An abnormal stress test result is your heart’s “check engine light.” It means the test flagged a potential issue with blood flow to your heart muscle when it was pushed, but it is not a diagnosis of a heart attack. Think of it as the critical first signal that tells your doctor, “we need to look closer here.”
This result is simply the start of a clear, well-defined diagnostic process.
What an Abnormal Stress Test Result Really Means
Getting a call about any “abnormal” result can be unsettling, especially when it’s about your heart. It’s crucial, however, to put this information in the right context. An abnormal stress test is the beginning of a conversation, not the final word. It’s a sensitive screening tool designed to cast a wide net and catch anyone who might have an underlying problem.
The whole point of a cardiac stress test is to see how your heart handles work. As you push yourself on a treadmill or bike, your heart demands more oxygen-rich blood. If the arteries supplying your heart have narrowed—a condition called coronary artery disease (CAD)—they might struggle to deliver enough blood to meet that increased demand.
Interpreting the Signal
This mismatch between what the heart needs and what the arteries can supply can trigger specific changes on your electrocardiogram (EKG), cause chest discomfort, or bring on other symptoms during the test. Those findings are what get flagged as an “abnormal” result.
At its core, the test is asking one simple question: when we put the heart under stress, is there any evidence of reduced blood flow (ischemia) to the muscle? An abnormal finding just suggests the answer might be yes.
An abnormal stress test is fundamentally a screening result. Its value isn’t in providing a definitive diagnosis but in identifying individuals who require a more detailed and specific evaluation. It efficiently sorts patients into groups needing a closer look.
From this point, the entire goal is to figure out the cause and the true significance of that signal. It’s a structured investigation that moves from a broad clue to a precise diagnosis.
To help frame your thinking, here’s a quick summary of what this result really means in the immediate term.
Key Takeaways From an Abnormal Stress Test Result
| Concept | What It Means for You |
|---|---|
| A Screening Tool | The test is designed to be sensitive, meaning it flags any potential concern. It’s not a definitive diagnosis of heart disease. |
| A Call for Context | Your symptoms, risk factors, and overall health profile are just as important as the test result itself in determining next steps. |
| A Starting Point | This isn’t the end of the road. It’s the beginning of a clear diagnostic pathway to get definitive answers. |
| A Path to Action | The result provides the information needed to take proactive, informed steps toward protecting your long-term heart health. |
This table helps put the result into perspective: it’s a piece of the puzzle, not the whole picture.
Moving from Indication to Diagnosis
Your physician now acts like a detective, using the abnormal stress test as a crucial clue. They will combine this finding with your complete clinical picture—your risk factors, symptoms, and overall health—to understand what’s really going on. This context is everything, because an abnormal test can have several explanations, and not all of them point to a serious problem.
Here are the key things to keep in your mind:
- It’s a Signal, Not a Verdict: The result simply flags a potential issue that needs a more precise, focused investigation.
- Context is Everything: Your personal health story provides the context needed to interpret the test correctly.
- A Clear Path Forward Exists: This result kicks off a well-established diagnostic plan to get you the right answers and the right care.
Understanding this framework can demystify the entire process and significantly reduce anxiety. An abnormal stress test result empowers you and your care team with the information needed to take proactive steps, ensuring you get the right follow-up at the right time.
Understanding Different Types of Cardiac Stress Tests
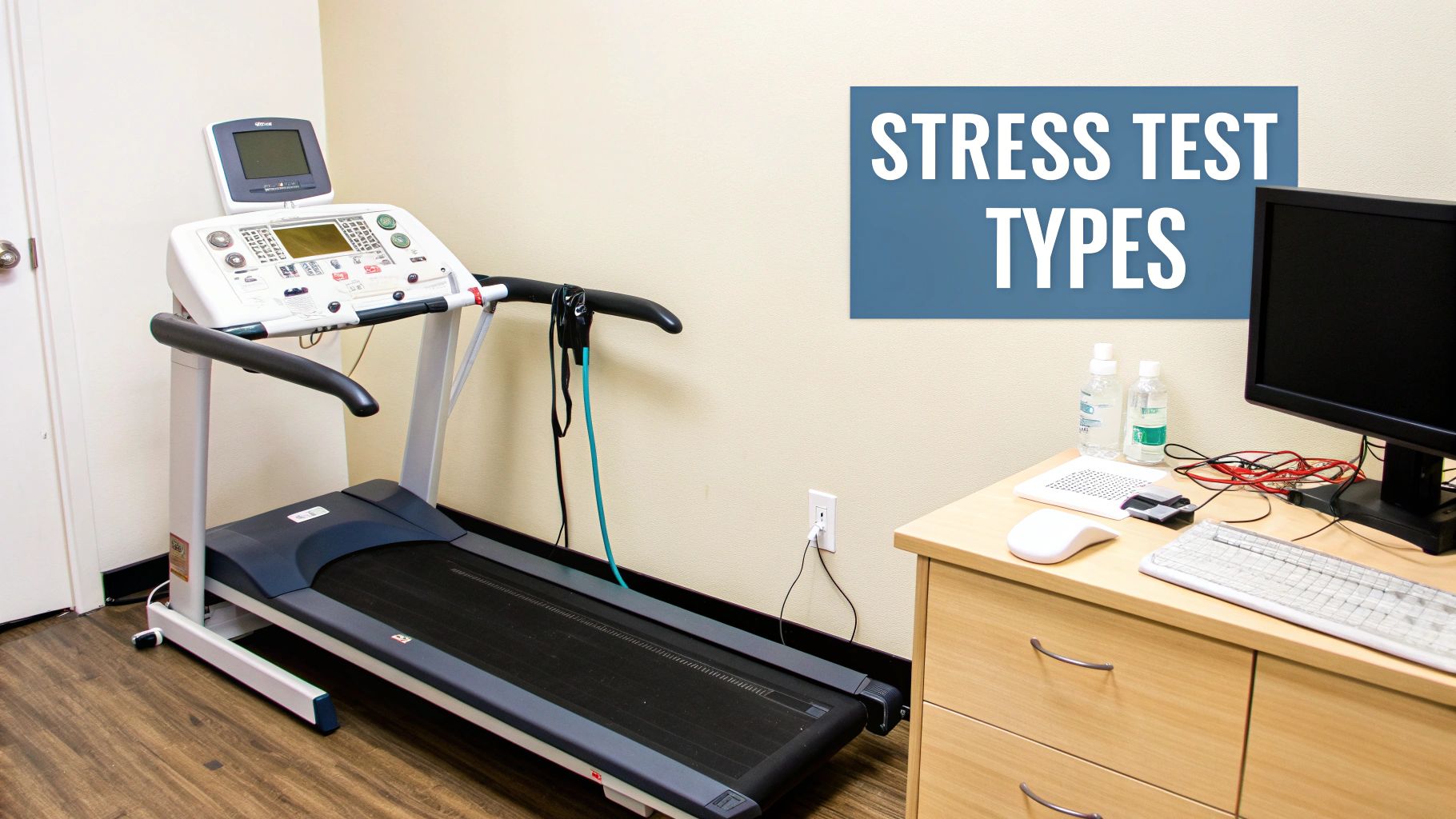
Not all stress tests are created equal. Decoding an “abnormal” result starts with understanding which test you actually had, because each one provides a different kind of information. Think of it like a mechanic diagnosing a car engine; listening to the engine provides one level of data, while plugging it into a computer diagnostic offers far more detail.
The most basic version is the standard exercise stress test, but cardiologists often layer in advanced imaging to get a much clearer picture of your heart’s function under strain. Each test has specific strengths, and the right one is chosen based on your health profile and symptoms. Let’s break down the common options.
The Standard Exercise Stress Test
This is the classic treadmill test. You’ll walk, and eventually run, on a treadmill while connected to an electrocardiogram (EKG) machine. The speed and incline ramp up in stages to make your heart work progressively harder.
Throughout the test, a technician is watching three key things: your EKG for electrical changes, your heart rate, and your blood pressure. An abnormal stress test here usually means the EKG shows specific changes—like ST-segment depression—that suggest a part of the heart muscle isn’t getting enough oxygen.
It’s an excellent screening tool, but it only shows the electrical “shadow” of a potential problem. It doesn’t give you a direct visual of blood flow or how the heart muscle itself is moving.
The Stress Echocardiogram
Building on the standard test, a stress echo adds a powerful imaging component. Before you start exercising and again immediately after you finish, a sonographer uses an ultrasound probe to capture images of your heart.
This allows your doctor to actually see how the walls of your heart muscle are contracting. When a coronary artery is significantly blocked, the segment of heart muscle it supplies often can’t pump as vigorously when it’s put under stress.
Here’s what your cardiologist is looking for:
- Resting Function: The first ultrasound establishes a baseline, showing how your heart muscle moves at rest.
- Post-Exercise Function: The second one, taken right after peak exercise, looks for any new abnormalities in wall motion that weren’t there before.
- Comparison: Your doctor then compares the “before” and “after” images side-by-side. If a new area of weakness appears, it strongly suggests ischemia caused by a blocked artery.
This test gives a direct look at the heart’s mechanical function, which makes it more specific and less prone to false positives than a standard EKG test alone.
The Nuclear Stress Test
A nuclear stress test, also known as myocardial perfusion imaging, offers the most detailed map of blood flow to the heart muscle. The test involves injecting a very small, safe amount of a radioactive tracer into your bloodstream. This tracer is taken up by your heart muscle, essentially “lighting up” the areas that are getting good blood flow.
A special gamma camera takes images of your heart at two key moments:
- At Rest: The first set of images shows the blood flow pattern when your heart isn’t working hard.
- Under Stress: The second set is taken after you exercise or are given medication to stress the heart.
By comparing these two sets of images, a cardiologist can precisely map blood flow. An “abnormal” result here is typically a “perfusion defect”—an area of the heart that looks bright and well-supplied at rest but appears dim or dark after stress. This is a classic sign that a blockage is preventing adequate blood flow when demand is high.
The Pharmacological Stress Test
What if you can’t exercise on a treadmill because of severe arthritis, an injury, or another medical condition? That’s where a pharmacological stress test comes in. It uses medication to simulate the effects of exercise on the heart.
Drugs like adenosine, dobutamine, or regadenoson are given through an IV. They work by either increasing your heart rate and the force of its contractions or by dilating your coronary arteries, which mimics the physiological state of intense physical exertion.
This chemical stress is then paired with either an echocardiogram or nuclear imaging to see how your heart responds. It’s a critical tool that allows doctors to evaluate patients who would otherwise be untestable with traditional exercise protocols.
Decoding Your Results: Is It Ischemia or a False Positive?
Getting an abnormal stress test result immediately raises a critical question: Is this a real problem, or is it just a false alarm? Your cardiologist’s job is to figure that out, and the investigation will head down one of two paths. Either the test has correctly identified true ischemia—a genuine reduction in blood flow to the heart—or it’s a false positive, where the test looks abnormal for reasons unrelated to a blockage.
Think of it like a highly sensitive smoke detector. Sometimes it goes off because there’s a real fire starting (ischemia). Other times, it’s just triggered by steam from the shower (a false positive). A cardiologist’s role is to determine which it is before calling the fire department.
The Case for True Ischemia
A “true positive” result is when the stress test has done its job perfectly and identified ischemia. This is the medical term for any time an organ isn’t getting enough blood, and in cardiology, it specifically means the heart muscle is starved for oxygen-rich blood when put under demand.
The most common culprit behind this is significant coronary artery disease (CAD). Over years, plaque can build up inside the heart’s arteries, narrowing the passageway for blood. When you’re resting, there might be enough room for blood to get through. But during exercise, your heart needs more fuel, and that narrowed artery simply can’t keep up with the demand.
This supply-and-demand mismatch is exactly what the stress test is designed to uncover. It shows up as tell-tale EKG changes or as defects on the imaging scans, signaling that a physical blockage is very likely the cause.
Navigating the World of False Positives
Just as often, an abnormal stress test is nothing more than a false positive. This can create a lot of unnecessary anxiety, but it’s crucial to understand that many things can make a stress test look abnormal without a dangerous blockage being present. This is precisely why a cardiologist’s interpretation—based on your complete health profile—is so essential.
A false positive result doesn’t mean the test was a waste of time. It simply means the initial signal was caused by something other than significant coronary artery blockages. The next step is to methodically figure out what that “something” is.
Your doctor will carefully consider a list of common culprits that can trip up the test’s sensors.
Common Causes of a False Positive Result
- Baseline EKG Abnormalities: Some people just have minor, harmless quirks in their resting EKG. When they start exercising, these pre-existing electrical patterns can become exaggerated and mimic the signs of ischemia, raising a false flag.
- Certain Medications: Drugs for high blood pressure or other conditions can alter the heart’s electrical behavior and how it responds to stress. Sometimes, this can create EKG changes that look suspicious but aren’t.
- Other Heart Conditions: Structural issues are a big one. Conditions like mitral valve prolapse or left ventricular hypertrophy (a thickening of the heart muscle) are well-known causes of false-positive results on an EKG-only stress test.
- Female Biology: Pre-menopausal women, in particular, have a higher rate of false-positive results on standard EKG stress tests. This is a key reason why cardiologists often recommend stress tests that include imaging (like an echo or nuclear scan) for women to get a more accurate picture.
- Technical Issues: Sometimes the problem is surprisingly simple. Poor electrode contact with the skin or even just the patient moving around too much can create electrical “noise” that gets misinterpreted by the EKG machine.
Why Stress Tests Are Not Perfect
While cardiac stress testing is a cornerstone of cardiology, it’s not infallible. It’s a powerful tool, but it’s important to understand its limitations. The test has a surprisingly modest sensitivity for spotting obstructive coronary artery disease.
This limitation means a huge number of patients with actual CAD—estimated at around 892,419 each year in the U.S.—might get a false-negative result (a normal test despite having the disease). You can read more about these statistical findings on stress test accuracy in the U.S. for a deeper dive. The data shows that of this group, only between 258,000 and 379,000 have abnormal tests suggesting ischemia, while over half get a clean bill of health despite having underlying disease.
This data drives home a critical point: a stress test result is a clue, not a conclusion. It’s a single data point in a much larger clinical picture. Your cardiologist’s real expertise lies in putting that result in context with your personal risk factors, your symptoms, and your medical history to arrive at an accurate diagnosis. This careful, methodical approach is what transforms a raw test result into a meaningful plan of action.
Why Your Doctor Looks Beyond the Test Result
An abnormal stress test result doesn’t exist in a vacuum. A skilled cardiologist never just glances at the report and makes a snap judgment. Instead, they see it as one critical piece of a much larger, more personal puzzle—your complete health story.
Think of your cardiologist as a detective building a case. Before they even order a stress test, they’ve already gathered a ton of evidence. This evidence forms the basis of what we call pretest probability—a professional assessment of your likelihood of having coronary artery disease before the test is even run.
Building Your Clinical Picture
This initial assessment is fundamental to getting things right. It’s built by carefully evaluating a host of personal risk factors, with each one adding another layer of detail to your unique profile.
Your physician will consider things like:
- Age and Gender: Heart disease risk naturally climbs with age, and the patterns often differ between men and women.
- Symptoms: Are you experiencing chest pain (angina), shortness of breath, or fatigue with exertion? The nature of these symptoms provides critical clues.
- Family History: A history of premature heart disease in your parents or siblings can significantly elevate your own risk.
- Personal Health Factors: This is a big one. It includes your cholesterol levels, blood pressure, smoking history, and whether you have conditions like diabetes.
An abnormal result in a 40-year-old marathon runner with perfect cholesterol and no symptoms means something vastly different than the exact same result in a 65-year-old smoker with diabetes and classic chest pain. The first scenario points strongly toward a false positive, while the second raises a serious suspicion of true ischemia.
The core of expert cardiology isn’t just reading test results; it’s interpreting them within the rich context of the individual patient. Your pretest probability acts as a filter through which the results are analyzed, guiding the next steps with precision.
Understanding Test Accuracy and Context
No medical test is perfect, and stress tests are no exception. Each type has its own statistical accuracy—its ability to correctly identify people with the disease (sensitivity) and correctly identify people without it (specificity). This is where your overall clinical picture becomes so important.
If your pretest probability is very low, an abnormal result is far more likely to be a false positive. On the other hand, if your risk profile is high, a “normal” result might still warrant a closer look to make sure nothing was missed. This nuanced approach helps avoid both the unnecessary anxiety from a false alarm and the false reassurance from a misleadingly normal test.
Other factors, like abnormal heart rhythms that pop up during the test, also require expert analysis. Understanding the electrical signaling of the heart is a specialty in itself, and you can learn more about what cardiac electrophysiology is in our detailed guide.
The Bigger Picture of Cardiac Events
Stress testing is a cornerstone of cardiology—over 8 million nuclear stress tests are performed annually in the U.S. alone. But that doesn’t mean it’s always used perfectly. Studies have shown that 32% to 48% of these tests are sometimes classified as ‘rarely appropriate,’ which highlights why a cardiologist must carefully select patients based on their pretest probability in the first place.
Still, the results matter. Research involving over half a million U.S. patients revealed that those with an abnormal stress test had a significantly higher risk of adverse events. Specifically, about 3% of patients with an abnormal result indicating coronary disease faced a major cardiovascular event. These numbers confirm that while context is king, an abnormal result is a serious signal that demands diligent follow-up. You can find more details in this comprehensive study on cardiac stress testing outcomes.
Ultimately, your result is not a final verdict. It’s a critical data point that, when combined with your doctor’s expertise and your personal health story, illuminates the path toward a definitive diagnosis and an effective plan to protect your health.
Navigating Your Next Steps After an Abnormal Result
So, you’ve received an abnormal stress test result. The first question that pops into your head is probably, “What happens now?” Take a deep breath. The most important thing to know is that this isn’t the end of the road; it’s the beginning of a focused investigation to protect your heart. There’s a clear, established roadmap to get you definitive answers.
Your first and most critical move is the follow-up consultation with a cardiologist. This is where a single test result gets put into the full context of you—your health history, your risk factors, and your lifestyle. It’s how a general signal becomes a specific, personalized plan. Finding the right specialist is everything. For those who demand premier care, exploring resources on ways to find top-rated physicians near you can be an invaluable first step.
During this conversation, your doctor will lay out the next diagnostic steps needed to get a direct, unfiltered look at your coronary arteries.
The decision tree below shows how your individual risk profile shapes the urgency and direction of what comes next.
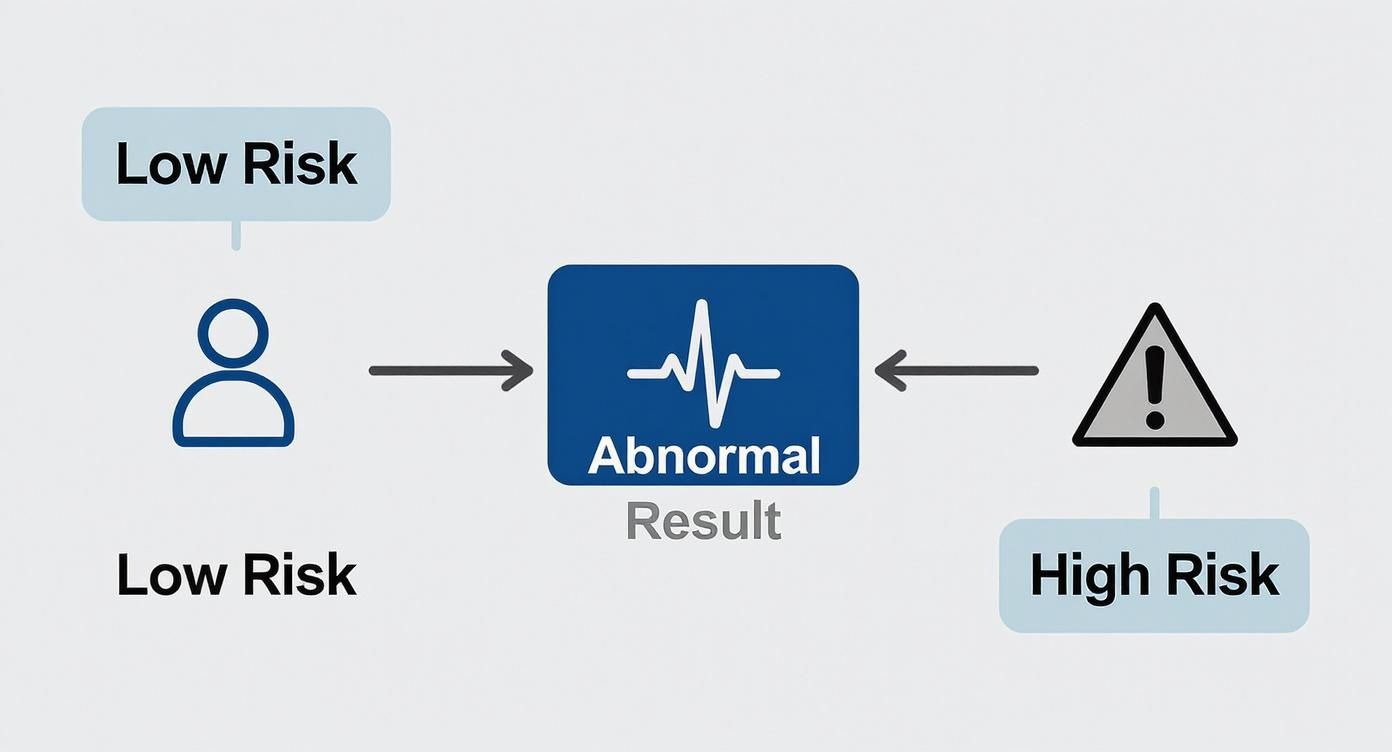
As the graphic shows, the very same abnormal result means something different for a patient with a low pre-existing risk versus someone with a high risk. This context is what guides the entire diagnostic journey.
Advanced Diagnostic Imaging Options
After an abnormal stress test, the goal is to shift from indirect evidence to direct visualization. Your cardiologist will likely recommend one of two highly effective imaging tests to get a clear answer.
1. Coronary CT Angiography (CCTA) Think of a CCTA as creating a high-resolution, 3D map of your heart’s plumbing. It’s a non-invasive test that uses advanced CT scanning to create incredibly detailed images of your heart and its arteries.
This test is fantastic at spotting both hardened (calcified) and soft plaque buildups on artery walls. Its greatest strength is its high negative predictive value—in simple terms, if the CCTA comes back clean, it’s extremely unlikely that you have significant coronary artery disease. It’s a powerful way to rule out a problem.
2. Cardiac Catheterization (Angiogram) This is the “gold standard” for diagnosing coronary artery disease. It’s a minimally invasive procedure where a cardiologist guides a very thin, flexible tube (a catheter) through a blood vessel up to your heart.
Once there, a special dye is injected, and X-ray images are taken. This creates a live-action video of blood flowing through your coronary arteries, letting your doctor see the exact location and severity of any blockages in real-time.
While an angiogram is more invasive than a CCTA, it provides the most precise diagnostic information available. Crucially, it also allows for immediate treatment. If a significant blockage is found, an angioplasty and stent can often be performed right then and there.
Potential Treatment Pathways
If further testing confirms you have significant coronary artery disease, your cardiologist will craft a treatment plan tailored specifically to you. The goal is simple: restore proper blood flow, get rid of symptoms, and slash your risk of future events like a heart attack.
The strategy depends entirely on how severe the blockages are and your overall health.
Lifestyle and Medication Management
For many people, especially those with mild to moderate disease, the first line of defense is a powerful one-two punch: lifestyle changes and medication. This is the bedrock of long-term heart health.
- Heart-Healthy Diet: Adopting an eating plan low in saturated fats, cholesterol, and sodium.
- Regular Exercise: Following a cardiac-safe exercise program that your doctor greenlights.
- Smoking Cessation: Quitting smoking is the single most effective lifestyle change you can make for your heart. Period.
- Medications: Your doctor might prescribe drugs to manage cholesterol (statins), lower blood pressure, or prevent blood clots (aspirin).
Interventional Procedures
When blockages are more severe and are causing symptoms or ischemia, your cardiologist may recommend an intervention to physically open up the narrowed artery.
The most common procedure is a percutaneous coronary intervention (PCI), better known as angioplasty and stenting. Performed during a cardiac catheterization, a tiny balloon is inflated inside the blocked artery to compress the plaque. Then, a small mesh tube called a stent is deployed to prop the artery open, locking in good blood flow.
In cases involving multiple, severe blockages, your doctor may bring up Coronary Artery Bypass Graft (CABG) surgery. This is an open-heart procedure where a surgeon uses a healthy blood vessel from another part of your body to create a detour around the blocked artery, effectively restoring blood flow to the heart muscle.
An abnormal stress test result isn’t a final verdict. It’s the key that unlocks a clear, methodical process of diagnosis and care, giving you the information you need to take full control of your heart health.
What Your Results Reveal About Your Overall Health
An abnormal stress test does more than just hint at a problem with your coronary arteries. Think of it as a detailed performance review for your entire cardiovascular system, giving you a snapshot of your body’s overall fitness and resilience that goes far beyond a simple “pass” or “fail” on blood flow.
Even if the result turns out to be a false positive for clogged arteries, the test is never a waste of time. It captures critical metrics about your physiological health that are powerful predictors of your long-term wellness. Two of the most important are your functional aerobic capacity and your heart rate recovery.
Beyond Blockages: A Fitness Assessment
Functional aerobic capacity is a fancy term for how efficiently your body uses oxygen when you’re pushing it. It’s a direct reflection of your cardiorespiratory fitness, and a low capacity can be a major red flag for your general health, not just for heart issues.
Likewise, heart rate recovery measures how quickly your pulse drops after you stop exercising. A fast drop is the sign of a healthy, well-conditioned heart. A sluggish recovery, on the other hand, can point to a less responsive nervous system and has been clearly linked to increased health risks down the road.
These metrics transform the stress test from a simple blockage detector into a powerful prognostic tool. The data gathered provides a baseline of your physiological age and fitness, offering insights that are fundamental to a proactive, long-term health strategy.
This isn’t just theory; it’s backed by serious research. A landmark Mayo Clinic study involving over 13,000 patients found that issues like low aerobic capacity and poor heart rate recovery were strong predictors of death from all causes, including non-cardiac ones like cancer. This really drives home the test’s value in assessing your complete health picture, as you can read in the Mayo Clinic’s findings on stress test abnormalities.
Ultimately, these results give you a wealth of actionable information. They arm you and your doctor with the data needed to build a robust wellness plan. This forward-thinking approach is at the core of preventive care, and you can learn more about what preventive cardiology is in our detailed article. By looking at the test through this wider lens, you can use every piece of data to optimize your health for years to come.
We Get These Questions All The Time
Hearing the words “abnormal stress test” can send a jolt of anxiety through anyone. It’s completely natural for your mind to jump to the worst-case scenario. But before you do, let’s walk through what these results really mean and what comes next.
Having clear, straightforward answers can make all the difference as you prepare for your follow-up with your cardiologist.
Does This Mean I’m Going to Have a Heart Attack?
Let’s be very clear: No, an abnormal stress test is not a crystal ball predicting an imminent heart attack. Think of it more like a sensitive smoke detector. It’s an early warning signal telling us we need to investigate further, allowing you and your physician to get ahead of any potential issues and protect your heart for the long haul.
A significant number of abnormal results are later found to be false positives or point to a condition that is highly manageable with the right strategy. The result itself is a reason for a closer look, not a reason to panic.
An abnormal stress test is a call to action, not a final diagnosis. It kicks off a crucial conversation with your cardiologist to figure out what’s really going on and build a clear, personalized plan forward.
Can I Still Exercise Safely?
This is a critical question, and the answer is deeply personal. Only your cardiologist can give you the green light after reviewing your specific results, your overall health profile, and your baseline fitness. The right advice depends entirely on what the test showed and your other risk factors.
Based on the findings, your doctor might advise you to:
- Continue with your current moderate exercise routine.
- Temporarily pull back on strenuous or high-intensity workouts.
- Pause all exercise until a final diagnosis is confirmed.
It is absolutely essential to follow your physician’s direct guidance before making any changes to your physical activity.
How Quickly Will I Get a Final Diagnosis?
The timeline for a definitive answer can vary, but it’s typically a streamlined process. You can usually expect a follow-up consultation with your cardiologist within a week or two to go over the stress test results and outline the next steps.
If more advanced imaging is needed—like a CCTA or a cardiac angiogram—it’s usually scheduled within the following few weeks. These tests are always prioritized based on medical urgency. Your cardiology team will give you a clear timeline so you know exactly what to expect.
When navigating the complexities of cardiac diagnostics, having access to the nation’s leading specialists is non-negotiable. Haute MD is an exclusive network that connects discerning patients with elite, board-certified physicians known for their precision and expertise. Find a top cardiologist to interpret your results and guide your next steps by visiting our curated network at Haute MD.

