposed to gout, your drain is either slow or partially clogged. This means your body is either making way too much uric acid or, more commonly, it just can’t clear it out fast enough.
What Happens When Uric Acid Levels Spike
When the “bathtub” starts to overflow, the uric acid in your bloodstream reaches a saturation point. It can no longer stay dissolved. Instead, it crystallizes, forming microscopic, needle-sharp shards.
These sharp crystals drift through your bloodstream and eventually settle in your joints—most famously the big toe, but the ankles, knees, and wrists are also common targets. Your immune system spots these crystals, mistakes them for foreign invaders, and launches an all-out inflammatory assault to destroy them.
This intense immune response is what you experience as a gout flare. The symptoms are unmistakable:
- Sudden, excruciating joint pain that people often describe as unbearable.
- Significant swelling and extreme tenderness around the joint.
- Deep redness and a feeling of intense heat over the area.
The pain from a gout attack is legendary for a reason. It’s often so severe that even the slight pressure from a bedsheet can feel like a crushing weight. This isn’t just a bit of joint ache; it’s a full-blown inflammatory crisis triggered by those tiny crystals.
So, while red meat isn’t the root cause of your faulty “drain,” its high purine content is one of the biggest reasons the “tub” overflows. This direct link makes managing your red meat intake an absolute cornerstone of any effective gout strategy. Understanding this process is the first, most critical step toward building a diet that protects your joints and keeps you out of the red zone.
How Your Body Turns a Steak into Gout Pain
To really get to the bottom of the “does red meat cause gout” question, we have to follow what happens from the moment you take a bite of steak. The whole story hinges on a group of organic compounds called purines.
Think of purines as tiny biological Lego bricks. Your body uses them to build and repair essential things like DNA and RNA. While your body makes some of these purines on its own, a huge chunk comes directly from your diet. And red meats—beef, lamb, pork—are absolutely loaded with these purine “bricks.”
When you dig into that steak, your digestive system starts breaking it down. As it metabolizes the meat, it also breaks down the purines tucked inside its cells. This process creates a natural waste product: uric acid.
From Harmless Waste to Painful Crystals
Most of the time, this is a perfectly normal, harmless cleanup job. The uric acid flows into your bloodstream, your kidneys filter it out, and you get rid of it through your urine. Your body keeps everything in a neat balance, and you’re none the wiser.
The trouble starts when that delicate system gets overwhelmed. This usually happens in one of two ways:
- Overproduction: Eating a lot of high-purine foods like red meat floods your system, forcing your body to crank out way too much uric acid.
- Under-excretion: Sometimes, for reasons like genetics or kidney issues, your body just can’t filter out uric acid fast enough to keep up, even with normal production.
When either of these happens, the concentration of uric acid in your blood starts to creep up. This condition is called hyperuricemia.
It’s like dissolving sugar in a glass of iced tea. A little bit dissolves no problem. But if you keep piling it in, you’ll hit a point where the tea is saturated. The extra sugar can’t dissolve anymore, so it just sinks to the bottom and forms solid crystals.
That’s exactly what happens in your bloodstream. When uric acid levels get too high, it can no longer stay dissolved. It crashes out of solution, transforming from a liquid into microscopic, needle-sharp solid crystals called monosodium urate crystals.
This simple chart breaks down that biological chain reaction.
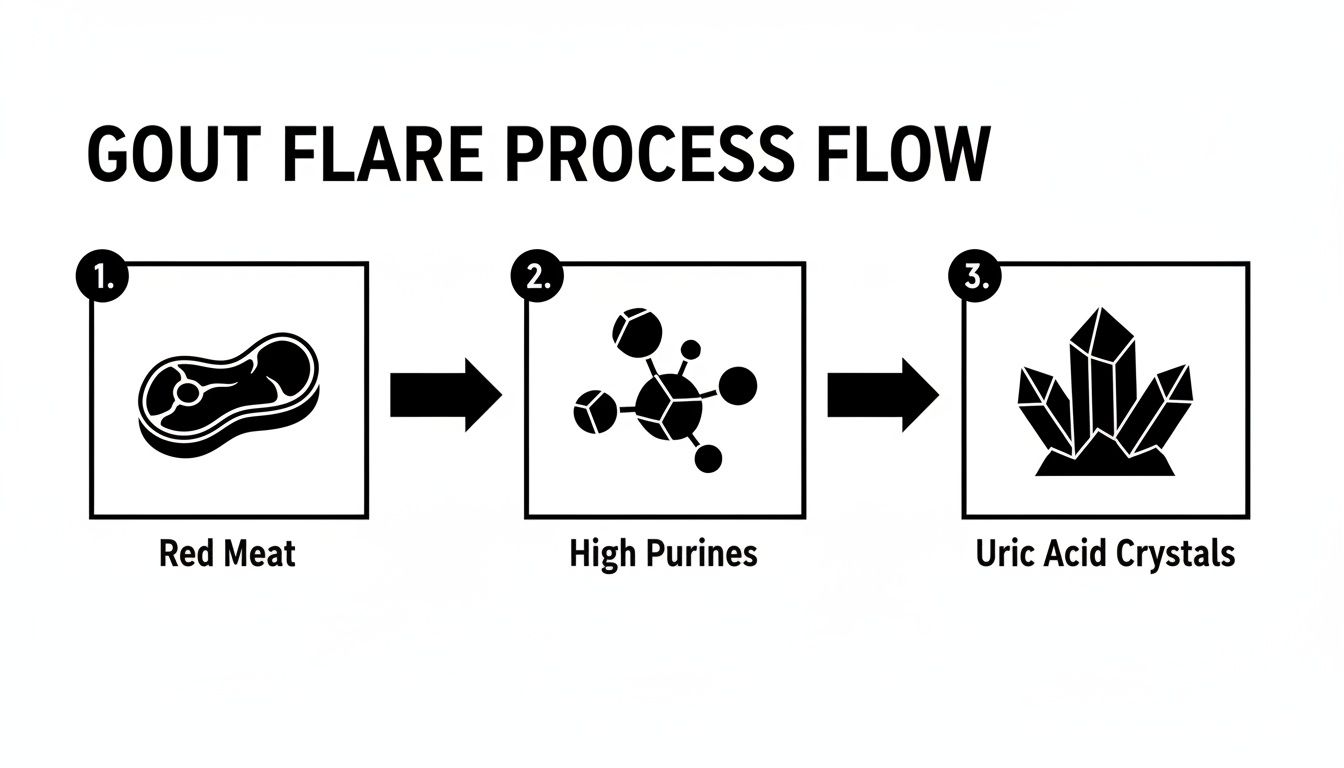
As you can see, the high purine content in red meat is the direct starting point for the uric acid crystals that kick off a gout flare.
The Science Behind the Numbers
This isn’t just a theory; it’s backed by some serious science. A landmark study from Massachusetts General Hospital followed nearly 47,000 men for 12 years to nail down the exact risk tied to meat. The results were crystal clear.
Men who ate the most red meat (about 2.5 servings daily) had a staggering 41% higher risk of developing gout compared to those who ate the least. The data even showed that just one extra daily serving of red meat jacked up the odds of a gout attack by 21%. You can dig into the specifics and powerful implications in the original study.
How Crystals Trigger a Gout Attack
Once these razor-sharp crystals form, they start circulating through your body. They tend to settle in your joints and the surrounding tissues, often drawn to areas with lower temperatures, like the big toe. But they can just as easily set up shop in your ankles, knees, wrists, or elbows.
Your immune system spots these crystals and freaks out, treating them like foreign invaders—splinters or bacteria. It launches an all-out inflammatory assault to destroy them. White blood cells swarm the area, engulfing the crystals and releasing a flood of inflammatory chemicals called cytokines.
This intense immune response is what you feel as a gout flare: the agonizing pain, the dramatic swelling, the deep redness, and the intense heat in the joint. It’s not the uric acid itself that hurts; it’s your body’s ferocious battle against the crystals it creates.
What the Scientific Evidence Actually Shows
The idea that a steak dinner can trigger a painful gout flare-up isn’t just a story passed down through generations—it’s a conclusion cemented by decades of large-scale scientific research. To really get to the bottom of this, we have to look past individual stories and dive into what massive studies, tracking thousands of people over many years, have uncovered. This isn’t about guesswork; it’s about seeing the clear, undeniable patterns that emerge from the data.https://www.youtube.com/embed/dEQ-SOoVLz8
When researchers dig into this data, they use a metric called relative risk. It’s a straightforward way to compare the odds of something happening in one group versus another. For example, if a study reports a relative risk of 1.41, it means the group with the high-risk behavior—in this case, eating a lot of red meat—has a 41% greater chance of developing a condition compared to the low-risk group.
That 1.41 figure isn’t hypothetical. It’s the precise number that came out of one of the most important long-term health studies ever conducted on men and diet. The evidence trail is direct, consistent, and points to a powerful link between diets heavy in red meat and the rise of gout.
Landmark Studies and What They Reveal
One of the most powerful tools in a researcher’s arsenal is the prospective cohort study. Think of it like this: scientists recruit a huge group of healthy people and then follow them for years, sometimes even decades. Along the way, they meticulously track everything from what they eat to their health outcomes. This approach allows them to connect the dots between specific lifestyle choices, like red meat consumption, and the eventual development of diseases like gout.
And these studies consistently point in one direction. The more red meat a person consumes, the higher their risk of developing gout becomes. The data isn’t subtle, either. It shows what’s called a dose-dependent relationship—meaning each additional weekly serving of red meat incrementally cranks up the risk.
The message from this mountain of evidence is crystal clear: while your genetics might load the gun for gout, a diet rich in red meat is like pulling the trigger. It dramatically increases the odds you’ll experience those excruciating flares.
This body of research also helps explain a broader trend. Gout cases have been on the rise, right alongside the global adoption of the “Western” diet, which is notoriously high in red and processed meats, refined carbs, and sugary drinks. It’s a massive public health pattern with diet sitting right at the center.
Red Meat vs Other Protein Sources and Gout Risk
Not all protein is created equal when it comes to gout risk. Major epidemiological studies have teased apart the effects of different protein sources, and the results are telling.
This table compares the relative risk of gout associated with high consumption of different protein sources, based on findings from major epidemiological studies.
| Protein Source | Purine Level | Impact on Gout Risk | Key Study Finding |
|---|---|---|---|
| Red Meat | High | Significant Increase | Highest intake linked to a 41% higher risk compared to lowest intake. |
| Seafood | Varies (High) | Moderate to High Increase | High consumption associated with a 51% increased risk. |
| Poultry | Moderate | Slight Increase | Much lower risk increase compared to red meat and seafood. |
| Dairy | Low | Protective (Decrease) | High intake linked to a 44% lower risk of gout. |
| Plant Protein | Low | No Increased Risk | No association found between high intake and gout risk. |
The data makes it obvious: swapping a serving of beef for low-fat dairy or plant-based protein isn’t just a minor tweak—it’s a strategic move to actively lower your uric acid burden and reduce your risk of a flare.
The Power of Meta-Analyses
To get an even clearer, more definitive answer, scientists take it a step further and perform a meta-analysis. This is essentially a “study of studies.” They pool all the data from multiple independent research projects into one massive, super-powered dataset. This process smooths out any minor inconsistencies between individual studies and gives us a conclusion that’s far more robust and reliable than any single study could provide on its own.
And when it comes to diet and gout, these meta-analyses have solidified the connection beyond any reasonable doubt. By combining results from different populations and study designs, they confirm that a high intake of red meat is a significant, independent risk factor for both high uric acid levels (hyperuricemia) and full-blown gout attacks.
For example, a major 2014 review published in the Asia Pacific Journal of Clinical Nutrition crunched the numbers from several of the most important studies in the field. The final verdict? Individuals who ate the most red meat had a 29% increased risk of developing gout or hyperuricemia compared to those who ate the least. With consistent findings like these across numerous studies, there’s little room for debate.
You can dive into the full findings of this powerful research for yourself. This wealth of evidence gives us the scientific certainty we need to make smart, informed choices about our diet. It shifts the conversation from “does red meat cause gout?” to the much more practical question of how we can moderate our intake to effectively manage risk and protect our joints.
Building a Practical Gout-Friendly Diet
Knowing that red meat can be a gout trigger is one thing; building a sustainable diet to manage it is where the real work—and real progress—happens. This isn’t about deprivation or a joyless eating plan. It’s about being smart with moderation, strategic with what you add to your plate, and empowering yourself with the right knowledge. Think of it less as avoiding foods and more as actively building a diet that helps your body handle uric acid more effectively.

This dietary approach is more than a passing trend—it’s a critical piece of the global health puzzle. The explosion of gout worldwide is directly linked to the dietary habits of high-income nations. By 2019, an estimated 53.9 million people were living with gout globally. The age-standardized prevalence hit a staggering 652.2 per 100,000, which is a 22.4% jump from 1990.
High-income North America saw a massive 56.6% increase, driven largely by the “Westernization” of diets heavy in purine-rich red meat. You can dig deeper into these global dietary trends and their impact on gout on CABI Digital Library.
Red Meat Moderation: What It Really Looks Like
When it comes to red meat, “moderation” is the golden rule, but what does that actually mean on your plate? It comes down to two simple things: portion size and frequency.
A sensible portion of red meat is about 3 to 4 ounces—roughly the size and thickness of the palm of your hand. In terms of frequency, many people with well-managed gout find they can enjoy a portion like this once or twice a month without stirring up trouble. It’s about treating red meat as an occasional indulgence, not a daily staple.
And remember, not all red meat is created equal. Some types are exceptionally high in purines and should be strictly limited or avoided altogether.
- Highest Purine Meats to Limit: Organ meats (like liver, kidneys, and sweetbreads), game meats (venison, duck), and certain fatty cuts of beef and lamb are the biggest offenders.
- Better Alternatives: When you do have red meat, opt for leaner cuts like sirloin or flank steak. Pork tenderloin and skinless poultry are also much safer bets.
By simply choosing leaner cuts and sticking to that palm-sized portion, you can dramatically cut your purine intake from a single meal.
Focusing on What You Should Eat
A successful gout diet is defined more by what you add than what you take away. The right foods can actively help your body lower uric acid levels and cool inflammation. Making these a regular part of your diet is a powerful, proactive strategy.
Shifting your focus from “what can’t I have?” to “what beneficial foods can I add?” transforms your entire mindset. It turns diet management from a restrictive chore into a positive, empowering action for your health.
Here are some key players to incorporate:
- Cherries: Both sweet and tart cherries contain compounds that are superstars at lowering uric acid and reducing inflammation.
- Low-Fat Dairy: Things like skim milk and low-fat yogurt have a protective effect, actually helping your kidneys excrete uric acid.
- Vitamin C-Rich Produce: Foods like bell peppers, oranges, strawberries, and broccoli can help lower uric acid levels naturally.
Managing your diet is a cornerstone of your overall wellness. For a deeper dive, check out our guide on how to improve metabolic health.
The Critical Role of Hydration
Of all the dietary tools at your disposal, perhaps the most effective—and simplest—is hydration. Water is your body’s natural flushing system.
Drinking plenty of water helps your kidneys do their job efficiently. Aim for at least eight glasses a day, and even more if you’re active. It dilutes the uric acid in your blood and helps your kidneys filter it out of your system before it can crystallize in your joints. Think of it as keeping the “drain” clear to prevent the “bathtub” from overflowing.
By combining smart moderation of red meat, an increased intake of protective foods, and a serious commitment to hydration, you build a practical and powerful defense against gout flares. This approach puts you back in control, turning your daily meals into an opportunity to support your joint health.
Here’s a quick-reference guide to help you make informed choices at a glance.
Purine Content in Common Foods (High to Low)
| Food Category | High-Purine Examples (Avoid/Limit) | Moderate-Purine Examples (Eat in Moderation) | Low-Purine Examples (Enjoy Freely) |
|---|---|---|---|
| Meat & Poultry | Organ meats (liver, kidney), bacon, game meats (venison), goose | Beef, pork, lamb, chicken, turkey (limit to 4-6 oz/day) | – |
| Seafood | Anchovies, sardines, herring, mussels, scallops, trout, haddock | Tuna, crab, lobster, shrimp, oysters (limit to 4-6 oz/day) | Most other fish in moderation |
| Vegetables | – | Asparagus, spinach, cauliflower, mushrooms, green peas, dried beans | Most other vegetables, including leafy greens, broccoli, peppers |
| Fruits | – | – | All fruits, especially cherries and those high in Vitamin C |
| Dairy & Eggs | – | – | Low-fat milk, low-fat yogurt, eggs |
| Grains | – | Whole grains like oatmeal, brown rice, whole wheat bread | Refined grains (white bread, pasta), rice |
| Beverages | Beer, spirits, sugary drinks (high-fructose corn syrup) | – | Water, coffee, tea, tart cherry juice |
This table isn’t about creating a “bad” list of foods but empowering you with the knowledge to balance your plate and manage your gout effectively.
Your Action Plan for Gout: From Prevention to Flare Management
Knowing what triggers gout is half the battle. But to truly get the upper hand, you need a complete toolkit—one that covers long-term prevention and what to do the moment a flare strikes. It’s about more than just watching what you eat; it’s a proactive strategy for your entire lifestyle. When you pair smart daily habits with a clear plan for an acute attack, you build a powerful defense against the pain and disruption of gout.

Successfully managing gout isn’t just about reacting to pain. It’s about creating a system that makes flares less likely in the first place. This proactive approach protects your joints from long-term damage and gives you back control over your health.
Lifestyle Strategies for Long-Term Prevention
While diet is a cornerstone, other lifestyle factors play a huge part in keeping your uric acid levels where they should be. Make these habits part of your routine, and you’ll dramatically lower your risk of future attacks.
- Maintain a Healthy Weight: Excess body weight doesn’t just put stress on your joints; it actually increases uric acid production while slowing down its removal by the kidneys. Even a modest amount of weight loss can make a big difference.
- Limit Alcohol, Especially Beer: Alcohol is a double threat. It’s often high in purines (beer is a major culprit) and it can dehydrate you, concentrating the uric acid in your system. If you do drink, keep it moderate and make sure to drink extra water.
- Stay Well-Hydrated: As we’ve covered, water is your best friend in the fight against gout. It helps your kidneys do their job and flush out excess uric acid. Aim for at least eight glasses a day, maybe more.
These adjustments are so important because they target the underlying metabolic issues that lead to high uric acid. For those who want to dig deeper into this, understanding how to reverse metabolic syndrome offers powerful insights into managing these related health risks.
It’s a common myth that gout is just about eating too much steak. The truth is, it’s a complex metabolic condition. Diet is a piece of the puzzle, but your genetics, kidney function, and overall lifestyle are just as critical.
What to Do During an Acute Gout Flare
Even with the best game plan, a flare-up can still happen. When it does, knowing exactly what to do can help you get through the intense pain and shorten the attack.
1. Act Fast with Medication: At the very first twinge of a flare, take the anti-inflammatory medication prescribed by your doctor. This is often an NSAID (like ibuprofen or naproxen) or a specific gout drug like colchicine. The faster you act, the more effective the medicine will be.
2. Rest the Affected Joint: A gout attack puts enormous stress on a joint. Stay off it. Avoid putting any weight on the joint and rest as much as you possibly can. A cane or crutches can be a lifesaver if your foot, ankle, or knee is the target.
3. Apply Ice: Cold packs are your friend. They are fantastic for reducing inflammation and numbing that searing pain. Wrap an ice pack in a thin towel and apply it to the joint for 20-30 minutes at a time, several times a day.
4. Elevate the Joint: Raising the affected limb helps drain fluid and reduce swelling. If your big toe is screaming, prop your foot up on a few pillows so it’s higher than your heart.
Understanding Your Medications
Your doctor might prescribe different medications for different jobs. It’s crucial to know what each one does.
| Medication Type | Purpose | When to Use | Common Examples |
|---|---|---|---|
| Acute Flare Relief | To knock down pain and inflammation quickly. | At the very first sign of a flare. | NSAIDs, Colchicine, Corticosteroids |
| Long-Term Prevention | To lower your body’s overall uric acid levels. | Daily, as prescribed by your doctor. | Allopurinol, Febuxostat |
These two types of drugs are not interchangeable. The fast-acting drugs are for immediate rescue, while the long-term medications work quietly in the background to stop attacks from happening. Following your doctor’s instructions is non-negotiable for keeping gout under control and protecting your joints from permanent damage.
When Should You See a Doctor About Gout?
Self-management is a powerful tool in your health arsenal, but it’s no substitute for professional medical care. While understanding the link between red meat and gout is a great first step, knowing when to bring in an expert is just as crucial. Don’t guess when it comes to severe joint pain; getting an accurate diagnosis is the only way to get effective, long-term relief.
It’s also worth remembering that many other conditions can mimic the symptoms of gout. A proper medical diagnosis is critical to rule out other issues and ensure you’re on the right treatment path with a safe, personalized plan.
Key Signals to Schedule an Appointment
Certain symptoms are a clear sign that it’s time to stop the guesswork and seek professional medical advice. If you experience any of the following, make an appointment with your primary care physician for an initial workup.
- A First-Time Suspected Attack: If you’ve never had gout before but wake up with sudden, excruciating pain in a joint—especially the big toe—you need a diagnosis.
- Flares Are Becoming More Frequent: If your attacks start happening more often or are more severe than in the past, your current management plan isn’t working. It’s time to escalate care.
- Appearance of Tophi: Noticing small, hard, chalky lumps under your skin is a red flag. These deposits, often found on elbows, fingers, or ears, are a sign of chronic, uncontrolled gout that needs immediate medical attention.
One of the most dangerous misconceptions about gout is that it’s only a problem during a flare. Even when the pain subsides, high uric acid levels can continue to cause silent, cumulative damage to your joints, kidneys, and other tissues. Consistent medical oversight is essential for preventing these long-term complications.
Finding the Right Specialist
Your primary care doctor is the perfect starting point for diagnosis and initial management. However, for complex, persistent, or severe cases, they will likely refer you to a rheumatologist. These specialists are the true experts in arthritis and related inflammatory conditions.
Finding the right expert is crucial for managing a condition like gout effectively. If you’re looking for specialized care, exploring a curated list of top doctors who treat arthritis can give you access to leading physicians in the field. An experienced specialist can offer advanced treatment options and a tailored strategy to protect your health for years to come.
Answering Your Questions About Gout and Diet
Once you understand the link between red meat, purines, and uric acid, the practical questions start popping up. How does this all play out on my dinner plate? Here are direct answers to the most common questions I hear from patients trying to navigate a gout-friendly diet.
Can I Eat Red Meat at All if I Have Gout?
For most people, the answer is yes—but with strict rules. Complete elimination isn’t usually necessary if your gout is otherwise well-managed. The key is moderation, and I mean true moderation.
Think of it as a rare indulgence, not a regular part of your meal rotation. For many, a small 3-4 ounce portion of red meat once or twice a month is a manageable risk. Stick to leaner cuts, and make organ meats like liver an absolute no-go zone; they are packed with purines. Of course, you need to run this by your doctor to figure out what’s safe for your specific situation.
Remember, managing gout is about building a sustainable lifestyle, not a miserable, restrictive one. An occasional, well-planned meal is worlds apart from making high-purine foods a dietary staple.
Are Plant-Based Purines as Bad as Those in Meat?
No, and the evidence on this is quite strong. Large-scale studies have shown, quite convincingly, that purine-rich vegetables like spinach, asparagus, and mushrooms do not increase the risk of gout attacks or raise uric acid levels.
It seems our bodies process purines from plants very differently than those from animal sources. So, there is no need to limit your intake of these healthy, nutrient-packed vegetables. They should absolutely remain a core part of your diet.
Which Is More Important for Gout: Diet or Medication?
This is a classic question, and the answer is that they are a team—you need both. Trying to choose between them is a false choice. Diet and lifestyle changes are your foundational defense, helping to reduce the daily purine load and minimize the frequency and intensity of painful flares.
However, for the vast majority of people with gout, diet alone is simply not powerful enough to lower uric acid to a consistently safe level. That’s where medication comes in. Uric acid-lowering therapies are often essential to prevent the silent, long-term joint damage that high uric acid causes.
Think of it this way: Diet is your daily strategy, while medication is the crucial tool that protects your joints for the long haul.
Finding the right medical expert is the single most important step in managing your health. Haute MD connects you with a curated network of the nation’s top physicians, from rheumatologists to metabolic specialists, ensuring you receive premium, outcome-driven care. Explore our network at Haute MD website to find a trusted specialist near you.

