That sharp, stinging burn inside your nose isn’t just an annoyance. It’s a direct signal from your body that the delicate, sensitive tissues lining your nasal passages are irritated. Most of the time, this raw or stinging feeling points to inflammation of the nasal lining, a tissue known as the nasal mucosa.
What Your Nose Is Trying to Tell You
Think of your nose as the body’s first line of defense—a sophisticated air filter that works around the clock. Its main job is to warm, humidify, and scrub the air you breathe before it ever reaches your lungs. This critical task is handled by the nasal mucosa, a specialized inner lining designed for this very purpose.
But when this system gets overwhelmed by allergens, germs, or environmental pollutants, it kicks off an inflammatory response. That response is what you feel as a burning sensation. It’s a clear sign that this protective barrier has been disrupted, causing swelling, dryness, or a release of chemicals that create that unmistakable discomfort.
The Most Common Triggers Behind Nasal Burning
Several factors can set off this irritating feeling. Getting to the bottom of them is the first step toward finding relief.
- Environmental Factors: Dry air is a major offender, especially in the winter or in buildings with aggressive climate control. It can strip moisture right out of your nasal tissues, leaving them feeling raw and exposed. Smoke, overpowering perfumes, and harsh cleaning chemicals are also common culprits.
- Infections and Allergies: Viral infections like the common cold are notorious for inflaming the nasal passages. Likewise, allergic rhinitis (hay fever) triggers an immune system overreaction to things like pollen, dander, or dust, which directly leads to inflammation and burning.
- Physical Irritation: Sometimes, the cause is purely mechanical. Blowing your nose too aggressively or overusing decongestant nasal sprays can physically damage the delicate mucosa, creating a vicious cycle of burning, irritation, and blockage.
The nasal mucosa is a lot like your skin. If you expose your skin to a harsh chemical, it becomes red, inflamed, and sensitive. The same thing happens inside your nose when it’s hit with irritants or infection—it becomes inflamed and painful.
This guide will help you understand what’s behind that burn, exploring the most common culprits, from seasonal allergies and sinus infections to less obvious irritants hiding in your environment. If you’re experiencing similar sensations elsewhere, you might want to learn more about a general burning skin sensation in our related article.
While we’re focusing on the nose here, learning to interpret your body’s signals is key to your overall health. By identifying the root cause, you can finally move from guessing what’s wrong to finding effective, lasting relief.
Is It Allergies or an Infection?
When your nose starts burning, it’s sending a clear signal that something’s wrong. More often than not, the two main suspects are allergies and infections. While they might feel surprisingly similar at first, they’re fundamentally different problems. Nailing down which one you’re dealing with is the critical first step toward getting relief because each demands a completely different battle plan.
Think of an allergic reaction as a classic case of mistaken identity. Your immune system, your body’s highly-trained security detail, incorrectly flags a harmless visitor—like pollen, dust, or pet dander—as a dangerous threat. It goes into full-on attack mode, unleashing a chemical called histamine that causes that all-too-familiar burning, itching, and sneezing.
An infection, on the other hand, is a real invasion. Viruses (like the common cold) or bacteria (which can escalate to sinusitis) are actively attacking the delicate lining of your nasal passages. Your body fights back with inflammation, which results in swelling, pain, and that raw, burning feeling.
This flowchart can help you visualize how different symptoms point to different root causes, whether it’s allergens, germs, or something else entirely.
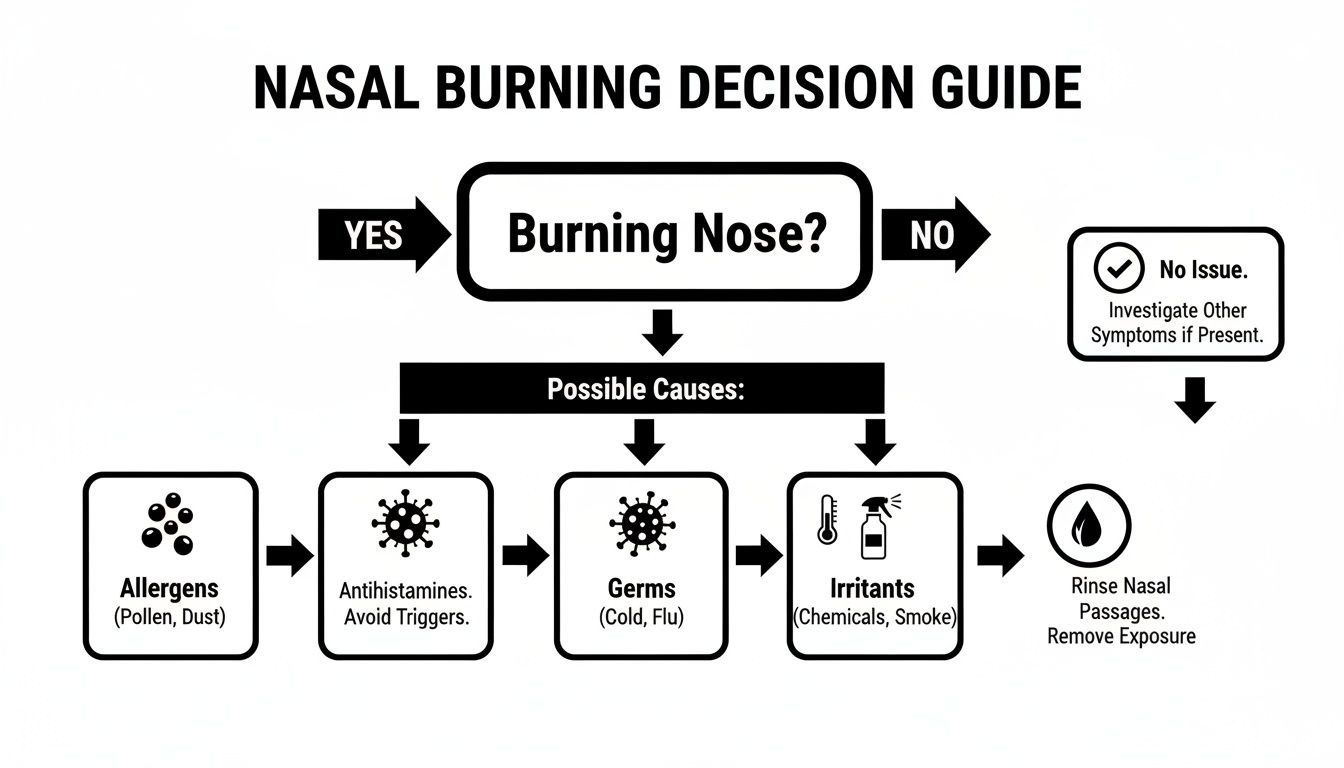
The key takeaway is that the type of symptoms you have—whether they’re itchy and seasonal or come with facial pain and a fever—offers huge clues to what’s really going on inside your nose.
Decoding Your Symptoms: Itchiness vs. Aches
One of the best ways to tell what you’re up against is to take a quick inventory of everything you’re feeling. Each condition leaves behind its own unique fingerprint.
Allergic rhinitis, or hay fever, almost always brings an unmistakable, relentless itch. It’s not just in your nose; you’ll often feel it on the roof of your mouth and, most annoyingly, in your eyes. Any nasal discharge is typically clear, thin, and watery. Allergy symptoms also tend to pop up in response to specific triggers, like a day with a high pollen count or spending time with a furry friend.
Infections tell a different story. They rarely cause that intense itching. Instead, you’re much more likely to feel rundown with body aches, a low-grade fever, and a dull, painful pressure behind your eyes and cheeks. The mucus from an infection is usually thicker and can be yellow or even greenish, particularly with bacterial sinusitis.
A simple rule of thumb: If you’re itching, think allergies. If you’re aching, think infection. It’s not a foolproof diagnosis, but it’s a surprisingly reliable starting point.
For many people, that burning nose is a tell-tale sign of allergic rhinitis. It’s incredibly common. Data from 2021 showed that around 81 million people in the U.S. had been diagnosed with it. That breaks down to about 26% of adults (67 million) and 19% of children (14 million), which shows just how widespread this issue really is.
Timing and Duration Are Key Clues
Another huge tell is the timing. Allergic reactions can hit you like a ton of bricks right after you’ve been exposed to a trigger. And they can stick around for weeks or months, depending on the season—tree pollen in the spring, ragweed in the fall.
A viral infection like the common cold, however, tends to follow a more predictable schedule. Symptoms usually creep in over a day or two, peak around day three or four, and then start to fade within a week to ten days. A bacterial sinus infection might hang on longer, but it often develops on the heels of a viral cold that just wouldn’t quit.
To make it even clearer, let’s put them side-by-side.
Allergies vs. Infections: Distinguishing Your Symptoms
Trying to figure out what’s causing your nasal misery can be confusing. This table breaks down the typical symptom profiles for allergies and infections to help you spot the key differences.
| Symptom | Allergic Rhinitis (Hay Fever) | Viral/Bacterial Infection (Sinusitis) |
|---|---|---|
| Primary Sensation | Itching in nose, eyes, and throat | Aching, pressure, and facial pain |
| Nasal Discharge | Clear, thin, and watery | Thick, often yellow or green |
| Onset | Sudden, often after trigger exposure | Gradual, developing over 1-3 days |
| Associated Symptoms | Sneezing fits, watery eyes | Body aches, fever, sore throat, cough |
| Duration | Can last for weeks or an entire season | Usually resolves in 7-14 days |
Knowing which camp your symptoms fall into is essential for getting the right treatment. If you’re constantly battling that burning, itchy feeling, it’s worth exploring a more targeted strategy for managing your allergies. For a deeper dive, you can learn about Dr. Purvi Parikh’s approach to personalized allergy and asthma treatment. By pinpointing the true cause, you can finally get on the right path to relief—whether that means dodging an allergen or helping your body fight off a bug.
How Everyday Irritants Affect Your Nasal Passages
Infections and allergies get a lot of attention, but often the culprit behind a burning nose is much simpler: the world around you. Your environment is packed with substances that can trigger that raw, irritated feeling, acting like tiny aggressors against the delicate lining of your nasal passages. This isn’t an immune reaction or a virus; it’s a direct physical or chemical assault.

Think of your nasal lining—the mucosa—as a sophisticated filter. It’s designed to warm, humidify, and clean the air you breathe. But when it’s overwhelmed by certain irritants, it becomes inflamed, and the result is a persistent burning sensation that can stick around long after the initial exposure.
The Impact of Your Immediate Environment
Your home or office could be ground zero for nasal irritation. Many common products release invisible particles into the air that directly aggravate the sensitive tissues inside your nose.
Watch out for these frequent offenders:
- Cleaning Products: Bleach, ammonia-based cleaners, and many aerosol sprays release harsh chemicals that can cause an immediate burning feeling.
- Strong Fragrances: That scented candle, air freshener, or perfume might smell nice, but they often contain volatile organic compounds (VOCs) that are notorious for irritating nasal passages.
- Secondhand Smoke: Cigarette smoke is a toxic cocktail of chemicals that actively inflames and dries out your nasal lining.
Even the air itself can be the problem. Dry air from indoor heating in the winter or round-the-clock air conditioning sucks the moisture right out of your nasal passages. This leaves them feeling parched and raw, making them far more susceptible to that burning feeling.
This reaction is known as irritant-induced rhinitis. It’s a non-allergic inflammation caused by direct contact with a bothersome substance. It’s not your immune system overreacting; it’s the tissue itself being physically or chemically damaged.
This is why you might suffer from a burning nose but test negative for every common allergy. The problem isn’t your body’s mistaken defense—it’s a direct injury to the tissue itself.
When Nasal Sprays Become the Problem
It’s a cruel irony, but the very thing you use for relief can become the source of your misery. Over-the-counter decongestant nasal sprays (like those with oxymetazoline) are fantastic for short-term relief from a stuffy nose.
But if you use them for more than three days straight, you risk a rebound effect called rhinitis medicamentosa. Your nasal blood vessels become dependent on the medication. When it wears off, they swell back up with a vengeance, creating a vicious cycle of congestion, overuse, and a chronic, burning irritation.
The Connection to Sinus Inflammation
Constant exposure to these irritants doesn’t just cause temporary discomfort—it can set the stage for bigger problems like sinusitis. When your nasal passages are always inflamed, the drainage pathways from your sinuses can get blocked. Fluid builds up, creating a perfect breeding ground for infection.
This isn’t a minor issue. Nearly 29 million adults in the U.S., which is about 11.6% of the adult population, are diagnosed with sinusitis. The problem is so widespread that over 37 million Americans deal with at least one acute episode each year, making it one of the top reasons people end up at the doctor’s office. You can find more data on the prevalence of sinusitis on fasttrackurgentcare.com.
The first real step toward relief is identifying and minimizing contact with these everyday triggers. By paying attention to the products you use and the quality of the air you breathe, you can dramatically cut down on the things that cause that painful burning sensation in your nose.
Exploring Less Common Causes of Nasal Burning
So you’ve ruled out the usual suspects—allergies, infections, and that new air freshener—but the burning in your nose just won’t quit. When the obvious answers don’t solve the problem, it’s time to dig deeper. Sometimes, the cause isn’t an external trigger at all but an internal issue with the structure or function of your nasal passages.
These less common causes often require a more thorough medical evaluation to uncover. Think of it this way: if the common culprits are rush-hour traffic jams on your daily commute, these issues are the unexpected detours caused by hidden road damage or faulty signals. They aren’t as frequent, but they can bring your comfort to a grinding halt.
Getting familiar with these possibilities is the critical next step, especially when standard remedies have brought you zero relief.
When Nasal Tissues Become Too Dry
One significant but often overlooked condition is atrophic rhinitis. This is a serious problem where the nasal mucosa—the delicate, moist tissue lining your nose—starts to thin out, harden, and essentially waste away. As this vital lining deteriorates, it loses its ability to produce the mucus needed to keep your nasal passages clean and hydrated.
The result is a miserable feeling of extreme dryness, thick, stubborn crusts, and a persistent, uncomfortable burning. It’s as if the natural irrigation system in your nose has completely failed, leaving the tissue raw and irritated. This condition can sometimes develop after nasal surgery or from chronic infections, but in some cases, it appears without a clear cause.
“In cases of severe mucosal dryness, the protective barrier is compromised. This not only causes a burning feeling but also makes the nasal passages more vulnerable to secondary infections, creating a difficult cycle of symptoms.”
Because the tissue isn’t functioning correctly, people with atrophic rhinitis may also notice a foul odor inside their nose or even a diminished sense of smell.
When the Nerves Are Sending Faulty Signals
Sometimes, the problem isn’t with the nasal tissue at all, but with the nerves that serve it. Neuropathic pain happens when nerves start sending incorrect pain signals to the brain, creating a very real sensation of burning, tingling, or aching—even when there’s no physical injury or inflammation.
Imagine a faulty fire alarm that keeps blaring despite there being no smoke or fire. In the same way, the nerves in your nose can become overactive or damaged, constantly telling your brain they’re being burned when there’s no actual trigger. This can lead to a constant, maddening burning that doesn’t respond to typical treatments for allergies or infections.
Diagnosing this kind of pain can be tricky and almost always requires a specialist’s evaluation to pinpoint the nerve-related source.
The Impact of Systemic and Autoimmune Conditions
Your nasal passages don’t exist in a vacuum; they’re connected to your body’s larger systems. This means certain systemic or autoimmune conditions can show up with symptoms like a burning sensation in the nose.
- Sjögren’s Syndrome: This autoimmune disorder is notorious for attacking glands that produce moisture, like those for saliva and tears. It can also target the mucous glands in the nose, leading directly to severe dryness, crusting, and burning.
- Internal Sores or Lesions: Sores inside the nostril, sometimes from conditions like the herpes simplex virus or certain bacterial infections, can create a localized and intense burning pain right at the source.
- Granulomatosis with Polyangiitis (GPA): A rare autoimmune disease, GPA causes inflammation of blood vessels in the nose, sinuses, and throat. This often results in sores, crusting, and a distinct burning feeling as the tissue becomes damaged.
Looking into these less common causes makes one thing clear: a persistent burning sensation in your nose should not be ignored. If your symptoms aren’t getting better with initial treatments, getting a thorough evaluation by an ENT or another specialist is the next logical move to get a real diagnosis and finally find the right path to relief.
Your Action Plan for Soothing Nasal Burning
When you’re dealing with a relentless burning sensation in your nose, you need a clear, methodical game plan to find relief. The strategy is to move from gentle, at-home remedies up to more targeted medical treatments, all while aiming to fix the root cause of the discomfort. Think of it as building a personalized toolkit to calm inflammation, restore moisture, and bring your nasal passages back into balance.

The first step is always the simplest: support your body’s own healing processes. By creating a healthier environment inside your nose, you can often quiet the irritation without immediately reaching for medication. These foundational steps focus on hydration, clearing out irritants, and taming inflammation.
Starting with Gentle Home Care
Before you even think about the pharmacy aisle, start with simple, effective strategies that directly counter the most common culprits, like dry air and irritants. These methods are safe, accessible, and should be the cornerstone of any treatment plan.
Your first line of defense includes:
- Using a Humidifier: Dry air is a major offender. Running a humidifier, especially in your bedroom overnight, adds crucial moisture to the air, preventing the delicate lining of your nose from drying out and feeling raw.
- Practicing Saline Rinses: A gentle saline spray or a neti pot can work wonders. This simple act literally washes away allergens, dust, and thick mucus that might be causing the fire. It’s also a great way to hydrate the nasal passages directly.
- Trying Steam Inhalation: Breathing in steam from a hot shower or a bowl of hot water provides immediate, soothing relief. The warm, moist air helps reduce inflammation and calm irritated tissues almost instantly.
Think of these home care steps like basic maintenance for your car’s air filter. A clean, hydrated filter works better. Saline rinses and humidifiers help keep your nose’s natural filtering system in optimal condition.
Moving to Over-the-Counter Solutions
If home remedies aren’t cutting it, the next logical step is to explore over-the-counter (OTC) options. These products are designed to tackle specific problems like allergies or inflammation more directly. The key is to match the product to what you think is causing the problem.
For example, if you suspect allergies are the trigger behind your burning sensation in nose, an antihistamine is your best bet. But if it’s pure inflammation without the sneezing and itching, you’ll need a different approach.
Here are the most common OTC categories:
- Antihistamines: If the burning comes with an itchy nose, sneezing, and watery eyes, an oral antihistamine (like loratadine or cetiririzine) can be incredibly effective. It works by blocking the chemical reaction causing your misery.
- Corticosteroid Nasal Sprays: For stubborn inflammation from allergies or general irritation, sprays like fluticasone or triamcinolone are a powerful choice. They work right where the problem is—inside your nose—to reduce swelling and irritation.
When to Consider Prescription Treatments
When you’ve tried the home care and OTC routes and the burning still won’t quit, it’s time to see a doctor. Getting a proper diagnosis is critical, because persistent symptoms can signal an underlying issue that needs a targeted medical attack. This is especially true when you need to figure out if you’re fighting a virus or a bacterial infection.
Viral and bacterial infections are major causes of a burning sensation in the nose and throat, affecting millions of people every year. Telling them apart is clinically important because bacterial infections often need antibiotics, while viral ones just need supportive care while they run their course. You can learn more about how these infections contribute to throat and nasal burning from Liv Hospital. A doctor has the tools to determine the precise cause and get you on the right treatment path.
Depending on their diagnosis, your doctor might recommend:
- Prescription-Strength Nasal Sprays: These are more potent versions of steroid or antihistamine sprays that can deliver greater relief for severe inflammation or allergies.
- Antibiotics: If a bacterial sinus infection is identified as the source of the burning and pressure, a course of antibiotics is necessary to wipe out the infection.
- Neuropathic Pain Medications: In less common cases where the burning is traced back to nerve issues (neuropathic pain), your doctor might prescribe specific medications like gabapentin or amitriptyline that target nerve pain signals.
By following this action plan—starting with gentle care and escalating only as needed—you can systematically figure out what works for you. This structured approach ensures you find the most effective and appropriate solution for your situation, helping you get back to breathing easy.
When to See a Doctor for Your Symptoms
Plenty of cases of a burning nose can be handled at home with simple remedies. But it’s absolutely critical to know when your body is signaling a bigger problem that needs a professional.
Think of a mild, temporary burning sensation as a yellow traffic light—a heads-up to pay attention. Certain symptoms, however, are a hard red light. It’s time to stop self-treating and call a specialist.
Ignoring persistent or severe symptoms can turn a manageable issue into a chronic condition. Getting a timely evaluation from an Ear, Nose, and Throat (ENT) specialist or an allergist is the fastest way to get an accurate diagnosis and, more importantly, a targeted treatment plan that actually works.
Identifying Your Red Flag Symptoms
Some signs just can’t be ignored. They suggest the burning in your nose might be tied to a serious infection, a structural problem, or another underlying medical condition that needs an immediate look.
Pay close attention if your nasal burning comes with any of the following:
- Symptoms lasting more than 10 days without any improvement.
- A high fever that just won’t break or doesn’t respond to over-the-counter meds.
- Severe or worsening headache or facial pain, especially if it’s focused around your eyes, forehead, or cheeks.
- Vision changes, like blurry vision, seeing double, or pain when you move your eyes.
- Swelling or redness around your eyes, across your nose, or on your face.
- Thick, green, or yellow nasal discharge paired with significant sinus pressure.
These symptoms could point to a severe bacterial sinus infection or another condition that requires prompt medical intervention to keep things from getting worse.
What to Expect During a Specialist Visit
When you finally see a specialist for that nagging burning in your nose, their goal is to get past the guesswork and find the real cause. Your appointment will be a deep dive into your nasal health, starting with a detailed conversation.
Be ready to talk about:
- The exact nature of your symptoms—is it burning, stinging, or more of a raw feeling?
- The timing and duration of the discomfort.
- Any triggers you’ve noticed, like specific places, foods, or even seasons.
After you talk, the doctor will do a physical exam, which might involve using a small, lighted tool to look inside your nostrils.
In many cases, an ENT will perform a nasal endoscopy. This is a simple in-office procedure where they use a thin, flexible tube with a tiny camera to get a clear, magnified view of your entire nasal passage and sinus openings. It’s the best way to spot inflammation, polyps, or structural issues you’d otherwise miss.
Depending on what they see, your specialist might recommend more tests to get the full picture. This could mean allergy testing to pinpoint specific triggers, a CT scan to get a detailed look at your sinus cavities, or a nasal culture to check for a bacterial infection.
Some complex cases might point toward a different specialist altogether. For instance, you can learn more about how to find a mast cell specialist near you if a broader immune system response is suspected. Getting the right diagnosis is the single most important step toward finding a solution that finally brings you relief.
Burning Nose FAQs
When your nose is on fire, you want answers—fast. It’s a uniquely irritating sensation, and it’s natural to wonder what’s behind it and what you should do next. Here are some straightforward answers to the most common questions we hear.
Can Stress Cause a Burning Sensation in My Nose?
While stress won’t directly light a match in your sinuses, it absolutely pours fuel on the fire. When you’re under intense pressure, your immune system takes a hit, making you a prime target for the very sinus infections that cause that burning misery.
Beyond that, stress acts like a volume knob for pain perception. A minor irritation you might otherwise ignore can suddenly feel intense and all-consuming. And don’t forget the stress-reflux connection; for some, stress triggers acid reflux, which can send acidic vapors creeping up into the back of your nasal passages, creating a distinct chemical-like burn.
Why Does My Nose Burn Only on One Side?
If the burning is a one-sided affair, it’s almost always a sign of a localized problem, not something systemic like widespread allergies. Think of it as a specific trouble spot.
Common culprits for one-sided burning include:
- A pimple, sore, or a tiny cut inside one nostril.
- A structural issue like a deviated septum, which can mess with airflow and create severe dryness on just one side.
- A foreign object stuck in the nasal passage (a classic, especially with kids).
- A developing nasal polyp or a contained infection brewing in a single sinus cavity.
If you’re dealing with persistent, one-sided nasal burning, it’s smart to have an ENT specialist take a look. They can do a quick in-office exam to rule out any anatomical quirks or specific issues that need targeted treatment.
Is a Burning Nose a Sign of COVID-19?
During the pandemic, that strange “fizzy” or burning feeling in the nose became a well-known early sign of COVID-19, often showing up right alongside the loss of smell and taste. The virus is known to directly inflame the delicate nasal lining, which triggers this bizarre sensation.
However, this symptom is hardly exclusive to COVID-19. Plenty of other respiratory viruses, from the common cold to various flu strains, can create the exact same feeling. So, while a burning sensation in the nose can be a sign of COVID-19, it’s not a slam dunk. It’s one piece of the puzzle that has to be considered with other classic symptoms like fever, cough, and body aches.
Finding the right specialist is the most important step toward getting an accurate diagnosis and effective treatment. Haute MD connects you with a curated network of the nation’s top, board-certified physicians in fields like allergy, immunology, and otolaryngology. Search our directory to find a leading doctor near you who specializes in providing premium, outcome-driven care. Find your specialist here.

