When you live with asthma, the dread of not being able to breathe is a powerful, ever-present feeling. This fear isn’t just an emotion; it’s a potent trigger that can kick off a dangerous chain reaction in your body. It’s a real physiological feedback loop where your mind’s fear and your body’s reaction become so intertwined, it’s hard to tell where one ends and the other begins.
This is asthma attack anxiety: the dangerous cycle where the fear of an asthma attack triggers physical symptoms that can cause an actual attack. Breaking this cycle means tackling both the physical and mental sides of the problem head-on.
Understanding the Asthma Attack Anxiety Cycle
Think of your fear of an attack as a switch. When something flips that switch—maybe a slight chest tightness or even just a stressful thought—your body slams into “fight or flight” mode.
This stress response causes immediate, noticeable physical changes:
- Your heart starts pounding.
- Your breathing becomes shallow and fast.
- Your chest muscles clench up.
For someone without asthma, this just feels like a panic attack. But if you have asthma, these symptoms are terrifyingly similar to the start of a real asthma attack. This overlap is what gives the cycle its power. The shallow, rapid breathing can irritate your already sensitive airways, leading to genuine bronchoconstriction—the tightening of the muscles around your airways.
The Feedback Loop Explained
This is where the vicious feedback loop kicks in. The initial fear creates symptoms that feel like asthma, which then ramps up your fear, making the physical symptoms even worse. You’re left wondering, “Is this anxiety, or is it my asthma?” That uncertainty just fuels the panic.
Before you know it, the anxiety-driven symptoms can provoke a full-blown asthma exacerbation.
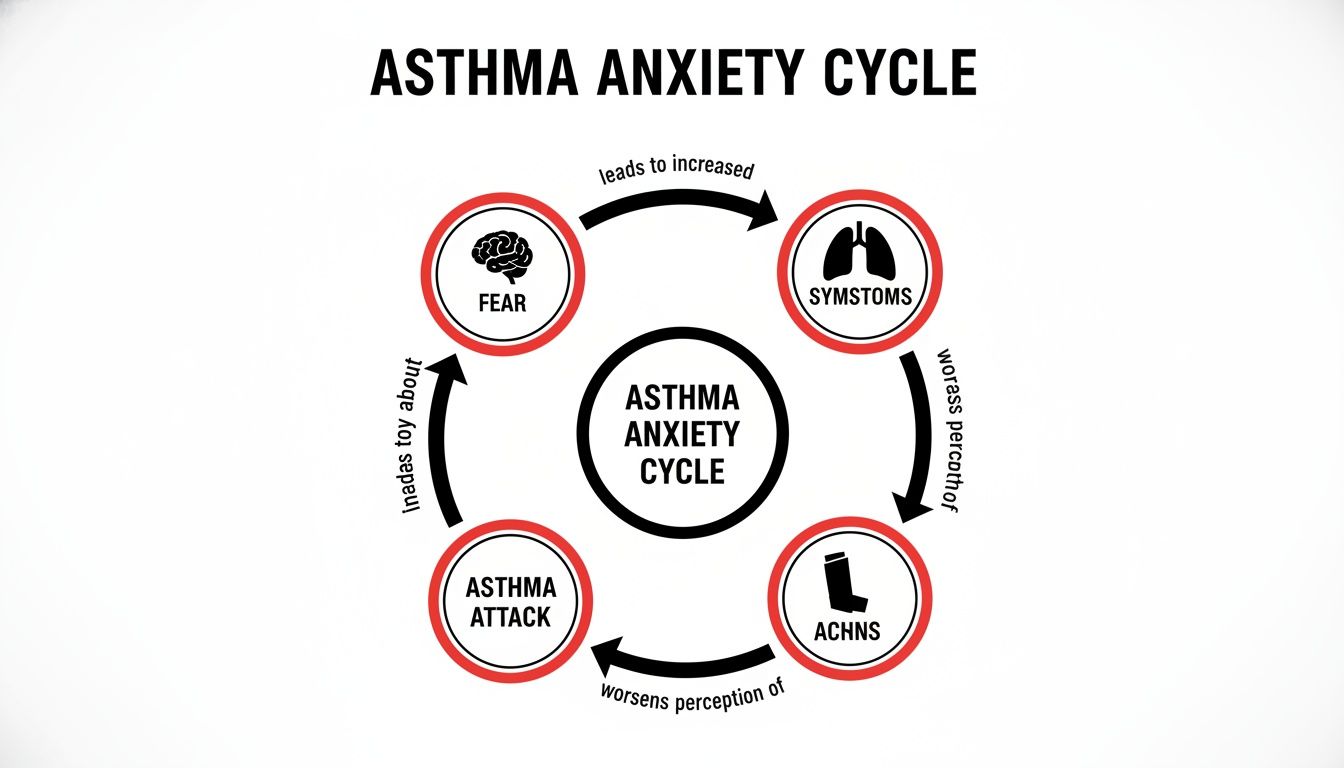
This cycle shows how a purely mental trigger (fear) can spiral into a very physical medical event (an asthma attack), highlighting just how connected they are.
The Real-World Impact on Health
This isn’t just a theory; the connection between mental health and asthma is backed by hard data. A major UK study conducted between 2017 and 2019 found that adults with asthma who also had depression or anxiety faced a 46% higher risk of severe asthma attacks.
This shows a direct, measurable link between psychological distress and how often people experience serious breathing problems. You can dig into the specifics of these asthma and anxiety findings to see the methodology for yourself.
Understanding this cycle is the first step toward regaining control. When you recognize that both your mind and body are playing a role, you can start using strategies that address both the psychological fear and the physical response, effectively breaking the chain reaction.
How Your Body Connects Panic and Breathing
To break the asthma-anxiety cycle, you have to understand why a panic attack feels so chillingly similar to an asthma attack. The answer isn’t just in your head; it’s buried deep within your body’s ancient, hardwired survival system.

Think of your body’s stress response—the famous “fight or flight” system—as a hyper-sensitive smoke detector. Its one job is to sense danger. The problem is, it can’t tell the difference between a real physical threat and a perceived one, like the spiraling fear of an impending asthma attack.
Once that alarm goes off, your brain floods your system with stress hormones like adrenaline and cortisol. These chemicals are pure action fuel, designed to prepare your body to either fight a threat or flee from it. This immediate hormonal surge is what creates the powerful, overwhelming physical sensations of panic.
The Fight or Flight Chemical Cascade
This flood of stress hormones triggers a direct and immediate chain reaction in your respiratory and muscular systems. It’s a physiological response so powerful that you can’t simply stop it with willpower.
Your body doesn’t care if the danger is a tiger in the grass or the fear of not being able to breathe. It interprets both as a genuine threat, unleashing a cascade of familiar symptoms:
- Accelerated Heart Rate: Your heart pounds faster to pump oxygen-rich blood to your muscles, getting them ready for action.
- Rapid, Shallow Breathing: Your breathing rate skyrockets to pull in more oxygen. This is great for a sprint, but terrible for sensitive airways.
- Muscle Tension: Your muscles clench and tighten, and this includes the small, delicate muscles wrapped around your airways.
This response is incredibly effective for survival, but for someone with asthma, it’s a dangerous mimic. The shallow breathing and chest tension are virtually identical to the start of an asthma episode, making it nearly impossible to tell where the anxiety ends and the asthma begins.
Bronchoconstriction The Critical Overlap
This is where the connection gets truly serious. That same stress response tensing your shoulders can also trigger bronchoconstriction—the tightening and narrowing of the very airways you rely on to breathe.
For someone with asthma, anxiety isn’t just a mental state; it’s a physical event. The stress hormones can directly cause the airways to narrow, transforming a moment of panic into a genuine breathing emergency. This physiological link is why managing asthma attack anxiety is a medical necessity, not just a mental health preference.
Your anxiety can become a direct, physical trigger for a real asthma attack. The shallow, rapid breathing that comes with panic also dries out and irritates your already sensitive airways, making them even more likely to spasm and constrict.
Telling the Difference When Symptoms Collide
In the heat of the moment, distinguishing between a panic attack and an asthma attack can feel impossible. The symptom overlap is significant. However, knowing the subtle differences can give you just enough clarity to respond correctly.
While chest tightness, a racing heart, and shortness of breath are common to both, certain signs point more clearly to one or the other.
Let’s break it down side-by-side.
Asthma Attack vs Panic Attack Symptom Overlap
This table highlights where the symptoms overlap and, more importantly, where they differ.
| Symptom | Asthma Attack | Panic Attack | Shared Symptom |
|---|---|---|---|
| Shortness of Breath | Yes | Yes | X |
| Chest Tightness | Yes | Yes | X |
| Rapid Heartbeat | Yes | Yes | X |
| Wheezing | Primary Symptom | Rare | |
| Persistent Cough | Common | Less Common | |
| Tingling/Numbness | Rare | Common | |
| Fear of Dying | Possible | Hallmark Symptom | |
| Dizziness/Lightheadedness | Yes | Yes | X |
As you can see, wheezing is the most reliable sign of an asthma attack, as it’s the sound of air struggling to pass through narrowed airways. On the other hand, tingling or numbness in your hands, feet, or face is a classic sign of hyperventilation during a panic attack.
Recognizing these key distinctions is your first step toward control. It can help you decide whether to reach for your rescue inhaler or to focus on calming techniques to ride out the panic.
What To Do During An Asthma-Anxiety Episode
When the familiar tightness grips your chest and your thoughts start to spiral, having a clear, actionable plan is your most powerful tool. The lines between an asthma attack and a panic attack can blur into an overwhelming mess, but a structured response can help you regain control over both your breathing and your mind.

Here’s the most critical rule: always treat the physical symptoms first. Never, ever assume it’s “just anxiety.” Your asthma action plan is your primary guide, and that rescue inhaler is your first line of defense against constricted airways.
Step 1: Follow Your Asthma Action Plan
Your doctor gave you that rescue medication for a reason. Use it exactly as directed the moment you feel symptoms like wheezing, a stubborn cough, or that unmistakable chest tightness. Dealing with the potential physical cause right away removes a huge variable and can stop a mild flare-up from turning into a severe one.
Waiting to see if things get better on their own is a dangerous gamble. Using your inhaler gives your airways immediate relief, which in turn can help quiet the rising panic that comes with the terrifying feeling of being breathless. For a deeper dive into the clinical side of things, our guide to acute asthma exacerbation treatment offers some valuable medical insights.
Once you’ve handled the physical side, you can pivot to managing the anxiety that’s pouring fuel on the fire. The goal is to shatter the feedback loop where panic makes your breathing worse, and troubled breathing makes your panic worse.
Step 2: Ground Yourself in This Moment
Anxiety yanks your focus inward, trapping you in a terrifying cycle of “what if” thoughts. Grounding techniques are designed to pull your attention back outward, reconnecting you with your immediate surroundings and breaking that mental spiral.
The 5-4-3-2-1 Sensory Method is a simple but incredibly powerful tool for this. It methodically walks you through your senses to anchor you in the reality of the present, pulling you away from the internal chaos.
Here’s how you do it:
- See: Name 5 different things you can see around you. Notice their color, their shape, maybe a crack in the wall.
- Feel: Touch 4 different things. Focus on the sensation—the coolness of a countertop, the soft fabric of your shirt.
- Hear: Identify 3 distinct sounds. It could be the hum of the refrigerator, traffic outside, or your own breathing starting to slow.
- Smell: Name 2 smells you can pick up. Maybe it’s the soap on your hands or the faint scent of coffee.
- Taste: Acknowledge 1 thing you can taste. Take a sip of water or just notice the taste already in your mouth.
This exercise literally forces your brain to shift from abstract fear to concrete sensory input, which can dial down the intensity of panic in a big way.
Step 3: Take Back Control of Your Breath
I know it sounds completely backward to focus on breathing when you feel like you can’t breathe, but specific techniques can calm your nervous system and actually improve your lung function. The shallow, rapid breathing that comes with panic is incredibly inefficient and can make asthma symptoms feel even worse.
Pursed-Lip Breathing is a technique clinicians recommend because it physically slows your breathing rate, makes the work of breathing easier, and helps release air that gets trapped in the lungs. It works by creating a little back pressure in your airways, which helps keep them open longer as you breathe out.
Here’s how to practice it:
- Breathe in slowly through your nose for a count of two.
- Pucker or purse your lips like you’re about to whistle.
- Breathe out slowly and gently through your pursed lips for a count of four.
This simple, intentional action can slow a racing heart and give you a sense of control right when you feel most helpless. By combining these steps—medication first, then grounding, then controlled breathing—you create a solid protocol to manage an asthma-anxiety episode and come out the other side.
Building a Proactive Long-Term Management Plan
Managing the chaos in the middle of an asthma-anxiety episode is a critical skill, but the real win is preventing these events from happening in the first place. This means shifting from a reactive mindset to a proactive, long-term strategy that addresses both your lungs and your mind. A truly resilient plan doesn’t just treat symptoms as they pop up; it builds a foundation of wellness that makes the whole cycle far less likely to ever get started.
This is about looking beyond your rescue inhaler and getting to the root of what makes your body so reactive. It requires a two-pronged attack: calming the chronic inflammation in your airways while simultaneously rewiring the anxious thought patterns that keep tripping your body’s alarm system.
Across the globe, asthma doesn’t just squeeze your lungs—it grips your mind, too. Data from 17 countries, covering over 85,000 adults, shows that people with asthma have 1.5 times higher odds of developing anxiety disorders. For many, this isn’t a secondary issue; it’s a core part of their daily reality with the condition, and it demands an integrated approach to care.
Fortifying Your Physical Defenses
Your first line of defense is to get the baseline inflammation in your airways under control. When your airways are less sensitive and swollen to begin with, they are far less likely to overreact to triggers—including the physiological stress of anxiety. This is precisely what controller medications are designed to do.
Unlike rescue inhalers that offer immediate relief, controllers work quietly in the background, day in and day out.
- Inhaled Corticosteroids (ICS): These are the cornerstone of modern asthma management. Taken daily, they reduce swelling and mucus production, making your airways far less “twitchy” and reactive.
- Long-Acting Beta-Agonists (LABAs): Often combined with an ICS in a single inhaler, these medications help keep the muscles around your airways relaxed for up to 12 hours.
- Biologics: For severe, difficult-to-control asthma, these advanced injectable medications are game-changers. They target specific inflammatory pathways in your immune system, offering a highly precise way to cool down the inflammation driving your symptoms.
A consistent controller medication routine is like building a firewall for your lungs. It doesn’t just put out the fire once it starts; it creates an environment where it’s much harder for a stray spark of anxiety to ignite a full-blown physical reaction.
Rewiring Your Mental Responses with CBT
Tackling the physical side is only half the battle. To truly break the cycle of asthma attack anxiety, you also have to dismantle the thought patterns that fuel it. This is where Cognitive Behavioral Therapy (CBT) becomes an invaluable tool.
CBT is a structured, evidence-based therapy that helps you identify, challenge, and reframe the negative thought loops that spiral into panic. It’s built on a simple principle: your thoughts, feelings, and physical reactions are all interconnected. Change the thought, and you can change how you feel and how your body responds.
A therapist trained in CBT can walk you through a clear process:
- Identify Automatic Thoughts: The first step is to simply notice the immediate, fearful thoughts that flash through your mind at the first sensation of chest tightness (e.g., “This is a major attack,” “I’m losing control,” “I can’t breathe”).
- Challenge Distorted Thinking: Next, you learn to examine the evidence. Are these catastrophic thoughts based on fact or just fear? What has actually happened during past episodes?
- Develop Coping Statements: Finally, you create and practice realistic, calming statements to deploy in moments of rising panic (e.g., “This feeling is familiar, and it will pass,” “I have my inhaler right here,” “I know exactly what to do”).
This process isn’t about ignoring your symptoms. It’s about learning to respond to them with logic instead of raw fear, which prevents the adrenaline surge that can physically make your asthma worse. Exploring a personalized approach to allergy and asthma treatment can help tailor these strategies to your specific triggers and needs.
Integrating Medical and Mental Health Care
For some, therapy alone isn’t enough to manage the intensity of the anxiety. Certain medications, like Selective Serotonin Reuptake Inhibitors (SSRIs), can be highly effective at lowering your baseline level of anxiety, making you far less susceptible to panic triggers.
However, it is absolutely essential that this is managed through a coordinated care plan. Your allergist or pulmonologist must be in communication with your mental health provider. Some medications can have interactions, and a holistic view of your health ensures that your treatment for anxiety complements—rather than complicates—your asthma management. This unified approach is the key to building a truly effective and sustainable plan for long-term health and peace of mind.
Knowing When You Need Specialist Care
Managing the day-to-day reality of asthma and anxiety is a delicate balancing act. While your primary care doctor is a crucial part of your team, there are times when your symptoms signal the need for a more focused level of expertise.
Recognizing these signs isn’t about failure; it’s a strategic move toward gaining greater control over your health. If you find yourself in a constant state of vigilance, it may be time to seek specialist care. This isn’t just about how often you have an attack, but how much the fear of an attack dictates your life.

Clear Signals to Escalate Your Care
So, how do you know when it’s time to move beyond your current plan? Certain patterns are clear red flags that your asthma—or the anxiety surrounding it—isn’t well-controlled. If any of the following feel familiar, it’s a strong sign to bring in a specialist.
It’s time for more support if you are:
- Using your rescue inhaler more than twice a week. This is a key benchmark. It means your baseline inflammation is too high and your current plan isn’t enough.
- Avoiding activities you once enjoyed. If the fear of triggering an episode keeps you from exercising, traveling, or seeing friends, your quality of life is being compromised. That’s not okay.
- Feeling like your care is fragmented. Juggling appointments between a GP for asthma and another provider for anxiety can be a nightmare. When they don’t communicate, crucial gaps can form in your treatment plan.
- Waking up at night with coughing or wheezing. Nocturnal asthma is a classic sign of poor control and absolutely requires specialized attention to get it sorted out.
The connection between asthma and anxiety is profound and bidirectional. Global data from 17 countries revealed that individuals with asthma are 1.5 to 1.6 times more likely to suffer from anxiety or depressive disorders, with one in three experiencing anxiety in their lifetime. You can explore the full research on the asthma-anxiety link to understand the data.
Understanding the Specialists Who Can Help
Navigating specialist care can feel intimidating, but each professional plays a distinct and vital role in managing complex cases of asthma attack anxiety. Knowing who does what helps you get the right help, right away.
Pulmonologist: This is your lung specialist. They are the experts in diagnosing and treating complex respiratory conditions, including severe or difficult-to-control asthma. A pulmonologist can perform advanced lung function tests and prescribe sophisticated treatments like biologics that your primary doctor might not.
Allergist/Immunologist: Since allergies are a major trigger for over 50% of adults with asthma, this specialist is absolutely key. They perform detailed testing to identify your specific environmental triggers—like pollen, dust mites, or pet dander—and can offer treatments like allergy shots (immunotherapy) to reduce your body’s reaction over time. Our network provides access to top experts in allergy and immunology.
Psychiatrist or Psychologist: For the anxiety component, a mental health professional is indispensable. A psychologist can provide therapies like CBT to help you rewire anxious thought patterns and regain control. A psychiatrist can do that as well, and if necessary, prescribe and manage anti-anxiety medications safely alongside your asthma treatments.
Seeking out one of these specialists is an empowered step. It means you are proactively assembling an expert team dedicated to crafting a precise, effective plan that addresses both your physical and mental well-being, paving the way for a calmer, healthier future.
Your Questions About Asthma and Anxiety Answered
When you’re dealing with both asthma and anxiety, a lot of questions come up. Getting clear, practical answers is the first step toward feeling in control and managing both conditions well. Let’s cut through the noise and tackle some of the most common questions people have about the link between asthma attacks and anxiety.
We’ll separate fact from fiction so you can focus on what really works for your health.
Can Breathing Exercises Alone Stop an Asthma Attack?
This is a critical point that causes a lot of confusion. While breathing exercises are incredibly powerful tools for managing anxiety, they have a very specific role. Techniques like pursed-lip or diaphragmatic breathing are fantastic for calming the shallow, rapid breathing that anxiety triggers. They can settle your nervous system down and keep panic from spiraling.
However, they absolutely cannot reverse the physical airway constriction of a true asthma attack.
Think of it this way: breathing exercises are a fire extinguisher for your panic, but your rescue inhaler is the fire hose for your lungs. During an actual asthma flare-up, your airways are physically narrowing from inflammation and muscle spasms. Only your prescribed rescue medication can open them back up. Always, always use your inhaler first, just as your action plan directs.
What Lifestyle Changes Help Both Asthma and Anxiety?
The great news is that many lifestyle changes pull double duty, benefiting both your respiratory and mental health. These strategies work by dialing down systemic inflammation and soothing your nervous system, creating a more resilient foundation for your body and mind.
Here are a few powerful adjustments to consider:
- Adopt an Anti-Inflammatory Diet: Foods rich in omega-3s (like salmon), antioxidants (like berries), and magnesium (like leafy greens) can lower the body’s overall inflammatory burden. This is a win for both your airways and your anxiety levels.
- Prioritize Consistent Sleep: Skimping on sleep causes a spike in cortisol, the stress hormone that worsens both anxiety and airway inflammation. A consistent sleep schedule is one of the best things you can do to stabilize your mood and strengthen your immune system.
- Embrace Approved Low-Impact Exercise: Activities like walking, yoga, or swimming (in a well-ventilated pool) can strengthen your lungs while releasing stress-busting endorphins. Just be sure to warm up properly and get your doctor’s green light first.
How Can I Explain My Asthma Anxiety to My Doctor?
Getting the integrated care you need starts with communicating your experience effectively. Many doctors are trained to focus on physical symptoms, so you might need to connect the dots for them between your mental state and your breathing. Instead of just saying “I feel anxious,” frame it in terms of its specific impact on your asthma.
Try using these phrases to get the conversation started:
- “I’ve noticed that when I feel stressed or panicky, my asthma symptoms get worse. Can we talk about how to manage that connection?”
- “The fear of having an asthma attack is causing me a lot of anxiety, and I’m worried the anxiety itself might be triggering some of my symptoms.”
- “I seem to be using my rescue inhaler more often, and I think it’s sometimes because of panic, not a true asthma flare. I need help telling the difference and creating a plan that addresses both.”
This kind of language shifts the conversation from a vague feeling to a concrete medical problem. It helps your doctor see the full picture, paving the way for a treatment plan that supports both your lungs and your mind.
Finding the right specialist who understands the complex interplay between physical and mental health is paramount. The Haute MD network is a premier resource that connects discerning patients with the nation’s top, board-certified physicians in fields like allergy, immunology, and executive health. Explore our curated directory to find a vetted expert who can provide the integrated, white-glove care you deserve.
Find your specialist at Haute MD.