Getting news that your stress test results were “abnormal” can feel like a punch to the gut. But it’s critical to understand what this really means. It’s not a final diagnosis, but rather your heart’s way of sending up a flare—a signal that your cardiologist needs to investigate further.
Decoding an Abnormal Stress Test Result
An abnormal stress test is a powerful diagnostic clue, not a definitive sentence of heart disease. It simply suggests that when your heart is working hard, it might not be getting all the oxygen-rich blood it needs. This condition is known as ischemia.
Think of this result as the first step in a much larger diagnostic journey. It’s about putting together a complete picture of your cardiovascular health, and this is just the first, crucial piece of the puzzle.
Common Indicators of an Abnormal Result
Cardiologists are trained detectives, looking for specific signals that point to potential issues with blood flow to the heart muscle. These clues can show up in different ways, depending on which type of stress test you had.
The most common red flags include:
- ECG Changes: Specific patterns on the electrocardiogram (ECG), like ST-segment depression, can suggest that parts of your heart muscle are struggling under the strain of exercise.
- Imaging Deficiencies: On a nuclear or echo stress test, the images might reveal areas of the heart wall that aren’t contracting properly or show reduced blood flow during exertion.
- Concerning Symptoms: If you experience significant chest pain (angina), become severely short of breath, feel dizzy, or have a sudden drop in blood pressure during the test, these are all important warning signs.
- Poor Exercise Capacity: Sometimes, the finding is as simple as not being able to reach the target heart rate or exercise duration for your age and fitness level. This can also be a significant clue.
An abnormal stress test is fundamentally a risk assessment tool. It helps stratify patients into higher or lower-risk categories, guiding the urgency and type of follow-up care needed to prevent future cardiac events.
To get a sense of what specific findings mean, this table breaks down some of the technical terms you might see on your report.
Decoding Common Abnormal Stress Test Findings
| Abnormal Finding | What It Looks Like | Potential Implication |
|---|---|---|
| ST-Segment Depression | A downward dip in a specific part of your ECG waveform. | Can indicate ischemia (reduced blood flow) to the heart muscle during exercise. The location and depth of the dip provide more clues. |
| Reversible Perfusion Defect | On a nuclear scan, an area of the heart shows less blood flow during stress but normal flow at rest. | This is a classic sign of a significant blockage in a coronary artery that limits blood flow only when the heart is working hard. |
| Wall Motion Abnormality | On an echocardiogram, a section of the heart muscle doesn’t contract as forcefully during stress as it does at rest. | This also points to ischemia, suggesting a blockage is preventing that section of the heart from getting enough oxygen to function properly. |
| Exercise-Induced Hypotension | Your blood pressure fails to rise or, even more concerning, drops during exercise. | This can be a sign of severe coronary artery disease or other serious cardiac conditions, as the heart can’t pump effectively under stress. |
This isn’t just academic. These results have real-world clinical significance. One study of patients who had imaging stress tests found that abnormal results were detected in approximately 37% of individuals. Of that group, 19% later needed hospital readmission and 3% had a heart attack, underscoring how these findings help predict—and hopefully prevent—future cardiac events. You can explore more on how this study’s impact informs clinical decisions.
Ultimately, these abnormal findings are your cardiologist’s starting point. They are gathering the evidence needed to map out the next logical step, which could be anything from medication and lifestyle changes to more definitive diagnostic tests. Your result is the beginning of a conversation, not the final word.
Understanding Different Types of Cardiac Stress Tests

To make sense of an abnormal result, you first have to understand the specific tool your cardiologist used. Not all stress tests are created equal; each serves a distinct purpose and offers a different level of detail. Think of them as a specialized toolkit—your doctor selects the right instrument based on your unique symptoms and risk profile.
The one most people are familiar with is the standard Exercise Stress Test, often just called a treadmill test. You walk on a treadmill while connected to an electrocardiogram (ECG) machine, and the goal is to see how your heart’s electrical activity responds to physical exertion. It’s a great foundational test for a first look at your cardiac fitness and for spotting major electrical changes under stress.
Adding Imaging for a Clearer Picture
But when a simple ECG isn’t enough, or if your cardiologist needs to see how your heart muscle is physically performing, they’ll bring in imaging. These more advanced tests give a far more detailed view, dramatically improving the accuracy of the diagnosis.
Two of the most common imaging-based stress tests are:
- Stress Echocardiogram: This test combines the treadmill with an ultrasound of your heart. An initial “echo” is done while you’re at rest, creating a video of your heart’s chambers and walls. Immediately after you finish exercising, a second echo is performed. By comparing the “before” and “after” videos, your doctor can spot if any parts of your heart muscle aren’t contracting as forcefully when stressed—a classic sign of a blockage.
- Nuclear Stress Test (Myocardial Perfusion Imaging): This is a more sophisticated method that uses a safe, radioactive tracer injected into your bloodstream to literally “light up” blood flow to the heart. A special camera captures images of your heart at rest and again after stress. Any areas that get less tracer during exercise show up as “cold spots,” pointing directly to where a blockage might be restricting blood flow.
These tests are at the forefront of a rapidly growing field. With cardiovascular disease remaining a top health concern worldwide, the demand for precise, early detection is soaring. The ECG stress test market alone was valued at around USD 2.7 billion and is projected to keep expanding, driven by an aging population and lifestyle factors that elevate heart disease risk.
What If You Can’t Exercise?
For people who can’t use a treadmill due to arthritis, an injury, or another medical condition, there’s a solution: the pharmacological stress test. Instead of physical exertion, a medication is given through an IV to mimic the effects of exercise on the heart.
This medication either makes your heart beat faster or dilates your coronary arteries, just like a brisk walk would. This “chemical stress” allows doctors to perform either an echocardiogram or a nuclear scan to see how your heart responds, making it a critical alternative for many patients. Understanding these electrical and functional responses is at the core of cardiology; if you’re curious about the specialty focused on the heart’s electrical system, you can read this quick guide on what electrophysiology cardiology is.
The type of stress test chosen is a strategic decision. A simple ECG test may suffice for a lower-risk individual, while a high-risk patient with ambiguous symptoms will almost always benefit from the superior clarity provided by imaging.
Ultimately, the choice of test directly impacts how your abnormal stress test results are interpreted. An abnormality on a nuclear scan provides entirely different information than an ECG change alone. Knowing which test you had gives you the context needed to understand what the findings mean for your heart—and what comes next.
True Positives vs. False Alarms: What’s Really Going On?
Getting the news that your stress test was “abnormal” is unsettling. The first question that flashes through your mind is almost always the same: is this a real problem, or could it be a false alarm? Making sense of this is the first step toward getting the right answers and managing the very real anxiety that comes with an uncertain result.
A true positive is exactly what it sounds like. It’s the test working as intended, correctly flagging significant coronary artery disease. In this scenario, a blockage is genuinely restricting blood flow to the heart muscle (a condition called ischemia) when you exert yourself. This is the signal we’re looking for—a clear indication that we need to dig deeper and likely intervene.
But no medical test is perfect. A false positive is the opposite—it’s a faulty alarm. The test suggests a problem that, after further investigation, turns out not to exist. Think of it like a sensitive car alarm that goes off in a thunderstorm. While it definitely gets your attention, the car is perfectly fine. A false positive means more advanced tests will likely show your coronary arteries are clear.
Why Do False Positives Happen?
It’s natural to feel confused or even frustrated by a false positive, but it’s a well-known limitation of stress testing, especially the standard exercise ECG. A number of factors can throw off the results, creating electrical signals or symptoms that look deceptively like true ischemia.
Knowing what can cause these misleading results helps put things in perspective while you’re waiting for definitive answers.
Here are some of the most common culprits behind a false positive:
- Pre-Existing ECG Patterns: Some people have a baseline heart rhythm, like a “left bundle branch block,” that can distort the ECG readout during exercise. It makes the test incredibly difficult to interpret and often mimics the signs of a blockage.
- Female Physiology: Women, particularly before menopause, have a higher rate of false-positive ECG stress tests. The exact reasons aren’t perfectly clear, but it’s thought to be related to hormonal influences and anatomical differences in the chest.
- Certain Medications: Common drugs for blood pressure or other heart conditions can change how your heart responds to exercise, directly affecting the ECG readings and sometimes creating a misleading picture.
- Being Out of Shape: If you aren’t used to intense exercise, your body’s reaction—a racing heart, shortness of breath—can sometimes be confused with a cardiac problem when it’s really just a sign of your current fitness level.
A false positive doesn’t mean the test was a waste of time. It’s a valuable piece of the puzzle. It forces your cardiologist to investigate more thoroughly, ensuring no real issue is missed while methodically ruling out a benign explanation.
Understanding these possibilities is crucial. The next step is seeing how a cardiologist puts all the clues together to separate the real signals from the noise.
Differentiating the Signals
An experienced cardiologist never makes a judgment based on a single piece of data. They function more like a detective, carefully weighing all the evidence to decide if an abnormal finding points to a real blockage or just a harmless imitation. They’ll look at the ECG changes, of course, but they’ll also consider how you felt during the test, how long you could exercise, and how your blood pressure and heart rate responded.
It’s about building a complete clinical picture. Here’s a look at how cardiologists sort through the data to distinguish between a true problem and a false alarm.
True Positive vs. False Positive Stress Test Results
This table breaks down the key differences a cardiologist looks for when evaluating abnormal stress test results.
| Factor | True Positive Indicator | Common Cause of a False Positive |
|---|---|---|
| ECG Changes | Significant, widespread ST-segment depression that shows up early in the test and lingers long into recovery. | Minor or isolated ECG changes that appear only at peak heart rate and disappear almost immediately. |
| Symptoms | You develop classic angina—chest pressure, tightness, or pain—that gets worse with exertion and better with rest. | You experience atypical chest pain, general fatigue, or shortness of breath without specific corresponding ECG changes. |
| Imaging Results | A stress echo shows a section of the heart muscle isn’t moving correctly (a wall motion abnormality), or a nuclear scan reveals a clear perfusion defect (a “cold spot”). | The imaging is completely normal, showing healthy blood flow and muscle function, even if the ECG looked abnormal. |
| Overall Clinical Picture | The patient has multiple risk factors for heart disease (e.g., high cholesterol, diabetes, a strong family history). | The patient is low-risk, healthy, and has no other concerning signs or symptoms of heart disease. |
When it’s all said and done, an abnormal stress test is the start of a conversation, not the final word. If the evidence is ambiguous or strongly suggests a false positive, your doctor won’t leave it to chance. They’ll recommend a more definitive test to get a clear, undeniable answer, ensuring your health decisions are based on certainty, not just suspicion.
Navigating Your Next Steps After an Abnormal Result
Getting an abnormal stress test result can feel like standing at a crossroads without a map. But it’s critical to see this not as a final diagnosis, but as the very first clue in a structured investigation. Your cardiologist now has a reason to dig deeper, and the next steps are all about turning that initial hint into a definitive answer.
This is a process of moving from suspicion to certainty. An abnormal result raises a question about blood flow to your heart; the follow-up tests are designed to provide a precise, high-definition answer. Your medical team will lay out a logical path, with each test building on what the last one revealed.
This visual decision tree shows the two main paths an abnormal result can lead to, helping clarify the diagnostic journey ahead.
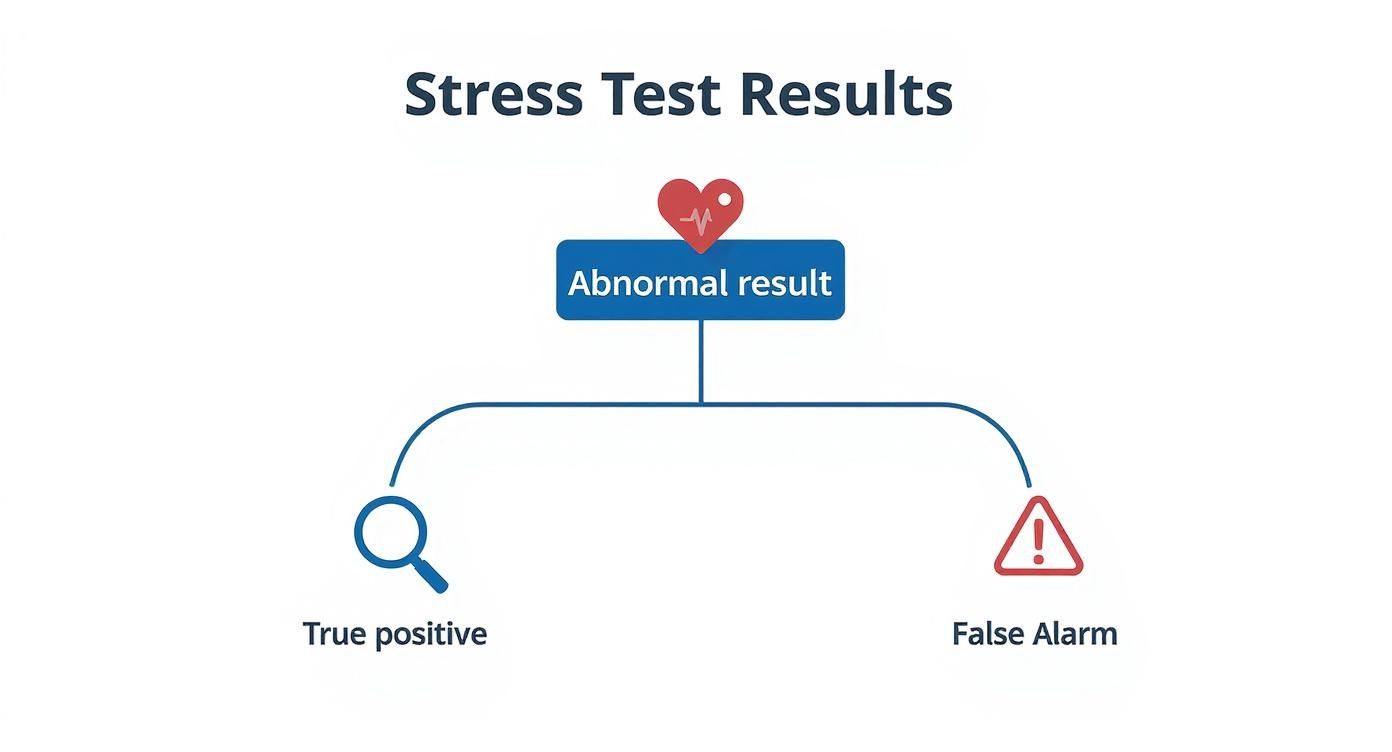
As the infographic illustrates, the goal is to figure out if this is a true signal of a problem or just a harmless false alarm. That answer dictates every diagnostic and treatment decision that follows.
The Next Level of Investigation
If your first test was a standard exercise ECG, the most common next step is a more advanced, non-invasive imaging test. Your doctor might recommend a stress echocardiogram or a nuclear stress test if you haven’t had one already. These tests don’t just track electrical signals; they provide actual pictures of your heart muscle and blood flow under stress.
However, if your initial results were highly abnormal or you’re experiencing significant symptoms, your cardiologist may decide to skip the intermediate steps and go straight to more definitive imaging.
A Coronary Computed Tomography Angiography (CCTA) is a powerful, non-invasive option here. This advanced CT scan uses dye and X-rays to create stunningly detailed 3D images of your heart’s arteries. It’s exceptionally good at ruling out coronary artery disease—if a CCTA comes back clean, you can be extremely confident your arteries are not the source of the problem.
The Gold Standard Diagnostic Test
When the evidence strongly points toward a significant blockage, cardiologists turn to the “gold standard” for diagnosis: cardiac catheterization, more commonly known as a coronary angiogram. This is an invasive procedure, but its precision is unmatched.
During an angiogram, a cardiologist skillfully guides a very thin, flexible tube (a catheter) from an artery in your wrist or groin all the way to your heart. A special dye is then injected directly into the coronary arteries, and real-time X-ray videos reveal their exact anatomy.
A coronary angiogram doesn’t just show if there’s a blockage; it shows exactly where it is, how severe it is, and what the plaque looks like. This level of detail is absolutely essential for planning any kind of intervention.
The unique power of an angiogram is its ability to pivot instantly from diagnosis to treatment. If a critical blockage is found, the cardiologist can often perform an angioplasty and place a stent during the very same procedure, immediately restoring blood flow to the heart muscle.
From Diagnosis to a Clear Treatment Plan
Understanding these follow-up procedures is key. Each step is a methodical move designed to give you and your doctor the clarity needed for an effective treatment plan. The information gathered will determine whether your path forward involves lifestyle changes, medication, a minimally invasive procedure like a stent, or a more significant intervention.
In cases where a major procedure like bypass surgery is on the table, choosing the right facility is paramount. Finding the best hospital for heart surgery options means looking closely at surgical expertise, advanced technology, and patient outcomes. Your abnormal stress test result is the first step on a path that leads to this level of precise, personalized care, ensuring you receive the most appropriate and effective treatment for your specific condition.
How Doctors Interpret Your Overall Heart Risk
Getting an abnormal stress test result can be alarming, but for your cardiologist, this finding is just one piece of a much larger, more intricate puzzle. A skilled physician doesn’t just react to a single data point. Instead, they perform a comprehensive risk assessment, blending the test data with your unique health profile to see the complete picture.
This holistic judgment is what separates exceptional medical care from a simple, automated response. The abnormal ECG change or imaging defect is the starting point, not the conclusion. Your doctor combines this with other crucial metrics gathered during the test to understand the full context of your heart’s performance under pressure.
The Metrics That Matter Beyond the Result
An expert cardiologist analyzes the entire dynamic of the test, looking for patterns and clues that reveal your true cardiovascular fitness. They are weighing several key factors at once to gauge your overall risk.
These critical performance indicators include:
- Your Exercise Capacity: How long and how hard could you push yourself? Your functional aerobic capacity, measured in metabolic equivalents (METs), is a powerful predictor of your health. A strong performance suggests a protective level of fitness, while a very low capacity can be a major red flag.
- Heart Rate Response and Recovery: How quickly did your heart rate climb? More importantly, how fast did it drop after you stopped exercising? A slow heart rate recovery—the speed at which your pulse returns toward its resting state—is an independent marker of increased cardiac risk.
- Blood Pressure Dynamics: A healthy response involves a steady rise in systolic blood pressure during exertion. An abnormal response, like a drop in blood pressure, can signal severe underlying issues and requires immediate, careful evaluation.
A cardiologist’s interpretation is an art informed by science. They integrate the “what” (the abnormal finding) with the “how” (your body’s performance) to create a nuanced risk profile that guides the next steps with precision.
Weaving Your Personal Health Story into the Data
The final step in this assessment is placing the test results into the context of you. Your personal health history provides the framework for interpreting what the data truly means for your future. A specific ECG finding might be highly concerning in one person but less urgent in another, depending entirely on their background.
Your doctor will meticulously weigh factors such as:
- Your age and gender
- Your family history of heart disease
- Existing conditions like diabetes, high blood pressure, or high cholesterol
- Your lifestyle habits, including diet, exercise, and smoking history
This comprehensive approach is why focusing on a specific diagnosis is a priority. For instance, a focus on preventive cardiology can provide a roadmap for mitigating future risks identified during this assessment.
Research from a landmark Mayo Clinic study of over 13,000 patients reinforces this broader view. The findings showed that stress test indicators like low aerobic capacity and slow heart rate recovery were powerful predictors of not just cardiac events but also overall mortality from other causes, including cancer. This highlights how a stress test provides a window into your body’s overall resilience. Discover more about how these exercise metrics predict long-term health.
Ultimately, your cardiologist’s final recommendation is a synthesis of all this information. It’s a thoughtful, evidence-based judgment that balances the objective test data with your personal story, ensuring the plan forward is perfectly calibrated to your specific needs and overall health.
Preparing for Your Follow-Up Appointment
Getting a call about an abnormal stress test can be jarring. It’s natural to feel a surge of anxiety, but walking into your cardiologist’s office armed with the right mindset can turn that fear into empowerment. This is your chance to become a proactive partner in your own healthcare. The key is knowing what to ask to get the clarity you need.
Your goal is to leave that appointment with a concrete understanding of what’s going on and a clear plan. Vague assurances aren’t enough—you need specifics to make informed decisions about your health.
Arming Yourself with the Right Questions
Think of this appointment as an information-gathering mission. Your cardiologist has the raw data, but it’s up to you to steer the conversation toward your specific concerns. If you walk in with a list of questions, you won’t leave wondering what you forgot to ask.
First, you need to understand the result itself. Go beyond the simple “abnormal” label.
- What specific part of my test was abnormal? Was it an ECG change? A problem with wall motion on the echo? Or was it a perfusion defect on the nuclear scan?
- How significant is this finding? Ask your doctor to put it on a scale from mild to severe. Where does your result fall?
- Could this be a false positive? What factors in my personal health profile might suggest this is a false alarm versus a true indicator of a problem?
This foundational knowledge helps you grasp the real context of your abnormal stress test results.
A well-informed patient is a doctor’s best partner. Your questions create a dialogue that leads to shared decision-making, ensuring the treatment plan aligns with your health goals and personal values.
Understanding the Path Forward
Once you understand the “what,” it’s time to focus on the “why” and “how” of what comes next. The follow-up plan is just as critical as the initial result, and you deserve to understand every single part of it.
Your questions should now pivot to the proposed diagnostic journey.
- What is the next test you are recommending, and why this one specifically? You need to understand the purpose of the next procedure, whether it’s a CCTA or a more invasive coronary angiogram.
- What are the risks and benefits of this test? Every medical procedure has a trade-off. Your doctor should be able to explain them clearly.
- Are there any non-invasive alternatives we should consider first? This is a crucial question to ensure you’re exploring all available and appropriate options.
- Based on these results, what immediate lifestyle changes should I make? Get actionable advice on diet, exercise, and stress management that you can start implementing today.
- What is the timeline for these next steps? Knowing the schedule helps manage expectations and reduces the anxiety that comes from uncertainty.
Walking out of your appointment with direct answers to these questions gives you a concrete plan. It replaces the fear of the unknown with a clear roadmap for your heart health, empowering you to take control of what comes next.
Of course. Here is the rewritten section, crafted to sound like an experienced human expert, following the specific style and voice of the provided examples.
Your Questions About Stress Test Results, Answered
Getting your stress test results is just the first step. Now, you’ve probably got a dozen new questions running through your mind. That’s completely normal. Let’s walk through some of the most common questions my patients ask after their evaluation.
Can I Have a Heart Attack Even with a Normal Stress Test?
Unfortunately, yes. It’s a tough reality to grasp, but a “normal” result isn’t an ironclad guarantee. Think of a standard stress test as a traffic report for your coronary arteries—it’s excellent at spotting a major traffic jam, the kind of blockage (70% or more) that restricts blood flow when you’re exerting yourself.
What it often misses, however, are the smaller, less severe pile-ups—the non-obstructive plaques. These smaller plaques can be unstable and rupture unexpectedly, causing a sudden clot that leads to a heart attack. So while a normal test is certainly reassuring and lowers your immediate risk, it doesn’t give you a free pass to ignore your heart health.
How Accurate Is a Cardiac Stress Test, Really?
The accuracy depends entirely on the type of test you get. A basic exercise ECG—just you on a treadmill hooked up to an EKG—is the entry-level option. Its sensitivity (the power to find disease if it’s there) is around 68%, and its specificity (the ability to correctly give an all-clear) is about 77%.
Frankly, that leaves a lot of room for error—both false alarms and missed warnings. This is precisely why we add imaging into the mix whenever possible.
When you upgrade to a stress echocardiogram (using ultrasound) or a nuclear stress test (using a radiotracer), the game changes. The accuracy for both sensitivity and specificity jumps to over 85%. This gives your cardiologist a much sharper, more reliable picture of how your heart is truly functioning under pressure.
Your doctor weighs these factors to choose the right test for you, balancing the need for precision against your individual health profile.
My Test Was Abnormal. What Lifestyle Changes Should I Make Right Now?
An abnormal result is a powerful wake-up call, regardless of whether it’s a true positive or just a false alarm. It’s your body’s way of telling you to start prioritizing your heart, starting today. Your cardiologist will give you a personalized game plan, but the foundational moves are consistent because they work.
Here’s where you can take back control immediately:
- Overhaul Your Diet: Start thinking like someone who lives on the Mediterranean coast. Your plate should be full of fruits, vegetables, whole grains, and healthy fats from olive oil and fish.
- Get Moving (Safely): Once your doctor gives you the green light, commit to regular, moderate exercise. The goal is to make your heart a stronger, more efficient muscle.
- Know and Manage Your Numbers: This is non-negotiable. You must work with your doctor to get your blood pressure, cholesterol, and blood sugar under control.
- Cut Out the Toxins: If you smoke, stop. It’s one of the single most impactful things you can do. At the same time, find healthy ways to manage your stress, which is a major accelerator of heart disease.
Taking these steps puts you back in the driver’s seat of your own health journey.
Navigating the complexities of cardiac care requires access to the best specialists. At Haute MD, we connect you with a curated network of the nation’s top cardiologists and executive health physicians, ensuring you receive premier, personalized care. Find a leading expert to guide your next steps by visiting Haute MD.

