Doctors of internal medicine are the specialists adults turn to for diagnosing, treating, and preventing the full spectrum of diseases. Commonly known as internists, they are often called the “master detectives” of adult healthcare—and for good reason. They possess a unique talent for solving complex diagnostic puzzles and managing intricate, often multi-system conditions. For many adults, an internist is their primary care provider, the trusted quarterback overseeing their long-term health.
The Role of a Health Detective
Think of an internist as a brilliant detective, but for your health. While many physicians focus on a single organ system—a cardiologist for the heart, a dermatologist for the skin—an internist is trained to see the entire picture. They excel at connecting seemingly unrelated symptoms, analyzing complex evidence from lab results and patient history, and solving the medical mysteries that can impact adults.
Their specialized focus is squarely on the adult body, from late adolescence through the senior years. This allows them to develop a profound understanding of how diseases present and progress over a lifetime. Whether you’re dealing with a common illness or a rare, chronic condition, your internist has the diagnostic toolkit to dig for the root cause and coordinate a truly comprehensive treatment plan.
Rigorous Training and Board Certification
Becoming one of these health detectives is a demanding journey. After four years of medical school, aspiring doctors of internal medicine dive into a rigorous three-year residency program. This is where the real-world training happens. They gain intensive, hands-on experience in various settings, from fast-paced hospitals to outpatient clinics, learning to manage the vast spectrum of adult illnesses.
Once their residency is complete, the best internists pursue board certification from the American Board of Internal Medicine (ABIM). This isn’t just a piece of paper; it’s the gold standard. It signifies that a physician has demonstrated exceptional knowledge and skill in their field. It’s a mark of commitment to the highest standards of care, and it requires continuous learning to maintain—a key reason why discerning patients seek them out.
The Foundation of Adult Primary Care
Internal medicine is one of the most vital physician specialties in the United States, forming the very foundation of adult healthcare. Internists are often the first point of contact for patients, acting as trusted primary care physicians who manage everything from preventive screenings to chronic disease. The scale of their importance is staggering; in 2022, there were an estimated 124,000 practicing general internists in the U.S., serving millions of adults. You can discover more insights about the role of internists in the US healthcare system.
Internists have two main paths. Many choose to practice general internal medicine, where they build lasting, long-term relationships with their patients. Others pursue further training in one of over a dozen subspecialties, becoming experts in areas like:
- Cardiology (heart diseases)
- Endocrinology (hormonal disorders)
- Gastroenterology (digestive system)
- Oncology (cancer treatment)
This deep and broad training is what allows internists to diagnose and manage complex health issues effectively. The following table breaks down their key responsibilities.
Core Responsibilities of an Internist
| Area of Focus | Description |
|---|---|
| Complex Diagnosis | Investigating and solving challenging medical puzzles, especially when symptoms are vague, multi-system, or don’t fit a clear pattern. |
| Chronic Disease | Managing long-term conditions like diabetes, hypertension, heart disease, and autoimmune disorders, often coordinating with other specialists. |
| Preventive Care | Conducting screenings, health risk assessments, and counseling on lifestyle factors to prevent diseases before they start. |
| Acute Illness | Treating common and serious short-term illnesses, from severe infections to sudden onsets of symptoms requiring immediate attention. |
| Care Coordination | Acting as the central point of contact for a patient’s health, ensuring that care from various specialists is integrated and aligned with overall health goals. |
| Pre-operative Care | Evaluating a patient’s overall health and risks before surgery to ensure they are medically optimized for the procedure and recovery. |
| Whole-Patient Care | Considering the interplay of physical, mental, and social factors on a patient’s health, rather than just focusing on a single symptom or organ system. |
Ultimately, an internist’s role is to serve as the patient’s primary health advocate and strategist, applying a wide lens to their care.
An internist’s ability to diagnose without a clear starting point is what truly sets them apart. They are trained to handle ambiguity and complexity, making them the ideal quarterback for your long-term health and wellness journey.
This blend of broad knowledge and the potential for deep specialization makes doctors of internal medicine uniquely equipped to provide sophisticated, whole-body care. They don’t just manage the illness; they manage the entire person, ensuring every aspect of your health is considered and coordinated.
Internist vs. Family Doctor: Key Differences Explained
Choosing a primary care physician is one of the most critical health decisions you’ll ever make. As you navigate your options, two titles inevitably surface: internist and family doctor. While both are exceptional primary care providers, doctors of internal medicine and family physicians differ fundamentally in their training, patient focus, and the overall scope of their practice.
Getting this choice right is crucial for ensuring you have the best possible quarterback for your long-term health, especially as an adult. The core distinction boils down to the patient population they are trained to serve. Think of it this way: a family doctor is like a generalist author, skilled at writing for an audience of all ages. An internist, however, is a specialist author who writes exclusively for adults, developing a profound expertise in the specific complexities and nuances of that readership.
This flowchart can help you visualize the decision-making process when you’re weighing your options for adult medical care.
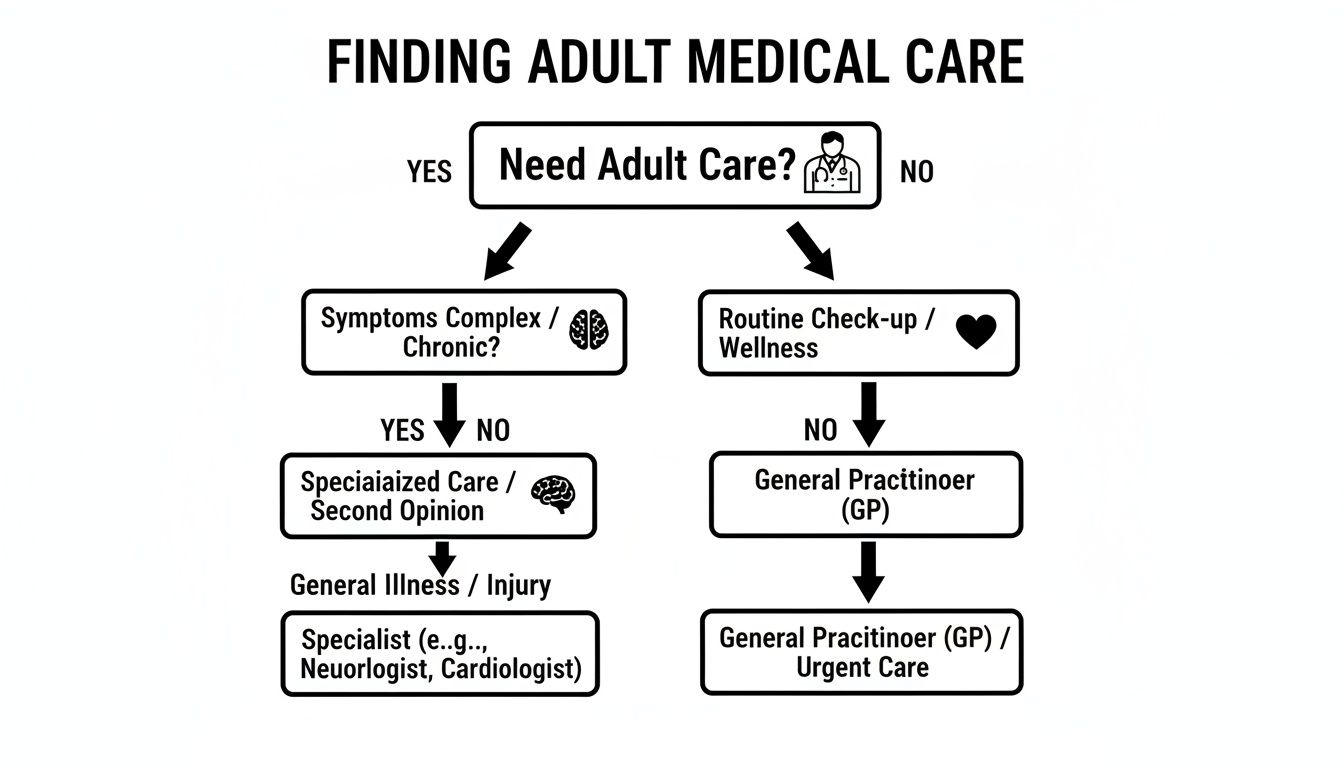
As you can see, both paths lead to high-quality care. But the internist’s route is specifically engineered for a deeper, more specialized approach to managing adult health.
Patient Focus: The Primary Distinction
The single most important difference is patient age. A doctor of internal medicine—an internist—exclusively treats adults, from late adolescence all the way through their senior years. Their entire three-year residency is dedicated to the prevention, diagnosis, and management of diseases that affect adults.
In contrast, a family doctor’s training is intentionally broad, designed to provide comprehensive care for the entire family unit. They are trained to see patients of every age, from newborns and toddlers to adolescents, adults, and the elderly. This “cradle-to-grave” model equips them to handle a massive variety of medical issues across all life stages.
Training and Scope of Practice
This difference in patient focus directly shapes their medical training and, ultimately, how they practice. An internal medicine residency provides a concentrated, in-depth education on conditions unique to adults. Internists spend years immersed in managing complex chronic illnesses like heart disease, diabetes, and autoimmune disorders. They become experts in the intricate ways multiple diseases can interact within a single adult patient—a common and challenging scenario.
A family medicine residency, on the other hand, covers a much wider curriculum. Their training includes mandatory rotations in areas an internist’s doesn’t:
- Pediatrics: Caring for infants, children, and adolescents.
- Obstetrics and Gynecology: Providing women’s health services, sometimes including prenatal care and deliveries.
- General Surgery: Gaining foundational surgical knowledge for common procedures.
This broad-spectrum training makes family doctors incredibly versatile, but it means their time learning adult medicine is shared with other crucial specialties. For a closer look at how this training impacts care, our guide on the difference between internal medicine and primary care offers more detail.
An internist’s singular focus on adult medicine allows for a level of depth that is essential for managing complex, chronic, or multi-system diseases. They are, in effect, the specialists in adult primary care.
Making the Right Choice for Your Health
So, which doctor is right for you? It’s a straightforward decision once you clarify your needs. If you are an adult seeking a physician with specialized, deep knowledge of adult physiology and disease, a doctor of internal medicine is an excellent choice. They are particularly well-suited for individuals managing one or more chronic conditions or those invested in proactive, adult-focused preventative health and longevity.
If, however, you need a single physician to care for your entire family, including your children, then a family doctor is the more logical option. Their ability to provide continuity of care for every family member, from pediatrics to geriatrics, is a significant advantage in that context.
The table below breaks it down to help guide your decision.
| Feature | Doctor of Internal Medicine (Internist) | Family Doctor |
|---|---|---|
| Patient Population | Exclusively adults (late teens to seniors) | All ages (infants, children, adults, seniors) |
| Training Focus | Deep dive into complex adult diseases and chronic condition management. | Broad training across multiple specialties, including pediatrics and OB/GYN. |
| Practice Setting | Primarily outpatient clinics and hospitals. | Mostly outpatient clinics, serving the entire family unit. |
| Best For | Adults with complex health needs or multiple chronic conditions. | Families seeking a single physician for members of all ages. |
Exploring Premium Care with Concierge and Executive Health
For adults who demand more from their healthcare, the traditional system can feel broken. The high-volume, reactive model—think 15-minute appointments and long waits—leaves little room for deep dives into preventative strategies or comprehensive wellness planning. It’s a system designed for sick care, not health optimization.
This frustration has fueled the rise of premium care models, an arena where top-tier doctors of internal medicine truly shine. By offering unparalleled access and personalized attention, these models shift the entire focus from treating illness to proactively building health. It’s a move toward a deliberate, white-glove level of service, perfectly suited for the complex diagnostic skills of an internist.

This demand for a better experience is more than just a feeling; it’s a powerful market force. The global primary care market, anchored by internists, is projected to hit $733.32 billion in 2025 and climb to $1,092.61 billion by 2034. With North America making up 40% of this market, driven by rising rates of chronic disease, the appeal of premium models that actually prevent these conditions is stronger than ever.
The Concierge Medicine Model
Concierge medicine scraps the traditional payment model for a membership-based structure. Patients pay an annual or monthly fee, often called a retainer, directly to their physician’s practice. This fee unlocks a level of service and access that standard insurance reimbursements simply don’t support.
Think of it as having a personal health advisor on speed dial. By intentionally keeping their patient panels small, internists can offer benefits that are impossible in a conventional practice. This completely changes the patient experience.
Key benefits typically include:
- 24/7 Physician Access: Direct communication with your doctor via phone, text, or email—whenever you need them.
- Extended, Unhurried Appointments: Real conversations that last 30, 60, or even 90 minutes.
- Same-Day or Next-Day Scheduling: No more waiting weeks for an appointment when you’re feeling unwell.
- Proactive Wellness Planning: A deep focus on prevention, longevity, and personalized health optimization.
This model gives doctors of internal medicine the time and resources to fully deploy their expertise in complex adult health. To understand this approach in greater detail, you can explore what concierge medicine is and how it works in our dedicated guide.
The Executive Health Program
While it shares the same proactive DNA as concierge medicine, an executive health program is structured differently. It’s typically an intensive, single-day assessment designed for busy professionals, entrepreneurs, and leaders who need an incredibly thorough health evaluation without the calendar disruption.
Instead of an ongoing membership, an executive physical is a comprehensive deep dive into your current health status and future risks, with an internist acting as the quarterback for the entire experience.
An executive health assessment is the ultimate data-driven physical. It goes far beyond a standard check-up to create a detailed baseline and a strategic roadmap for peak performance and long-term wellness.
A typical program consolidates a full suite of advanced screenings and specialist consultations into one seamless, efficient day. This often includes:
- Advanced cardiac screenings like calcium scoring and stress tests.
- Detailed body composition and metabolic analysis.
- Cognitive and neurological function tests.
- Consultations with specialists such as nutritionists or exercise physiologists.
At the end of the day, you walk away with a detailed report and a personalized action plan from your doctor of internal medicine. For discerning patients who value both their time and their health, it’s the pinnacle of medical efficiency.
How to Select a Top-Tier Doctor of Internal Medicine
Choosing a physician is one of the most important decisions you’ll make for your long-term health. For discerning adults, picking a top-tier doctor of internal medicine isn’t just about finding someone with a valid license. It’s about finding a true partner in health—a brilliant diagnostician, a strategic advisor, and a trusted advocate who understands your goals for wellness and longevity.
The right internist doesn’t just treat symptoms after they appear. They anticipate risks, masterfully coordinate complex care, and provide the unhurried, thoughtful guidance that’s become a rarity in today’s high-volume healthcare system. This search requires a smart approach, starting with the basics and moving into the more subtle but critical aspects of communication and practice philosophy.

Start with the Essentials: Verification and Credentials
Before you even think about personality or practice style, you need to verify the non-negotiables. These are the foundational checks that ensure a physician meets the highest professional standards and has the specialized training you need.
The first step is checking for board certification. This is a critical marker of excellence, not just a piece of paper. You can easily verify any doctor’s status with the American Board of Internal Medicine (ABIM). ABIM certification confirms they’ve not only survived a grueling residency but have also passed demanding exams and are committed to the continuous learning required to stay at the forefront of medicine.
Next, dig into their specific training and any subspecialty credentials. If you’re managing a known heart condition or a complex hormonal disorder, an internist who completed an extra fellowship in cardiology or endocrinology offers a massive advantage. This information is almost always available on their practice website or professional profiles.
Key Questions to Ask a Potential Internist
Once you’ve confirmed their credentials, it’s time to understand their approach to medicine. This is where you find out if their philosophy aligns with yours. An initial consultation or a “meet and greet” is the perfect time to ask sharp, targeted questions that reveal how they actually practice.
Think of it as an interview. You’re not just gathering data; you’re testing for compatibility and seeing how they communicate under pressure. Their answers will give you a clear window into what you can expect from their care day in and day out.
To really get to the heart of a doctor’s practice style, you need to ask the right questions. The table below is designed to help you probe beyond surface-level answers and understand what a partnership with this physician would truly look like.
Essential Questions for Vetting a Potential Internist
| Category | Question to Ask | What You’re Looking For |
|---|---|---|
| Practice Philosophy | “Can you describe your approach to preventative care and longevity? How do you help patients move beyond just treating illness?” | A proactive, data-driven approach. Look for mentions of advanced diagnostics, risk stratification, and personalized wellness plans, not just standard annual physicals. |
| Complex Cases | “What is your experience with managing patients who have multiple chronic conditions? How do you handle complex diagnostic challenges?” | Confidence and a clear, systematic process. They should talk about collaborating with specialists and using a methodical approach to unravel complex medical puzzles. |
| Specialist Coordination | “How do you manage referrals? What is your process for collaborating with and vetting other specialists to ensure my care is seamless?” | A “quarterback” mentality. They should have a curated network of trusted specialists and a clear system for sharing information and co-managing your care. |
| Patient Communication | “What is the best way to communicate with you between appointments? Do you offer direct access for urgent questions?” | Accessibility and responsiveness. A top-tier doctor will have a clear, reliable system for communication, often including direct email or cell phone access in a concierge model. |
| Appointment Structure | “How much time do you typically reserve for a new patient visit or a comprehensive annual physical?” | Unhurried time. An answer like “60-90 minutes” signals a practice built on depth, whereas “15-20 minutes” is a hallmark of a traditional, high-volume model. |
These questions aren’t about catching a doctor in a “gotcha” moment. They are about opening a dialogue to ensure your expectations for proactive, high-touch care are perfectly aligned with their ability to deliver it.
Recognizing Red Flags and Warning Signs
Just as important as knowing what to look for is knowing what to avoid. Certain behaviors and practice patterns are clear signals that a doctor may not be the right fit, especially for a patient seeking attentive, world-class care.
Pay close attention to how you feel during your interactions. A top-tier physician should make you feel heard, respected, and empowered. If you walk out of an appointment feeling rushed, dismissed, or more confused than when you walked in, that’s a massive red flag.
Other warning signs to watch for include:
- Rushed Appointments: If you feel like you’re on a conveyor belt, it’s a sure sign of a volume-based practice that simply doesn’t have the time for deep, preventative medicine.
- Dismissive Attitude: A doctor who downplays your concerns, interrupts you, or doesn’t listen actively is not going to be a good long-term partner in your health.
- Poor Communication: Disorganized office staff, unreturned calls, and a struggle to get clear answers are all symptoms of a poorly managed practice.
- Lack of Transparency: Any hesitation to discuss their care philosophy, specialist network, or approach to complex cases should give you serious pause.
Ultimately, your intuition is a powerful tool. The best doctor-patient relationships are built on a foundation of mutual respect. If a physician’s style just doesn’t feel right, trust your gut.
Navigating the Growing Shortage of Primary Care Physicians
Finding an exceptional doctor of internal medicine is harder than ever, and it’s not just you. The entire healthcare system is groaning under the weight of a physician shortage that makes getting thoughtful, unhurried care feel like a luxury.
This isn’t some problem looming on the horizon—it’s here now, directly impacting your ability to get quality medical attention. The traditional model, already notorious for its 15-minute appointments and reactive approach, is being stretched to its breaking point. As doctors burn out and retire faster than they can be replaced, the pool of internists is shrinking just as an aging population needs them most.
The Numbers Behind the Strain
The data tells a stark story. Physician attrition rates are climbing, creating a widening gap between the number of patients who need care and the doctors available to provide it. This is especially true for doctors of internal medicine, who are the bedrock of adult primary care.
A recent decade-long study revealed a troubling trend: physician attrition climbed from 3.5% in 2013 to 4.9% in 2019. This contributes to a projected shortfall of up to 86,000 doctors by 2036, with a staggering 40,000 of those needed in primary care alone.
This mounting pressure translates into longer waits for appointments, shorter face-to-face time with your doctor, and less opportunity to build the kind of trusting, long-term relationship that is essential for great health management. You can learn more about the findings on physician attrition and what it means for the system.
The fallout from this shortage hits patients directly. Forget trying to get an extended consultation to dive deep into preventative strategies; it’s hard enough just to get a same-day appointment when you’re actually sick. This frustrating reality is precisely why alternative care models have become essential for anyone who refuses to compromise on their health. The growing physician shortage by specialty isn’t just a headline—it’s a critical factor in planning your healthcare future.
Premium Care as a Strategic Solution
In this strained environment, concierge medicine and executive health programs have emerged as a powerful answer. These aren’t just perks; they are a strategic move away from the systemic failures of modern healthcare. They offer a direct path to the attentive, high-quality care that is becoming so rare.
By stepping outside the high-volume, insurance-driven machine, internists in these practices can finally offer what the traditional model can’t:
- Time: Appointments are measured in hours, not minutes, creating space for real, meaningful conversations.
- Access: You can reach your physician directly, ensuring you get immediate guidance from someone who actually knows you.
- Proactivity: The entire focus shifts from just treating sickness to building a personalized, proactive plan for wellness and longevity.
Why Curated Networks Are the Answer
Trying to find a top-tier internist in one of these premium models on your own is a daunting task. How do you know who is truly exceptional? This is where a curated network becomes your most valuable asset.
Instead of a cold, impersonal Google search, a vetted network provides a clear, reliable path to elite physicians. These platforms do the exhaustive work for you, ensuring every single doctor listed meets strict criteria for board certification, professional reputation, and a deep-seated commitment to patient-centered care. They cut through the noise, connecting you directly with the doctors of internal medicine who are actively solving the access and quality problem through their superior practice models. It transforms a frustrating search into a confident choice.
Find Vetted Doctors of Internal Medicine Near You
You now understand what a doctor of internal medicine does. That’s the first step. The next—finding the right one—is the move that can completely change the course of your health. But after learning about their rigorous training and the premium care models they often lead, a practical question remains: how do you actually connect with a top-tier internist?
This is where most people get stuck. The process of searching, vetting, and interviewing physicians is exhausting and time-consuming, creating a frustrating barrier to the very care you’re seeking.
Instead of trying to navigate this landscape alone, a curated network offers a direct, trusted path. Think of it as bypassing the endless, uncertain results of a Google search and instead being handed a private list of pre-approved experts. A platform like Haute MD was designed for exactly this purpose, serving as a definitive resource for discerning patients who refuse to compromise on their health. It transforms a frustrating search into a confident choice.
The Power of a Rigorous Vetting Process
Let’s be honest: not all doctors are created equal. And not every physician offering premium services actually meets the highest standards of excellence. The real value of a curated network lies in its meticulous vetting protocol. Only distinguished, board-certified doctors of internal medicine who demonstrate an unwavering commitment to patient outcomes are even invited to join.
This isn’t a simple check-the-box exercise. The selection process is built on several pillars of quality:
- Board Certification: Verifying active certification with respected bodies like the American Board of Internal Medicine (ABIM) is the absolute baseline.
- Professional Standing: We look for physicians with stellar peer recognition, leadership roles in their field, and meaningful contributions to medicine.
- Patient Experience: The focus is on physicians known for delivering white-glove service and, most importantly, building strong, lasting relationships with their patients.
This process ensures that every connection you make is with a practitioner at the absolute top of their game. It removes the guesswork and the risk, giving you peace of mind that you’re engaging with a true leader in adult medicine.
A curated directory isn’t just a list; it’s a seal of approval. It signifies that a physician has not only met but exceeded the rigorous standards required for inclusion, ensuring you connect only with the best.
The experience itself is designed for simplicity and precision. You can easily search by location or subspecialty to find leading internists who already specialize in concierge care, executive health, or advanced longevity science. This focused approach connects you directly with physicians operating at the pinnacle of personalized medicine. It’s not about finding a doctor; it’s about finding your doctor—one who is vetted, trusted, and perfectly aligned with your health ambitions.
Common Questions, Answered
When you’re making decisions about your health, you need clear answers. Here are a few of the most common questions that come up when considering an internal medicine doctor.
What’s the Real Difference Between an MD and a DO Internist?
Both MDs (Doctors of Medicine) and DOs (Doctors of Osteopathic Medicine) are fully licensed physicians. They complete the exact same demanding three-year internal medicine residency after medical school and are held to the same high standards of care.
The main distinction goes back to their initial medical school philosophy. DOs get extra training in a hands-on diagnostic and treatment method called osteopathic manipulative treatment (OMT). In the real world of an internal medicine practice, though, their approaches are nearly identical, focusing on evidence-based medicine. The choice really just boils down to personal preference.
Do I Need a Referral to See a Doctor of Internal Medicine?
This depends entirely on two things: your insurance plan and the doctor’s practice model.
- PPO Plans: Usually, no. PPO plans are designed to give you the flexibility to see specialists, including internists, without a referral.
- HMO Plans: Almost always, yes. HMOs operate with a “gatekeeper” model, meaning you’ll need a referral from your main primary care doctor first.
- Concierge & Executive Health: Almost never. These models operate outside the typical insurance hoops, allowing you to self-refer and contact the practice directly for an appointment.
What Kinds of Conditions Do Internists Typically Treat?
Think of an internist as the master diagnostician and manager for adult health. Their training is laser-focused on the enormous range of conditions affecting adults, from long-term chronic diseases to sudden, acute illnesses.
They’re the experts you see for managing things like hypertension (high blood pressure), diabetes, heart disease, and asthma. But they’re also the ones who quarterback your care when you have a complex infection or the flu, especially if you’re juggling multiple health conditions at once.
An internist’s deep training in adult medicine makes them uniquely qualified to manage the full spectrum of conditions, from prevention and wellness to the intricate management of multi-system chronic diseases.
Can an Internist Actually Be My Primary Care Physician?
Yes, absolutely. In fact, a general internist is one of the three core specialties—along with family doctors and pediatricians—recognized as a primary care physician (PCP).
Many successful adults specifically seek out an internist for their primary care. Why? Because their deep, focused knowledge of adult medicine is invaluable for building proactive health strategies and managing the complexities that can arise as we age.
Finding the right expert is the most critical step in taking control of your health. Haute MD simplifies this search by providing direct access to a vetted network of the nation’s leading doctors of internal medicine and other specialists who are leaders in their fields. Explore our curated network to connect with a top-tier physician near you. Find your specialist on Haute MD.

