The phrase “brain surgery” often brings a single, dramatic image to mind, but in reality, it’s not just one procedure. It’s a whole spectrum of highly specialized brain surgery types, each meticulously designed for a specific problem. These interventions run the gamut from traditional open craniotomies to sophisticated minimally invasive techniques, and even non-invasive radiosurgery that uses focused energy instead of a scalpel.
Understanding Your Neurosurgical Journey
Hearing that you might need brain surgery is, without a doubt, a heavy moment. It’s completely normal to feel overwhelmed. But it’s crucial to understand that modern medicine has made incredible leaps, transforming what was once thought impossible into routine, life-saving procedures. The path forward isn’t one you walk alone; it’s a clear, collaborative discussion with your medical team to find the right approach for you.
Think of this guide as a way to arm yourself with knowledge. Our goal is to demystify the world of neurosurgery, breaking down the main categories so you can feel confident and prepared when you talk with your doctors.
From Diagnosis to a Clear Plan
Everything starts with a precise diagnosis. From there, the conversation turns to the best way forward, which often involves surgery. This is especially true in the world of brain tumors, where progress has been nothing short of remarkable. In fact, brain cancer surgeries are the largest part of the neurosurgery market, a trend driven by the unfortunate rise in malignant brain tumors worldwide.
In the United States alone, this market is expected to hit over USD 1.3 billion by 2025. That growth is fueled by incredible technologies like advanced imaging and real-time intraoperative monitoring that give surgeons unprecedented precision. For non-cancerous tumors like meningiomas, the results speak for themselves—surgical success rates can be as high as 90-95%. You can learn more about these trends on cognitivemarketresearch.com.
Of course, a neurosurgeon’s work extends far beyond tumors. For a broader look at the conditions they handle, you might want to review what a neurosurgeon treats.
A diagnosis isn’t just a label; it’s the starting point for a strategic plan. Understanding the different types of brain surgery allows you to become an active partner in crafting that plan, ensuring it aligns with your health goals and personal priorities.
Ultimately, being informed is about more than just satisfying curiosity. It’s about recognizing why world-class care matters, where deep expertise and precision lead directly to better outcomes. This foundational knowledge is the perfect setup for a deeper dive into the specific procedures available.
The Three Main Approaches to Brain Surgery
Trying to get your head around the different brain surgery types can feel overwhelming, but it boils down to three main strategies. Neurosurgeons think about these approaches on a spectrum, defined by how direct the access to the brain needs to be. It ranges from a traditional open procedure to remarkable techniques that don’t even require an incision.
The right approach is always tailored to the specific problem—its size, its location, and its nature. The surgeon’s goal is to strike the perfect balance between treating the issue effectively and protecting the healthy, functioning brain tissue that surrounds it.
This diagram gives you a clear, high-level look at these fundamental categories.
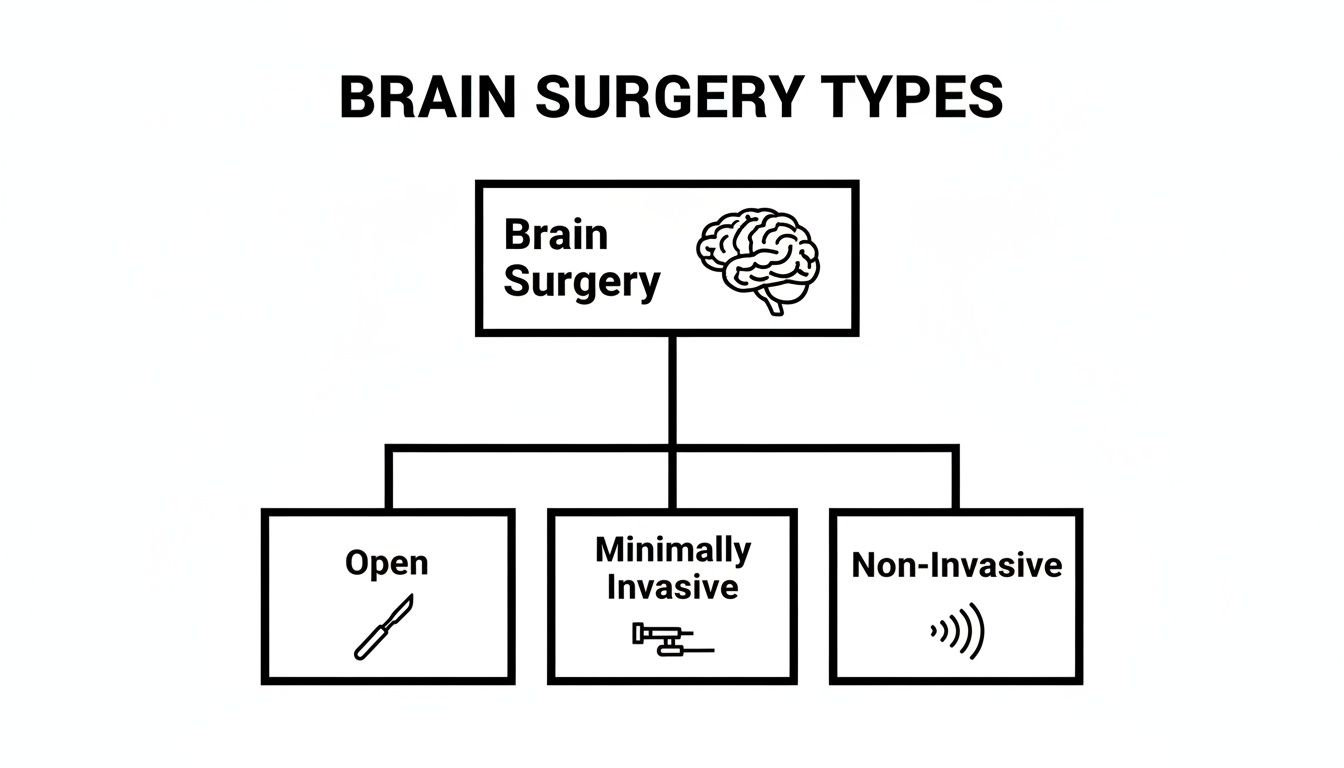
As you can see, the field has evolved from the most invasive methods toward incredibly precise, minimally disruptive techniques.
To give you a clearer picture, this table breaks down the key differences between the major surgical approaches at a glance.
At-a-Glance Comparison of Major Brain Surgery Approaches
| Surgical Approach | Invasiveness Level | Primary Use Cases | Typical Hospital Stay |
|---|---|---|---|
| Open Craniotomy | High | Large tumors, aneurysm clipping, trauma | 3-10 days |
| Minimally Invasive | Medium | Skull base tumors, biopsies, cysts, AVMs | 1-4 days |
| Non-Invasive | None | Small tumors, AVMs, functional disorders | 0-1 day |
This comparison highlights how the choice of surgery directly impacts everything from the conditions it can treat to the recovery experience you can expect. Now, let’s explore what each of these approaches really entails.
Open Brain Surgery: The Craniotomy
The most established and widely recognized approach is open brain surgery, usually performed as a craniotomy. Here, the surgeon makes an incision in the scalp and temporarily removes a small piece of the skull. This technique provides the widest, most direct view of the brain, giving the surgeon maximum room to work with delicate instruments.
Think of it like a master watchmaker needing to fix a complex, antique timepiece. To guarantee absolute precision, they first have to carefully remove the watch’s outer casing. A craniotomy follows the same logic, giving the neurosurgeon unobstructed access for the most intricate tasks.
Open surgery remains the gold standard for treating a host of conditions, including:
- Large or complex tumors that need to be significantly reduced in size or removed entirely.
- Aneurysm clipping, where a tiny metal clip is meticulously placed at the base of a brain aneurysm to cut off its blood supply and prevent a rupture.
- Traumatic brain injuries, such as removing blood clots (hematomas) or relieving dangerous swelling.
While it is the most invasive option, a craniotomy often remains the most effective and safest way to address large or difficult-to-reach problems. The direct visualization it provides is essential for protecting critical brain functions during the procedure.
Minimally Invasive Brain Surgery
The next category is a huge leap forward: minimally invasive techniques. These procedures are designed to accomplish the same goals as open surgery but through much smaller openings. This approach dramatically reduces trauma to the surrounding tissues, which often means a faster recovery, less pain, and smaller scars.
A key player here is the endoscope—a thin, flexible tube fitted with a high-definition camera and a light. It’s inserted through a small incision or even a natural pathway, like the nostril, giving the surgeon a crystal-clear, magnified view inside the skull without a large opening.
It’s like a plumber using a tiny camera to find a leak inside a wall instead of knocking the whole thing down. The endoscope lets surgeons “see” and operate in deep, hard-to-reach parts of the brain with incredible precision.
Common minimally invasive approaches include:
- Endoscopic Endonasal Surgery: The surgeon accesses tumors at the base of the skull by navigating through the nasal passages, avoiding any external incisions on the face or scalp.
- Neuroendoscopy: A dime-sized hole is drilled in the skull to insert an endoscope, often used to remove cysts or tumors from the brain’s fluid-filled chambers (ventricles).
- Endovascular Procedures: Instead of opening the skull, a neurosurgeon threads a tiny catheter through blood vessels, usually starting from an artery in the groin, all the way up to the brain to treat aneurysms (coiling) or arteriovenous malformations (AVMs).
This approach beautifully bridges the gap between traditional open surgery and non-invasive methods, offering a powerful, less disruptive option for many patients.
Non-Invasive Brain Procedures
The final category feels like something out of science fiction. Non-invasive procedures are remarkable treatments that require no scalpels and no incisions at all. Instead, they use intensely focused beams of energy to treat problems deep inside the brain from the outside.
The most well-known example is Stereotactic Radiosurgery (SRS). Don’t let the name fool you; despite the word “surgery,” it’s actually a highly advanced radiation therapy technique, not a traditional operation. Using detailed MRI and CT scans, a team of specialists creates a precise, 3D map of the target. Then, hundreds of tiny radiation beams are aimed at that exact spot from many different angles.
Each individual beam is too weak to harm the healthy tissue it passes through on its way. But at the point where all the beams converge—right on the tumor or malformation—their combined energy is powerful enough to destroy the abnormal cells or seal off faulty blood vessels. It’s the ultimate form of precision targeting.
This non-invasive approach is a game-changer for:
- Small, clearly defined tumors located in critical areas or places that are too risky to reach with open surgery.
- Arteriovenous malformations (AVMs).
- Certain functional disorders, like the debilitating facial pain of trigeminal neuralgia.
Because there are no incisions, patients often go home the very same day and get back to their lives much faster than with any other type of brain surgery.
Diving into Highly Specialized Brain Procedures
Beyond the foundational approaches of open or minimally invasive surgery, neurosurgery offers an incredible array of highly specialized procedures. These aren’t general tools; they’re more like custom-designed keys, engineered with immense precision to solve very specific problems within the brain’s complex landscape.
These advanced techniques often come into play when dealing with issues of function, pressure, or the brain’s delicate network of blood vessels. Each one demands a unique skill set and a profound grasp of neuroanatomy, representing some of the most targeted and sophisticated applications in modern medicine.

Restoring Control with Deep Brain Stimulation
For patients living with movement disorders like Parkinson’s disease, essential tremor, or dystonia, the brain’s internal signaling can go haywire, causing debilitating symptoms. Deep Brain Stimulation (DBS) is a remarkable procedure designed to bring order back to these faulty electrical circuits.
Think of it as a pacemaker for the brain. A surgeon implants incredibly thin electrodes into the precise brain regions that govern motor control. These electrodes are then connected by a tiny wire, threaded just beneath the skin, to a small battery-powered device—a neurostimulator—implanted in the chest.
The device sends out continuous, controlled electrical pulses that help regulate the brain’s abnormal activity. While it doesn’t cure the underlying disease, DBS can dramatically improve symptoms, often giving patients back a level of control over their movements that significantly enhances their quality of life.
Relieving Pressure with CSF Shunts
Your brain is cushioned by a clear liquid called cerebrospinal fluid (CSF), which is always circulating. But if this fluid builds up—a dangerous condition known as hydrocephalus—it can create immense pressure inside the skull. This can happen because of a blockage, poor fluid absorption, or the body simply making too much of it.
To fix this, a neurosurgeon can install a CSF shunt. It’s essentially a sophisticated plumbing solution. The shunt is just a thin, flexible tube that creates a new drainage path for the excess fluid.
The process is straightforward:
- Placement: One end of the shunt is carefully placed into one of the brain’s fluid-filled chambers, called ventricles.
- Tunneling: The tube is then tunneled under the skin to another part of the body—most often the abdominal cavity.
- Drainage: A valve connected to the shunt regulates the flow, ensuring just the right amount of fluid is siphoned away to maintain normal pressure. The body then safely reabsorbs the excess CSF.
For both children and adults with hydrocephalus, this is often a life-saving procedure that effectively relieves the pressure that could otherwise damage brain tissue.
Clarifying Diagnosis vs. Treatment
When a scan reveals a suspicious mass in the brain, surgeons have two distinct options: a biopsy or a resection. They might sound similar, but their goals are fundamentally different.
A brain biopsy is purely a fact-finding mission. It’s like a detective collecting a small sample from a crime scene for analysis. The surgeon removes a tiny piece of the abnormal tissue, which is then sent to a pathologist to determine exactly what it is—a benign tumor, a malignant cancer, or something else entirely. This information is absolutely critical for planning the correct treatment.
A tumor resection, on the other hand, is the treatment. The primary goal here is to remove as much of the tumor as can be done safely. It’s a much more extensive operation than a biopsy, aimed squarely at getting rid of the problem’s source.
A biopsy asks, “What are we dealing with?” A resection answers, “Let’s remove it.” The results of the biopsy almost always dictate whether to move forward with a full resection.
Securing Dangerous Blood Vessels
Two of the most critical vascular problems that can occur in the brain are aneurysms and arteriovenous malformations (AVMs). Both involve abnormal blood vessels that pose a high risk of rupturing and causing a devastating bleed or stroke. Neurosurgeons have specialized techniques to make them safe.
Aneurysm Clipping and Coiling A brain aneurysm is a weak, bulging spot on the wall of an artery. The two main ways to secure it are:
- Clipping: This is an open surgical procedure (a craniotomy) where the surgeon places a tiny metal clip across the neck of the aneurysm, sealing it off from blood flow much like a clamp on a hose.
- Coiling: This is a minimally invasive endovascular procedure. A catheter is guided from an artery in the groin all the way up to the aneurysm. Tiny, soft platinum coils are then deposited inside the bulge, which causes the blood to clot and seals off the weak spot from the inside.
Treating Arteriovenous Malformations (AVMs) An AVM is a tangled mess of abnormal arteries and veins that bypass the normal capillary system, creating a high-pressure connection that is prone to bleeding. Treatment options include:
- Surgical Resection: The most direct approach, involving open surgery to carefully disconnect and remove the entire tangle of vessels.
- Endovascular Embolization: A minimally invasive technique where a special glue-like substance is injected into the AVM to block its blood flow. This can be a standalone treatment or used to make a future surgical resection safer.
- Stereotactic Radiosurgery: A non-invasive option that uses highly focused beams of radiation to gradually scar and close off the AVM’s vessels over several months or years.
Deciding on the right technique from this toolbox of highly specialized brain surgeries always comes down to the precise nature of the condition, its location, and the patient’s overall health, highlighting why a deeply personalized surgical plan is so important.
Balancing the Benefits and Risks of Neurosurgery
Deciding to move forward with any of the brain surgery types we’ve covered is a profound moment. It’s a decision reached not through a quick checklist, but through a thoughtful, collaborative conversation between you and your neurosurgeon. This isn’t about just listing potential complications; it’s a careful weighing of the immense potential for a better life against the real risks that come with any neurosurgical procedure.
Every single patient’s situation is unique. Your personal risk profile is a complex mix of the specific surgery you need, your overall health, the hospital’s resources, and, most critically, your surgeon’s deep, specialized experience with your exact condition. The entire goal is to tip that scale—to maximize the benefits while systematically minimizing every single risk.
Understanding the Potential Rewards
While it’s human nature to focus on the “what ifs,” it’s just as important to understand the life-changing benefits that modern neurosurgery makes possible. For many patients, the operation is a turning point—a powerful, definitive intervention that can restore health and give them their life back.
The rewards are often incredibly direct, addressing the very root of a debilitating problem. Depending on your diagnosis, the primary benefits of brain surgery can include:
- Preventing a Catastrophic Event: For conditions like an unruptured brain aneurysm or an AVM, surgery can be a life-saving, proactive measure. It’s about defusing a ticking time bomb before it causes a devastating stroke or hemorrhage.
- Stopping or Reducing Seizures: Removing a tumor or the precise area of brain tissue causing epilepsy can lead to a dramatic reduction—or even complete freedom from—seizure activity.
- Restoring Neurological Function: Simply relieving pressure on the brain, whether it’s from a tumor or excess spinal fluid, can improve everything from your motor control and vision to your ability to think clearly.
- Providing a Definitive Diagnosis: When imaging scans are ambiguous, a biopsy is the only way to get the answers. It provides the crucial tissue sample needed to identify the exact problem and design the most effective treatment plan.
Acknowledging and Managing Potential Risks
Of course, any operation has risks, and brain surgery is no different. But it’s crucial to see these as possibilities, not certainties. Elite surgical teams dedicate their entire process to mitigating these risks through obsessive planning, advanced technology, and decades of experience.
The usual concerns for any surgery apply: infection, bleeding, blood clots, and reactions to anesthesia. Specific to the brain, risks can also involve swelling (edema) or potential changes to neurological function—things like speech, memory, or motor skills. For example, some studies show that seizures are a possible outcome after surgery for glioblastoma, occurring in 20–50% of patients, though this is often well-managed with medication.
It is the surgeon’s core responsibility to anticipate, plan for, and manage these risks. This is where experience and specialization become everything. A top-tier neurosurgeon doesn’t just show up to operate; they leverage advanced imaging to map your critical brain pathways before surgery and use real-time monitoring during the procedure to actively protect your function.
How Top Surgeons Tilt the Balance in Your Favor
The difference between an acceptable outcome and an exceptional one often comes down to how proactively risks are managed. World-class neurosurgeons and their teams at premier medical centers don’t just react to problems—they build an entire system designed to prevent them from ever happening.
This system is built on a few key pillars:
- Hyper-Specialization: A surgeon’s focus and case volume matter immensely. A surgeon who performs hundreds of awake craniotomies for tumors near the speech center has seen and successfully navigated countless challenges. They have refined their technique to a level that a generalist simply cannot match.
- Advanced Pre-Surgical Planning: Using powerful tools like functional MRI (fMRI) and diffusion tensor imaging (DTI), surgeons create a detailed 3D roadmap of your brain. This allows them to identify and meticulously plan a route to the target that avoids critical pathways for language, movement, and sensation.
- Intraoperative Monitoring: During the operation itself, a team of neurophysiologists is constantly watching your brain’s electrical activity. This real-time feedback is like an early warning system, instantly alerting the surgeon to any potential stress on crucial neural networks so they can make immediate adjustments.
This multi-layered approach to safety is what allows you to have a truly meaningful discussion with your doctor. You can move past a generic list of risks and into a personalized understanding of your prognosis and the precise steps being taken to secure the best possible result for you.
Navigating Your Recovery After Brain Surgery
The surgery itself is a major milestone, but the journey truly begins the moment you leave the operating room. Your recovery is an equally critical phase, a time when your body and brain start the intricate process of healing. Understanding what to expect can make all the difference, transforming uncertainty into a structured, manageable plan.

Every recovery is deeply personal. The path forward depends entirely on the specific type of brain surgery you had. A non-invasive radiosurgery procedure might see you home the same day, while a major open craniotomy requires a much more gradual, supported return to daily life.
The First Hours and Days
Immediately after most open or minimally invasive procedures, you’ll be moved to a specialized unit for close observation. This is almost always a Neurosurgical Intensive Care Unit (Neuro ICU) or a similar high-acuity setting where a dedicated team can monitor your vital signs and neurological function around the clock.
This constant monitoring isn’t cause for alarm; it’s a standard safety protocol. The team’s top priorities are managing post-operative pain, watching for any signs of swelling, and ensuring your brain is recovering exactly as expected. While an ICU setting can feel intense, it’s the safest and most controlled environment for this delicate initial phase.
Your recovery is a collaborative effort. An entire team of specialists—from neurologists to physical therapists—works in concert to support your healing, with every step tailored to your personal progress and goals.
This initial hospital stay, which can range from a single night to several days, lays the foundation for the rest of your recovery.
Your Dedicated Rehabilitation Team
As you stabilize, a broader team of experts will join your care. Their focus shifts from immediate post-op safety to actively helping you regain strength, function, and confidence. This multidisciplinary approach ensures every aspect of your well-being is addressed.
Your team will likely include:
- Physical Therapists (PT): These specialists are all about mobility, balance, and strength. They’ll guide you through exercises to safely get you walking and moving again.
- Occupational Therapists (OT): OTs focus on the practical skills needed for daily life—things like dressing, eating, or writing. Their entire goal is to help you reclaim your independence.
- Speech-Language Pathologists (SLP): If your surgery was near language or cognitive centers of the brain, an SLP will be invaluable. They help with any difficulties in speaking, understanding language, or even the mild “brain fog” that can follow surgery.
This integrated team is in constant communication with your neurosurgeon, creating a rehabilitation plan that is both safe and effective, ensuring your progress is steady and sustainable.
Life After Leaving the Hospital
Going home is a huge step. From this point, the recovery timeline varies widely. Someone who had a minimally invasive procedure might feel close to normal within a couple of weeks. For a patient recovering from a major tumor resection, the process could take several weeks to months.
During this time, it’s completely normal to experience fatigue, headaches, or some cognitive slowness. This is simply part of the brain’s healing process. It is absolutely essential to follow your surgeon’s specific instructions on rest, activity restrictions, and when to consider returning to work. Rushing things is counterproductive; giving your brain the time it needs to heal is the fastest way to a full and lasting recovery.
How to Find an Elite Neurosurgeon
https://www.youtube.com/embed/wiYu7pDtlksChoosing your neurosurgeon is, without question, the single most important decision you will make in this entire process. It’s a choice that goes far beyond checking for board certification or a medical school degree. The difference between a good outcome and an exceptional one often comes down to finding the one specialist whose entire career is focused on your specific condition.
Think of it this way: you wouldn’t ask a world-class watchmaker to repair a jumbo jet engine. Both are masters of precision engineering, but their skills are worlds apart and not interchangeable. Neurosurgery operates with the same degree of hyper-specialization, and understanding this is the first step toward securing the right care.
The Power of Sub-Specialization and Case Volume
A general neurosurgeon is a highly trained expert, but an elite specialist has spent their career mastering one specific niche. A vascular neurosurgeon who performs hundreds of aneurysm clippings a year operates in a different universe than a skull base surgeon who has perfected the art of removing complex tumors through the nasal passages. This relentless focus builds an unparalleled depth of experience.
The most revealing metric here is case volume—how many times a surgeon has performed your specific procedure. High repetition isn’t just about practice; it’s about building mastery. It allows a surgeon to anticipate subtle challenges and navigate impossibly delicate anatomy with a practiced, almost intuitive, finesse. When you’re seeking top-tier care, one of your very first questions should be about their direct experience with your exact diagnosis.
A surgeon’s deep specialization is the bedrock of a successful outcome. Every time they perform a procedure like an awake craniotomy, they are adding to a vast library of experience, refining their technique with each repetition to achieve the pinnacle of precision.
This level of focus isn’t just a nice-to-have. For the most complex brain surgery types, it’s absolutely essential for a safe and effective outcome.
Evaluating the Entire Surgical Ecosystem
An exceptional surgeon rarely works alone. They are the conductor of a highly coordinated orchestra, operating within a world-class medical center. The quality of this support system—the entire surgical ecosystem—is just as critical as the surgeon’s individual skill.
As you make your decision, you need to look at the whole picture:
- Advanced Technology: Does the hospital have the latest tools? This includes intraoperative MRI, sophisticated neuro-navigation systems, and real-time monitoring technology designed to protect brain function during surgery.
- Specialized Support Staff: The anesthesiologists, nurses, scrub technicians, and physical therapists should also be neurosurgery specialists. Their familiarity with the unique demands of these procedures enhances safety and streamlines every aspect of your care.
- The Second Opinion as Due Diligence: Seeking a second or even a third opinion isn’t a sign of doubt. It’s a standard, responsible part of making a life-altering medical decision. When you hear a consistent recommendation from multiple top experts, it provides incredible confidence and clarity.
Ultimately, you are choosing a comprehensive program, not just an individual surgeon. By looking into the best neurosurgeons in California and other leading centers, you can see how the very best practitioners are backed by premier institutions. This ensures the care you receive is not only expert but truly holistic.
Common Questions About Brain Surgery
It’s completely normal to have a flood of questions when facing the prospect of brain surgery. Getting clear, straightforward answers is the first step toward feeling in control and confident in your path forward. Here are a few of the most common concerns we hear from patients and their families.
How Long Is the Hospital Stay?
Your time in the hospital really comes down to the complexity of the procedure. For something non-invasive, like stereotactic radiosurgery, you could be home the very same day. For most minimally invasive surgeries, a short stay of just 1 to 3 days is typical.
On the other hand, a major open craniotomy for a complex tumor is a different story. That usually requires a hospital stay of 5 to 10 days, which almost always starts with close monitoring in the Intensive Care Unit (ICU) to ensure the safest possible start to your recovery.
Will My Whole Head Be Shaved?
This is a huge source of anxiety for many, but rest assured, the full head shave is mostly a relic of the past. Modern neurosurgery is far more precise.
Surgeons now typically shave only a very small, specific area right around the planned incision site, and they do it just before the operation begins. This approach keeps the surgical field sterile while minimizing the cosmetic impact for you.
The goal is always to balance surgical safety with your comfort and dignity. Your surgeon will walk you through the exact plan so there are no surprises on the day of your procedure.
Clipping vs. Coiling for an Aneurysm: What’s the Difference?
Both of these techniques are designed to secure a brain aneurysm and prevent it from rupturing, but they go about it in completely different ways.
- Clipping is an open surgical procedure. It involves a craniotomy to access the aneurysm directly so a tiny metal clip can be placed at its base, or “neck.” This effectively cuts off its blood supply from the outside.
- Coiling is a minimally invasive, endovascular procedure. A catheter is guided up from an artery, usually in the groin, all the way into the brain. From there, tiny platinum coils are deposited inside the aneurysm, which causes the blood to clot and seals it off from within.
The decision between them isn’t arbitrary; it depends entirely on the aneurysm’s specific size, shape, and location in the brain. For more guidance on preparing for your procedure, you can explore these essential questions to ask before surgery.
Finding a trusted, world-class specialist is the most critical part of your journey. Haute MD provides a curated network of the nation’s top, board-certified neurosurgeons, connecting you directly with elite practitioners known for precision, innovation, and exceptional outcomes. Discover a leading neurosurgeon in your area through the Haute MD network.

