That phantom burning feeling on your skin is a deeply unsettling signal that something is wrong, even when there’s no obvious burn or injury. It’s not in your head. This sensation is a real physiological message, and figuring out its origin is the first step toward relief. The problem almost always boils down to one of two things: an issue with the skin itself (dermatologic) or a problem with the nerves that send signals from the skin (neuropathic).
Understanding That Burning Feeling On Your Skin

The sensation of burning skin without an actual heat source can be confusing and alarming. Think of it like a faulty fire alarm system in your body.
Sometimes, the alarm is accurate—there’s a real fire. This is the dermatologic side of the problem, where something is directly irritating or damaging your skin, like a chemical exposure or a severe rash.
Other times, the alarm is triggered by faulty wiring. This is the neuropathic side. The nerves responsible for sensing temperature and pain are misfiring, sending “burn” signals to your brain even when your skin is perfectly fine. This distinction is everything, because you wouldn’t use a fire hose to fix an electrical short.
Two Primary Pathways to a Burning Sensation
A burning feeling on the skin almost always originates from one of these two sources. Disentangling them is the primary goal when you see a specialist.
- Dermatologic Causes: This is a problem with the skin. The issue is often visible, showing up as redness, rashes, blisters, or inflammation. It’s a direct cause-and-effect scenario where an irritant, allergen, or skin disease has compromised the skin’s barrier.
- Neuropathic Causes: This is a problem with the nerves. The skin can look completely normal, yet it feels like it’s on fire. This happens when nerves are damaged, compressed, or affected by a systemic condition like diabetes or an autoimmune disorder.
The key takeaway is that your symptom is real, even if the cause isn’t visible. A burning sensation without a rash is a classic sign that the issue may lie deeper than the skin’s surface, often pointing toward a nerve-related problem that requires specialized investigation.
Why You Should Never Ignore This Symptom
A minor sunburn will heal, but a persistent or unexplained burning skin sensation is a signal you shouldn’t dismiss. It can be the first clue to an underlying condition that needs real attention. For example, it’s often one of the earliest indicators of nerve issues stemming from conditions like diabetes or certain vitamin deficiencies.
Ignoring these signals is like ignoring your car’s check engine light—the problem rarely fixes itself and can become far more serious over time. Acknowledging that this sensation is a legitimate medical symptom is the first step. From there, a clear path toward diagnosis and relief can begin, guided by an expert clinical evaluation.
Exploring the Causes Behind Burning Skin
Figuring out what’s causing a burning skin sensation is a bit like detective work. The feeling itself is your first clue, but the real culprit could be hiding in one of two places: the skin itself (dermatologic) or the complex network of nerves running beneath it (neuropathic).
This distinction is everything. A dermatologic cause means something is actively irritating or damaging your skin’s surface. A neuropathic cause, on the other hand, points to a malfunction in your body’s electrical wiring. Getting this right is the only path to finding a real solution.
And if you’re experiencing this, you’re far from alone. The feeling of sensitive skin is incredibly common. Major studies show that roughly 60-70% of women and 50-60% of men report some degree of skin sensitivity, which often includes that burning feeling.
When the Problem Is on the Surface
Dermatologic causes are often the most straightforward to pin down because they usually leave visible evidence—a rash, redness, or obvious injury. The burning is a direct, logical response to damage or inflammation of the skin barrier.
- Contact Dermatitis: This happens when your skin touches something that either irritates it (irritant contact dermatitis) or triggers an allergy (allergic contact dermatitis). Think of culprits like harsh soaps, cleaning agents, fragrances, metals like nickel, or plants like poison ivy. The result is almost always a red, itchy, and burning rash.
- Thermal or Chemical Burns: This is the most obvious cause—direct injury from heat (like a hot stove) or exposure to harsh chemicals. This kind of damage to the skin layers triggers immediate pain and a persistent burning sensation as your body rushes to heal.
- Sunburn: A classic first-degree burn. The UV radiation damages your epidermis, the skin’s outermost layer. Your body’s inflammatory response kicks in, leading to the familiar redness, heat, and painful burn.
When the Signal Is the Problem
Neuropathic causes are much trickier. In these cases, the skin can look perfectly normal, which can be confusing and frustrating. The burning sensation isn’t coming from skin damage but from nerves firing off faulty pain signals to the brain.
Imagine it like static on a phone line. The line itself is fine, but the message gets garbled, turning a normal sensation—or no sensation at all—into a painful one.
A key indicator of a potential neuropathic cause is a burning sensation that occurs without any visible rash, redness, or injury. This “invisible” symptom strongly suggests the problem lies within the nervous system.
This is precisely where a specialist’s evaluation becomes non-negotiable, as these conditions require a completely different diagnostic playbook.
Deeper Neuropathic and Systemic Causes
Several specific conditions are notorious for creating this phantom burning by directly affecting the nerves.
- Shingles (Herpes Zoster): This is caused by the reactivation of the chickenpox virus. It creates an intensely painful, burning rash, usually in a stripe on one side of the body. The virus lies dormant in nerve tissue for years, and when it wakes up, it travels along nerve pathways to the skin, causing that signature fiery pain.
- Small-Fiber Neuropathy (SFN): This condition involves damage specifically to the tiny nerve fibers in your skin that are responsible for sensing temperature and pain. SFN is famous for causing burning, tingling, or “pins-and-needles” feelings, often starting in the feet and hands. It can be linked to diabetes, autoimmune disorders, or sometimes appears with no known cause.
- Erythromelalgia: A rare but dramatic condition marked by intense, episodic burning pain, redness, and swelling, most often in the feet and hands. These flare-ups can be triggered by warmth or exercise and are thought to stem from issues with both blood vessels and nerves.
- Burning Mouth Syndrome: Just as the name suggests, this condition creates a chronic burning or scalding feeling in the mouth, lips, or tongue without any clear medical or dental reason. It’s considered a neuropathic pain disorder.
- Autoimmune Conditions: Diseases like lupus or rheumatoid arthritis can trigger systemic inflammation that sometimes targets nerves, leading to burning sensations. If you suspect your symptoms might be part of a bigger picture, reviewing an autoimmune symptoms checklist can give you valuable context before speaking with your doctor.
How Doctors Diagnose Your Burning Sensation
Moving from a mysterious burning skin sensation to a clear diagnosis isn’t guesswork. It’s a meticulous, evidence-based process where your doctor acts like a detective, piecing together clues from your personal story and advanced clinical tools. This systematic investigation is what demystifies your symptoms and paves the way for effective treatment.
The entire journey begins with a detailed conversation. This initial discussion is the foundation, guiding every subsequent test and examination to ensure the investigation is focused and efficient.
The Critical Role of Your Medical History
Your doctor will want to understand the full context of what you’re experiencing. Every detail you provide is a valuable clue, so be prepared to discuss a few key things.
- Symptom Onset and Timeline: When did the burning start? Was it a sudden fire, or a slow smolder that grew over time?
- Location and Pattern: Is the sensation stuck in one spot, or does it move around? Is it happening on both sides of your body symmetrically?
- Triggers and Relievers: Does anything make it worse, like heat, a light touch, or even stress? Does anything bring relief, like a cool compress or simply resting?
- Associated Symptoms: Are you also dealing with numbness, tingling, weakness, or is there a visible rash?
This storytelling phase is absolutely crucial. Think about it: a burning sensation that neatly follows the path of a single nerve tells a very different story than one that erupts with a blistering rash after you tried a new laundry detergent.
Your personal account is the most powerful diagnostic tool. The details you provide about your experience—when it started, what it feels like, and what makes it change—create a roadmap that helps your physician narrow down the possibilities from dozens to a select few.
This infographic helps visualize that initial fork in the road—the first big question is whether the problem originates in the skin or the nerves.
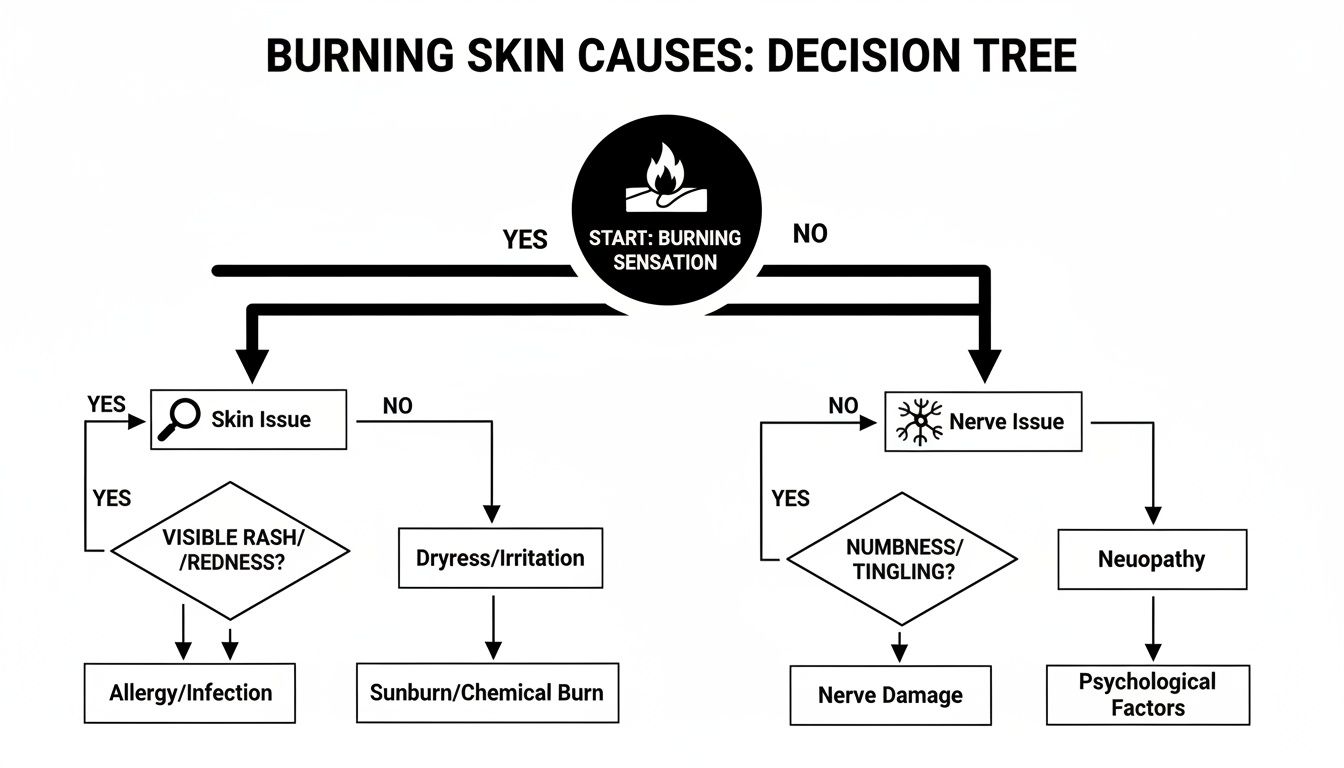
As you can see, the presence or absence of a visible skin issue is often the first major branch in the diagnostic journey.
Advanced Diagnostic Tools and Tests
After gathering your history and performing a thorough physical exam, your specialist may need more data to confirm what they suspect. This is where advanced tools come in, allowing them to look beneath the surface for objective evidence.
The table below outlines some of the most common diagnostic tools used to get to the bottom of a burning sensation, helping to distinguish between a skin problem and a nerve problem.
| Diagnostic Tool | Primary Purpose | What It Reveals |
|---|---|---|
| Blood Tests | To screen for systemic issues. | Uncovers underlying conditions like diabetes, vitamin deficiencies (B12, B6), thyroid problems, or markers of autoimmune disease. |
| Nerve Conduction Studies (NCS) / Electromyography (EMG) | To assess large nerve function. | Measures the speed and strength of electrical signals in your nerves, identifying damage to the larger “wiring.” |
| Skin Biopsy for Nerve Fiber Density | To diagnose small-fiber neuropathy. | Directly counts the number of tiny nerve endings in a skin sample. A low count is the gold standard for confirming small-fiber damage. |
These tests provide the hard data needed to move from a suspected cause to a confirmed diagnosis, ensuring that the subsequent treatment plan is targeting the true source of the problem.
Let’s break down how these tools are used.
1. Blood Tests A simple blood draw can reveal a surprising amount about what’s happening inside your body. It helps uncover systemic issues known to cause nerve-related burning. Key markers include blood sugar levels to check for diabetes, vitamin levels (B12 and B6 are common culprits), thyroid hormones, and specific antibodies that point to autoimmune conditions.
2. Nerve Conduction Studies (NCS) and Electromyography (EMG) If a larger nerve issue is suspected, these tests measure how well your nerves transmit electrical signals. Think of it as an electrician checking the wiring in a house. An NCS can determine if nerve damage is slowing down signals, while an EMG checks the health of the muscles controlled by those nerves.
3. Skin Biopsy for Nerve Fiber Density When the symptoms point toward small-fiber neuropathy, a skin biopsy is the definitive test. A tiny punch biopsy, usually from the ankle, allows a pathologist to count the number of small nerve fibers present. A reduced number is concrete proof of damage to these delicate sensory nerves.
Occasionally, a burning sensation is tied to less common conditions like Mast Cell Activation Syndrome (MCAS), where immune cells go haywire and release inflammatory chemicals. If your symptoms are widespread and involve multiple body systems, you might want to learn how to find a mast cell specialist near you for a highly specialized evaluation.
Ultimately, this multi-step approach ensures nothing is missed. By combining your story with objective data from targeted tests, your physician can pinpoint the precise cause of your burning skin sensation and build a treatment plan that addresses the root of the problem—not just the symptoms.
Finding Lasting Relief with Advanced Treatments
Once a skilled clinician pinpoints the root cause of your burning skin sensation, the mission shifts entirely to finding a real, lasting solution. Modern medicine isn’t about throwing darts in the dark; it’s about deploying evidence-based treatments designed to calm both irritated skin and haywire nerves. The goal is never a one-size-fits-all fix but a precision-guided plan that targets the specific mechanism driving your discomfort.
This journey toward relief often begins with treatments applied directly to the skin, giving you localized control right where you feel the burn.
Targeted Topical Therapies
For many, the first line of defense is a topical agent that works on the skin’s surface to intercept pain signals before they can even reach the brain. Think of them as a highly specialized fire crew, sent directly to extinguish the blaze.
Two of the most reliable options are:
- Capsaicin Cream: This isn’t just folk medicine; it’s science. Derived from chili peppers, capsaicin works by depleting a chemical called Substance P, a key messenger for pain. At first, it might create a mild warming sensation of its own, but with consistent use, it brilliantly desensitizes the nerve endings, effectively turning down the volume on those burning signals.
- Lidocaine Patches or Creams: Lidocaine is a local anesthetic that acts like a temporary roadblock for nerve signals in the skin. Applying a patch or cream creates a numbing effect right over the painful area, offering predictable and targeted relief for localized burning.
These topicals are often the go-to, especially when the burning is contained to a specific area. But when the problem is more widespread or originates deeper within the nervous system, it’s time for a different strategy.
Systemic Medications for Neuropathic Pain
When the burning comes from faulty nerve “wiring” throughout the body—as we see in small-fiber neuropathy—we need medications that can calm the entire system from the inside out. These oral medications work on the central nervous system to reduce the intensity of the rogue pain signals being sent to your brain.
The most effective neuropathic treatments don’t just mask the pain; they work to correct the underlying nerve hyperexcitability. This is like turning down the sensitivity of a smoke detector that’s been set off by steam instead of an actual fire.
The main classes of medications used for this purpose include:
- Gabapentinoids (Gabapentin and Pregabalin): These are often the heavy hitters for neuropathic pain. They work by telling overactive nerve cells to calm down, making them far less likely to send those spontaneous and exaggerated pain signals.
- Tricyclic Antidepressants (Amitriptyline, Nortriptyline): Don’t let the name fool you. While originally developed for depression, these medications are incredibly effective at low doses for nerve pain. They work by tweaking the levels of certain brain chemicals involved in how we perceive pain.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) (Duloxetine, Venlafaxine): Similar to tricyclics, these medications also modify neurotransmitter levels, helping to dampen pain signals as they travel up the spinal cord to the brain.
Finding the right medication and the perfect dose is a careful process of trial and adjustment, always guided by a specialist to get you the most relief with the fewest possible side effects.
Cutting-Edge and Immunomodulatory Treatments
For complex or stubborn cases, especially those tied to autoimmune conditions or severe nerve damage, more advanced interventions might be on the table. These therapies are designed to tackle the underlying disease process or provide more powerful, direct pain relief.
- Immunomodulatory Treatments: If an autoimmune disease is attacking your nerves, the strategy shifts to calming the overactive immune response. Treatments like corticosteroids, intravenous immunoglobulin (IVIg), or other immune-suppressing agents can stop the nerve damage at its source.
- Procedural Options: For severe, localized nerve pain that doesn’t respond to other treatments, nerve blocks or spinal cord stimulation can be life-changing. These procedures physically interrupt the pain pathway, preventing the signals from ever reaching the brain.
The sheer prevalence of uncomfortable skin sensations highlights just how urgent the need for these treatments is. A massive study across Europe found that over 94 million individuals complain of sensations like burning, itching, or dryness. You can read more about these findings on dermatological conditions and see just how common this issue is.
Navigating these options requires a skilled specialist. A board-certified dermatologist, for instance, is an expert not just in skin-level issues but also in the complex dance between the skin and the nervous system. Understanding what a dermatologist treats clarifies why they are so often central to solving the puzzle of a burning skin sensation. A personalized plan from an expert is your surest path to tangible, long-term results.
When You Should Seek Immediate Medical Care
Most of the time, a burning skin sensation is something you can manage with a specialist’s help on a normal schedule. But some situations are different. They’re your body’s version of a fire alarm—loud, clear signals that something far more serious is happening and you need to act now.
Knowing how to spot these “red flag” symptoms isn’t about creating panic. It’s about being prepared to make the right call when every second counts. While a mild, nagging burn is cause for a scheduled appointment, the symptoms below are your cue to seek immediate medical evaluation. They could point to a fast-moving infection, an acute neurological event, or a severe systemic reaction.

Recognizing Red Flag Symptoms
If your burning skin comes with any of the following signs, don’t wait it out. This is when you head to an urgent care center or emergency room.
- Sudden Muscle Weakness or Numbness: If the burning is coupled with a sudden loss of strength, difficulty moving a limb, or numbness that seems to be spreading, it could signal a serious neurological problem like a stroke or severe nerve compression. This requires immediate intervention to prevent permanent damage.
- A Rapidly Spreading Rash with Blisters: A burning rash that is visibly expanding, especially if it’s forming blisters or open sores, might be a severe infection like cellulitis or a major allergic reaction. It’s especially urgent if the rash is anywhere near your eyes or mouth.
- Signs of a Systemic Infection: Is the burning area also swollen and hot to the touch? If you’re also running a fever, have chills, or just feel deeply unwell, it’s a strong indicator that an infection is taking hold and possibly spreading through your body.
- Difficulty Breathing or Swallowing: When a burning feeling on the face or neck is paired with shortness of breath, wheezing, or swelling of the tongue or throat, it could be anaphylaxis. This is a life-threatening allergic reaction that requires an immediate emergency response.
- Third-Degree Burn Characteristics: Look at the skin itself. If it appears charred, waxy white, or leathery—and particularly if the center of the burn has lost all feeling—you’re likely dealing with a third-degree burn. This has destroyed all layers of skin and needs specialized medical care to prevent devastating complications.
Why Acting Fast Is Crucial
In these scenarios, time is absolutely critical. Conditions like severe infections or acute neurological events can cause irreversible harm if they aren’t treated within a very narrow window.
Seeking immediate care is about preserving function and preventing long-term complications. For example, in the case of a rapidly spreading infection, early antibiotic treatment can prevent it from entering the bloodstream, a far more dangerous situation.
Do not attempt to treat these symptoms at home. This isn’t the time for ointments, ice, or home remedies, which can make things worse. Your only job is to cover the area with a clean, dry cloth and get to an urgent care center or emergency room for an expert diagnosis without delay.
Burning Skin: Your Questions Answered
Even after getting a handle on the causes and treatments for a burning skin sensation, you’re bound to have more specific questions. I’ve put together some expert-backed answers to the most common queries I hear, designed to give you concise, practical insights into this frustrating symptom.
Think of this as bridging the gap between general knowledge and what you’re actually experiencing, clarifying key ideas and tackling those nagging concerns head-on.
Can Stress Really Cause My Skin to Burn?
Absolutely. The mind-skin connection is incredibly powerful. When you’re under high stress, your body pumps out cortisol, the primary stress hormone. This can ignite inflammation system-wide and crank up the sensitivity of your nerve endings, leading to very real physical symptoms like burning, itching, or tingling—even when there’s no obvious skin issue.
While stress is rarely the single culprit, it’s a potent amplifier. If you notice your burning sensation consistently flares up during periods of high anxiety or emotional strain, that’s a major clue. It means a solid stress management strategy needs to be a core part of your relief plan.
Does a Burning Sensation Always Mean Nerve Damage?
No, and it’s a common misconception that a burning feeling automatically points to nerve damage. While neuropathic problems like small-fiber neuropathy are frequent offenders, they’re far from the only cause. A burning sensation is more like a general alarm bell from your body, and the source could be one of many things.
Think of it this way: a fire alarm doesn’t just signal a massive blaze. It could be triggered by steam from the shower or even a low battery. In the same way, burning skin can signal nerve issues, but it can also point to allergic reactions, circulatory problems, or direct skin irritation from contact dermatitis.
This is why getting a professional diagnosis is non-negotiable. You have to find the true source of the alarm to shut it off for good.
What Can I Do at Home for Some Quick Relief?
For mild, temporary relief from a burning sensation, there are a few safe and practical things you can try at home. Just remember, these are meant to provide immediate comfort and should never take the place of a proper medical evaluation, especially if your symptoms are persistent or severe.
- Apply Cool Compresses: Soak a clean cloth in cool water and lay it over the affected area for 15-20 minutes. This can help soothe irritated skin and temporarily quiet down overactive nerve endings. Steer clear of applying ice directly to the skin, as the extreme cold can sometimes make things worse.
- Wear Loose, Natural Fabrics: Tight, synthetic clothing traps heat and creates friction, which is the last thing sensitive skin needs. Opt for loose-fitting clothes made of breathable fabrics like cotton or linen to minimize irritation.
- Use a Gentle Moisturizer: Keeping your skin barrier hydrated is critical. Apply a fragrance-free, hypoallergenic moisturizer to help protect the skin and dial down the discomfort.
These at-home tactics can offer a quick fix, but they only mask the symptom. True, lasting relief starts with an accurate diagnosis from a qualified specialist who can get to the root of the problem.
Finding a specialist you can trust is the single most important step toward resolving a persistent burning skin sensation. For patients looking for premier, board-certified physicians, Haute MD provides a vetted network of the nation’s top experts in dermatology, neurology, and concierge medicine. You can connect with top-tier doctors who specialize in diagnosing and treating complex symptoms with precision and truly personalized care.
Find your specialist at Haute MD.

