Navigating the world of primary care often feels more complicated than it should be, especially when you’re trying to choose between an internist and a general practitioner. At first glance, the roles seem similar, but the core difference between internal medicine and a general practitioner lies in their patient focus.
Simply put, internists are specialists exclusively trained to handle the complex medical needs of adults, while GPs offer comprehensive care for the entire family, from infants to seniors. This fundamental distinction is the starting point for building a personal health strategy that truly aligns with your needs.
Foundational Differences in Primary Care
Deciding between an internist and a general practitioner (GP) goes far beyond their basic definitions. It requires a deeper look into the nuances of their training, the scope of their practice, and the specializations that directly shape the care you receive. The physician you choose will become the expert guiding your long-term health, so it’s a decision worth making thoughtfully.

This guide will walk you through these key differences, helping you select a physician who is the right fit—whether you’re managing multiple complex conditions, focusing on longevity, or simply seeking a single trusted doctor for your whole family. Making an informed choice is the first real step toward a strong and effective doctor-patient relationship.
Key Differences at a Glance
Sometimes, the most direct way to understand two specialties is to see them side-by-side. While both internists and GPs are excellent primary care providers, their approach and patient demographics are fundamentally different.
The decision often comes down to this: An internist provides deep, specialized expertise in adult medicine, while a general practitioner offers broad, continuous care for every member of the family, across all stages of life.
To make this comparison crystal clear, we’ve put together a table summarizing the essential differences between these two medical professionals.
Key Differences Internal Medicine vs General Practitioner
| Attribute | Internal Medicine (Internist) | General Practitioner (GP) |
|---|---|---|
| Patient Age | Exclusively adults (typically 18+) | All ages (infants to seniors) |
| Training Focus | Three-year residency focused solely on adult diseases, from common to complex. | Residency in family medicine, covering pediatrics, obstetrics, and adult care. |
| Scope of Practice | Deep expertise in diagnosing and managing complex adult illnesses and chronic conditions. | Broad-spectrum care including routine check-ups, preventive services, and acute care for the whole family. |
| Ideal for Patients | Adults with multiple chronic conditions or those seeking focused adult preventive health. | Families seeking a single physician for all members, from children to grandparents. |
This at-a-glance comparison helps frame the choice based on your specific life stage and health needs.
For those looking to explore their options further, you might be interested in our guide on finding top general medicine doctors that align with your health goals.
How Physician Training Defines Medical Expertise
A doctor’s residency is the crucible where their entire clinical philosophy is forged. Those intense, multi-year programs after medical school are what truly shape how a physician approaches patient care, and it’s where the fundamental difference between internal medicine and a general practitioner is born. If you want to choose the right primary care physician, you have to understand their distinct training paths.
At the core of an internist’s expertise is a demanding, three-year residency focused exclusively on adult medicine. This isn’t a brief overview; it’s a deep dive into the staggering complexities of the adult body, from common ailments to the intricate management of multiple chronic diseases.
The Internist’s Path: A Deep Specialization in Adult Health
Internists spend their training completely immersed in the world of adult health. They learn to diagnose and manage conditions like heart disease, diabetes, hypertension, and autoimmune disorders with a specialist’s eye. More importantly, they become experts in untangling the knotty problems of patients with multiple, overlapping health issues, navigating complex diagnostic puzzles and sophisticated treatment plans.
This singular focus on adults is what molds them into what many call “the doctor’s doctor”—a sharp diagnostician with a profound understanding of adult physiology. Their training is often heavy on hospital time, managing acutely ill patients in critical care units and on general medical wards. That experience is invaluable, giving them the skills to handle serious health crises and ensure seamless care from the clinic to the hospital and back.
The philosophy of internal medicine training is depth over breadth. By concentrating solely on adults, internists develop an exceptional level of expertise in preventing, diagnosing, and managing the conditions that primarily affect the adult population.
The General Practitioner’s Path: A Foundation in Family Care
In sharp contrast, a general practitioner’s training—typically a residency in family medicine—is designed for breadth. While it also lasts three years, the curriculum is intentionally diverse. The goal is to prepare GPs to be the go-to primary care providers for the entire family unit, from newborn to grandparent.
Their residency is a whirlwind of rotations through a wide array of fields:
- Pediatrics: Caring for infants, children, and adolescents.
- Obstetrics and Gynecology: Providing prenatal care and managing women’s health.
- Adult Medicine: Handling common health problems in adults.
- Minor Surgery: Performing various in-office procedures.
This broad-spectrum education gives GPs incredible versatility to handle almost any medical concern a family might face, across all life stages. They are trained to be the first point of contact, building long-term relationships and viewing a patient’s health within the full context of their family and community.
In the United States, these two specialties are the pillars of primary care. Data from 2019 showed that of roughly 228,000 primary care physicians, family medicine (general practice) accounted for 39.8%, while general internal medicine made up 34.5%. This balance underscores the vital and distinct roles both specialties play in the nation’s health.
Ultimately, the training paths diverge to serve very different patient needs. If you’re an adult seeking a physician with specialized, in-depth knowledge of adult disease, learning more about the role of doctors of internal medicine is a smart move. This distinction in education is the single most significant factor defining their medical expertise.
3. Clinical Settings: Where They Practice and Why It Matters
A doctor’s training doesn’t just dictate what they treat; it fundamentally shapes where and how they practice. This distinction in the clinical environment is one of the most practical differences between an internist and a general practitioner, especially when your health takes an unexpected turn.
Internists are masters of two domains: the outpatient clinic and the hospital. This unique flexibility is a direct outcome of their intensive training in complex adult diseases. In their private practice or clinic, an internist is your long-term strategist, managing chronic conditions, performing deep-dive physicals, and mapping out preventive health plans for adult patients.

But here’s the critical advantage: when one of their patients gets sick enough to be hospitalized, many internists can follow them inside. Acting as a hospitalist, they continue to manage that patient’s care. This continuity is invaluable, ensuring the one physician who knows your entire health history is steering the ship during your most vulnerable moments.
The Internist: A Natural Fit for Concierge and Executive Health
The internist’s deep expertise in adult medicine makes them the ideal physician for high-touch care models like executive health and concierge medicine. These environments are built around proactive, in-depth care for adults—precisely the cornerstone of internal medicine.
In a concierge setting, an internist has the time and resources to elevate the standard of care significantly:
- Proactive Longevity Planning: They move beyond routine check-ups to architect detailed, personalized strategies for health optimization and long-term wellness.
- In-Depth Diagnostics: With longer appointments, they can thoroughly investigate complex symptoms and subtle health shifts that might otherwise be overlooked.
- Seamless Specialist Coordination: They act as the quarterback for your health, managing referrals and ensuring fluid communication with top-tier specialists like cardiologists or oncologists.
This meticulous, partnership-based approach is exactly what discerning patients demand. It’s a completely different world from conventional primary care, a difference we explore in our guide on concierge medicine vs. traditional healthcare.
The General Practitioner: The Community Healthcare Hub
General practitioners, by contrast, almost exclusively practice in outpatient, community-based clinics. Their entire model is engineered to be the accessible, central point of contact for a family’s day-to-day healthcare needs, and their greatest strength lies in this incredible breadth.
A general practitioner’s clinic is built for accessibility and comprehensive family service. It’s the place you go for everything from a child’s flu shot to a grandparent’s blood pressure check, emphasizing broad-spectrum care over deep specialization.
The scope of a GP’s practice is necessarily wide to serve this diverse patient base. A typical day could easily involve:
- Administering pediatric immunizations.
- Performing a routine prenatal check-up.
- Conducting a well-woman exam.
- Managing a senior’s stable chronic conditions.
- Treating acute illnesses like strep throat or suturing minor injuries.
This model makes GPs an indispensable asset for families who want a single, trusted physician for everyone, at every age. Their clinical environment is optimized for volume and variety, handling the everyday health needs of the entire community. While they are exceptionally skilled, their setting and focus aren’t designed for the intensive, adult-focused diagnostic dives that define an internist’s practice—a direct reflection of their distinct training philosophies.
Understanding Subspecialties and Referral Networks
There’s a reason internists are often called the “doctor’s doctor.” The title isn’t just a clever phrase; it’s a direct reflection of their deep, specialized training in adult medicine, which serves as a natural launchpad for further specialization. Grasping this career trajectory is crucial to understanding a major difference between internal medicine and a general practitioner.
An internist’s residency is an exhaustive deep dive into the complexities of adult physiology and disease. This intensive grounding allows them to transition seamlessly into highly specialized fellowship programs, where they become true experts in specific organ systems or disease categories. This built-in pathway to subspecialization is a defining feature of internal medicine.
The Internist’s Subspecialty Pathways
After finishing a demanding three-year residency, a significant number of internal medicine physicians pursue what’s known as a fellowship. This involves another one to three years of rigorous training in a chosen field, transforming them from a general internist into a subspecialist.
This creates a powerful, tightly woven network. Even an internist who functions as a primary care physician (PCP) possesses an intricate understanding of these advanced fields and the experts who practice in them.
Common subspecialties branching from internal medicine include:
- Cardiology: Focusing on the heart and circulatory system.
- Endocrinology: Specializing in hormonal disorders, metabolism, and diabetes.
- Gastroenterology: Concentrating on the digestive system and related conditions.
- Oncology: Diagnosing and treating cancer.
- Pulmonology: Dealing with lung diseases and complex respiratory issues.
Because of this shared foundation, when an internist refers you to a specialist, it’s often to a colleague whose clinical approach and training they know intimately. The referral isn’t a blind handoff; it’s a highly informed, collaborative move within a shared ecosystem of adult medical expertise. This results in incredibly efficient, targeted care—especially for patients managing complex, multi-system health problems.
This trend toward specialization isn’t just anecdotal. Data from the career choices of internal medicine residents reveals a stark reality: only a small fraction, roughly 20-25%, choose to practice as generalists. A landmark study published in JAMA found that just 22.0% of U.S. medical graduates and 21.1% of international graduates in internal medicine intended to pursue careers in general internal medicine, underscoring the powerful pull of subspecialty training.
The General Practitioner’s Broader Network
A general practitioner’s referral network, by design, is far broader and more diverse. Since their training spans the entire human lifespan—from newborns to the elderly—their referral patterns have to cover that same vast territory. Their professional circle isn’t confined to adult specialists; it encompasses the full spectrum of medical care for every member of a family.
On any given day, a GP might refer:
- An infant with a heart murmur to a pediatric cardiologist.
- A teenager with a sports injury to an orthopedic surgeon.
- An expectant mother to an OB/GYN for specialized prenatal care.
- An older adult showing signs of cognitive decline to a geriatrician.
The core difference in referral networks comes down to depth versus breadth. An internist’s network is a deep well of adult-focused specialists, facilitating precise coordination for complex adult diseases. A GP’s network is a wide web designed to support the varied health needs of an entire family across all ages and life stages.
This makes GPs exceptional coordinators of family-wide healthcare, ensuring every person gets to the right specialist at the right time. For an adult managing multiple chronic conditions, however, the internist’s highly integrated, adult-centric network offers a distinct advantage in navigating intricate health challenges with precision.
Making the Right Choice for Your Health Goals
Choosing a primary care physician isn’t just about finding someone to call when you’re sick. It’s a strategic decision that directly shapes your long-term health trajectory. Once you move past the textbook definitions, the practical choice between an internist and a general practitioner really boils down to your personal health context, your current life stage, and your future goals.
The best doctor isn’t the one with the most credentials, but the one whose expertise aligns perfectly with your needs. This isn’t about which doctor is “better,” but which one is the better fit for you. By breaking down specific scenarios and knowing what to ask, you can confidently make the right call.
When to Choose an Internist
Think of an internist as the specialist in adult medicine. They are the ideal choice for adults who require deep, focused medical expertise. Their training is laser-focused on the complexities of adult physiology, which makes them uniquely equipped for a few key situations.
You should seriously consider an internist if your health profile looks like this:
- You’re Managing Multiple Chronic Conditions: If you’re juggling two or more chronic illnesses—like diabetes, heart disease, and hypertension—an internist is an expert at managing the overlap. They excel at handling complex medication regimens and coordinating care to head off complications before they start.
- You’re Focused on Longevity and Proactive Health: For high-achievers prioritizing peak performance and longevity, an internist offers a strategic advantage. Their in-depth knowledge of adult-onset diseases allows them to build sophisticated preventive plans aimed at early detection and aggressive risk mitigation.
- You Have a Complex or Undiagnosed Illness: Internists are renowned diagnosticians. If you have puzzling symptoms that have been tough to pin down, their methodical and deep diagnostic approach can be invaluable in finally uncovering the root cause.
- You Prefer a Concierge or Executive Health Model: The high-touch, in-depth care model of concierge medicine is a natural fit for an internist’s skillset. This environment provides the time and resources needed for the comprehensive, personalized care that complex adult health demands.
An internist acts as a specialist in adult primary care. Their value shines brightest when managing intricate health puzzles, architecting long-term wellness strategies, and providing continuous care for serious illnesses from the clinic to the hospital.
This decision tree shows the distinct career and referral pathways that stem from these different training philosophies.
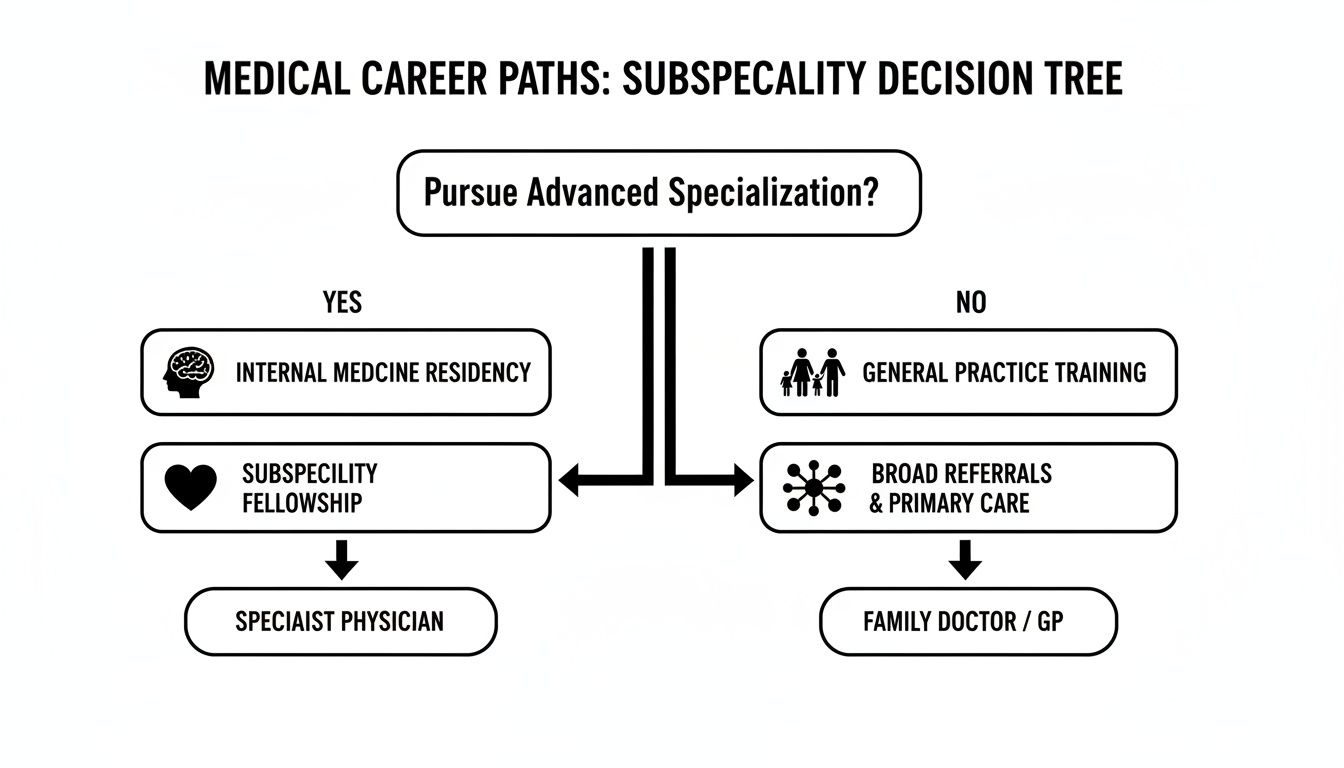
The visual makes it clear: internal medicine is a direct gateway to advanced subspecialties, while general practice provides a broad foundation for coordinating care across the entire family.
When to Choose a General Practitioner
A general practitioner (GP), often called a family medicine doctor, offers incredible value through their sheer versatility and focus on the family unit. Their broad training prepares them to be the central point of contact for a massive range of medical needs across all ages.
A GP is likely the right choice for you in these circumstances:
- You Need a Single Doctor for Your Entire Family: This is the ultimate convenience. Having one trusted physician for your children, your spouse, and yourself creates seamless family health management and gives you a doctor who truly understands your family’s collective health history and dynamics.
- You Are Generally Healthy and Need Routine Care: For adults without complex chronic conditions, a GP is perfectly equipped to handle annual physicals, preventive screenings, and treatment for common acute illnesses like the flu or minor injuries.
- You Want a Doctor to Grow with Your Family: A GP builds relationships for the long haul, often caring for children through adolescence and well into their adult years. This continuity of care is a hallmark of family medicine and provides a consistent, trusted source of medical guidance through every life stage.
Questions to Ask Yourself Before Deciding
To lock in your decision, take a moment to reflect on your priorities. Your honest answers here will point you toward the physician who makes the most sense for your unique situation.
- What is my current health status? Do I have one or more chronic conditions that demand specialized management, or am I primarily focused on maintaining general wellness?
- What are my long-term health goals? Am I trying to optimize my health for peak performance and longevity, or is my main priority consistent, reliable care for routine issues?
- What does my family look like? Is the convenience of a single doctor for myself, my partner, and my children a top priority?
- How important is hospital continuity to me? Do I want a physician who can potentially manage my care from their office straight through to a hospital admission if I become seriously ill?
By thoughtfully considering these points, you can align your specific needs with the distinct strengths of either an internist or a general practitioner. This ensures you’re building a lasting and effective partnership for your health.
Common Questions About Choosing Your Primary Care Physician
When it comes to the practical choice between an internist and a general practitioner, a few key questions always come up. Getting straight answers here is the final step in feeling confident you’ve picked the right doctor for your specific health goals and lifestyle.
Can an Internist Be My Primary Care Physician?
Yes, absolutely. An internist isn’t just qualified to be a primary care physician (PCP)—they represent an ideal choice for many adults. Their entire training is a deep dive into adult medicine, making them specialists in preventing, diagnosing, and managing the health conditions that impact adults, from common illnesses to complex, chronic diseases.
For anyone serious about long-term wellness, an internist brings a level of knowledge specifically matched to adult physiology. Think of them as a specialist in adult primary care.
I Am Healthy in My 30s. Do I Really Need an Internist?
While a GP is a perfectly capable choice for a healthy adult, choosing an internist can be a strategic, forward-thinking move. An internist’s training is intensely focused on the prevention and earliest possible detection of adult-onset diseases like hypertension, diabetes, and heart disease.
For high-performers who prioritize longevity and peak health, starting with an internist early on helps establish a crucial health baseline. This isn’t just a check-up; it’s the beginning of a long-term partnership with a physician whose expertise is precisely aligned with where your health journey is headed over the next few decades.
Choosing an internist in your 30s is an investment in proactive, specialized adult health. It shifts the focus from reactively treating problems to building a strategic plan for lifelong wellness and disease prevention.
If I Choose an Internist, Who Will Treat My Children?
This is a critical distinction: internists exclusively treat adults, typically patients aged 18 and over. Their residency training does not cover pediatrics, so they aren’t equipped to manage the unique health needs of infants, children, or adolescents.
If you select an internist as your PCP, your children will need their own doctor, like a pediatrician or a family medicine physician. If having a single doctor for every member of the family is your top priority, then a General Practitioner is the more practical choice.
Are Concierge Doctors Usually Internists or GPs?
While you’ll find physicians from both backgrounds in concierge medicine, the model is a natural fit for internists. The entire framework of concierge care—which prioritizes personalized, in-depth service and a strong doctor-patient relationship—aligns perfectly with internal medicine’s focus on complex adult health and proactive disease management.
This model gives internists the time they need to dive deep with each patient, which is essential for crafting the comprehensive executive health plans and longevity strategies that discerning patients demand. This structure truly supports the meticulous, diagnostic-heavy approach that defines the difference between internal medicine and a general practitioner.
Finding a physician whose expertise truly matches your health ambitions is the single most important step in building a proactive wellness strategy. At Haute MD, we connect discerning patients with the nation’s leading, board-certified physicians in internal medicine, concierge care, and longevity. Discover a vetted provider ready to partner with you on your health journey by exploring our exclusive network.

