Ever wondered how doctors can see a hairline fracture in your wrist or spot a tiny tumor deep inside the brain without making a single cut? That’s the world of diagnostic radiology. It’s the medical field that uses sophisticated imaging—like X-rays and MRI scans—to peer inside the human body, giving doctors the critical information they need to diagnose, monitor, and sometimes even treat diseases.
Think of it as a form of high-tech medical investigation.
Seeing Inside the Body: An Introduction to Diagnostic Radiology

Imagine a medical detective trying to solve a complex mystery hidden within the body’s intricate systems. Instead of a magnifying glass, this expert wields powerful machines that capture detailed visual clues. This is the very essence of diagnostic radiology—it’s the art and science of interpreting medical images to uncover the root cause of your symptoms.
These “detectives” are highly specialized medical doctors called radiologists. After medical school, they complete years of rigorous training to master the skill of analyzing images from various technologies. Their findings are often the missing piece of the puzzle, providing the definitive evidence your primary doctor needs to build an effective treatment plan.
From Symptoms to Solutions
The journey almost always starts with a symptom—that persistent cough, an aching joint, or a series of unexplained headaches. To figure out what’s really going on, your doctor needs to look beyond what they can see and feel on the surface. Diagnostic radiology provides that indispensable window into your body.
The field serves a few critical functions:
- Pinpointing Injuries: It can identify the exact location and severity of bone fractures, torn ligaments, or internal bleeding with stunning precision.
- Detecting Diseases: It often spots the early signs of conditions like cancer, heart disease, or neurological disorders long before they would otherwise become obvious.
- Monitoring Treatment: Doctors use it to track the progress of a condition, like watching a tumor shrink in response to chemotherapy.
- Guiding Procedures: It provides a real-time visual map for surgeons and other specialists during minimally invasive operations, making them safer and more accurate.
At its core, diagnostic radiology bridges the gap between a patient’s symptoms and a clear, actionable diagnosis. It transforms medical guesswork into a precise science, delivering the clarity needed to make confident healthcare decisions.
Without the insights from this specialty, much of modern medicine would be flying blind. Radiologists and the images they interpret are fundamental to nearly every area of patient care, from the chaos of the emergency room to the quiet focus of an oncology clinic. They deliver the visual proof that confirms a diagnosis, guides treatment, and ultimately helps ensure the best possible outcome for your health.
The Evolution of Medical Imaging: From X-Rays to AI
The story of diagnostic radiology isn’t a dry clinical timeline; it’s a narrative of scientific grit and relentless progress that fundamentally remade medicine. It began not in a sterile lab, but with an accidental discovery that lit up the human body in a way no one thought possible.
This journey from a shadowy black-and-white image to today’s high-definition, AI-assisted scans is the key to understanding the power behind a modern diagnosis.
It all started in 1895 with German physicist Wilhelm Conrad Röntgen. While experimenting with cathode rays, he noticed a mysterious glow emanating from a chemically coated screen across his lab. These unknown rays, which he aptly named “X-rays,” could pass straight through solid objects—including human tissue—but were stopped by denser materials like bone.
Within months, physicians were using this strange new technology to see inside their patients, visualizing fractures and locating foreign objects without a single incision. Just like that, diagnostic radiology was born.
Expanding the Diagnostic Horizon
For decades, the X-ray was the only game in town for peering inside the body. But the mid-20th century saw an explosion of new ideas, each leveraging different physical principles to paint an even clearer picture of our internal anatomy. This period laid the groundwork for the powerful tools we rely on today.
The key breakthroughs came in rapid succession:
- Ultrasound in the 1950s: Originally adapted from sonar technology used in World War II, medical ultrasound uses high-frequency sound waves to create real-time images. It proved to be a safe, radiation-free way to visualize soft tissues, organs, and, most famously, the developing fetus during pregnancy.
- Computed Tomography (CT) in 1971: The first patient brain CT scan was a landmark event. By combining a series of X-ray images taken from different angles, the CT scanner created cross-sectional “slices” of the body, offering a three-dimensional perspective that was previously unimaginable.
- Magnetic Resonance Imaging (MRI) in 1977: The first human MRI scan introduced a completely new way of seeing. Using powerful magnets and radio waves, MRI could produce breathtakingly detailed images of soft tissues like the brain, muscles, and ligaments, all without using any ionizing radiation.
These weren’t just incremental improvements; they were monumental leaps that transformed diagnostics from a practice of educated guesswork into one of remarkable precision. Each new technology gave doctors a sharper, more specific view of disease and injury.
From Innovation to Standard of Care
This rapid expansion has made diagnostic radiology an indispensable part of modern medicine. In just over a century, the field has grown from a single accidental discovery into a suite of advanced technologies that underpin the vast majority of clinical decisions in major health systems.
Today, it’s estimated that diagnostic imaging influences a staggering 80–90% of hospital-based care pathways—a testament to its central role. You can explore the ARRT timeline to see just how far we’ve come.
This legacy of innovation is far from over. The journey from Röntgen’s faint images to the AI-enhanced scans of today shows an unwavering commitment to seeing the human body with ever-greater clarity. For patients, this history provides the assurance that when they step into a scanner, they are benefiting from more than a century of scientific advancement dedicated to getting the diagnosis right.
A Look Inside the Radiologist’s Toolkit
To really get what diagnostic radiology is all about, we have to look at the remarkable technologies that let radiologists see inside the human body. Each imaging method, or modality, works differently, offering a unique window into your health. It’s like a master mechanic’s workshop; you wouldn’t use a wrench to measure an engine’s timing, and a doctor won’t order an X-ray when an MRI is the only tool that can properly see a torn ligament.
Choosing the right tool is the critical first step toward a precise diagnosis. Let’s pull back the curtain on the primary technologies in the radiologist’s toolkit, breaking down how they work and what they help your doctor find.
This visual guide shows the evolution of some of the most influential imaging tools that have defined modern medicine.
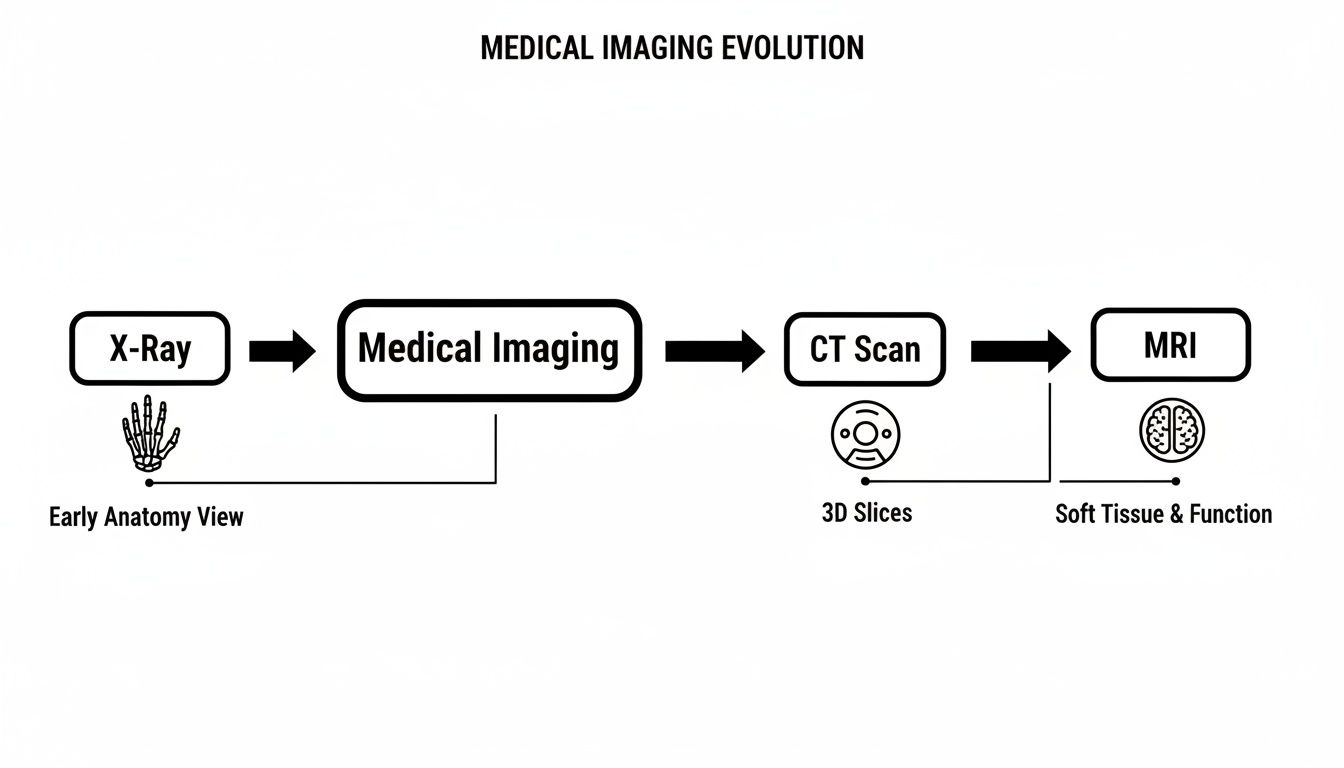
You can see how each technology built upon the last, taking us from seeing dense structures like bone to capturing incredibly fine details in soft tissue and the brain.
The Classic Workhorse: X-Ray
The X-ray, or radiograph, is the oldest and most familiar form of medical imaging. It’s a straightforward process: a small, controlled amount of ionizing radiation passes through the body. Denser materials, like bone, block more of the radiation and show up as white on the final image. Softer tissues let more of it pass through, appearing in shades of gray.
This makes X-rays exceptionally good for:
- Identifying bone fractures and breaks with fantastic clarity.
- Spotting certain lung conditions, like pneumonia or a collapsed lung.
- Detecting dental issues like cavities and impacted teeth.
Because it’s fast and widely available, the X-ray is often the first test ordered in an ER or for an initial look at bone and chest issues. It gives a quick, foundational snapshot of the body’s structural framework.
The 3D Detective: Computed Tomography (CT)
A Computed Tomography (CT) scan is a much more powerful application of X-ray technology. Instead of one flat image, a CT scanner takes a series of X-ray pictures from hundreds of different angles as it rotates around you. A powerful computer then pieces this data together to create detailed cross-sectional images, or “slices,” of your body.
Imagine being able to digitally slice a loaf of bread to see every detail inside. That’s what a CT scan does for your organs, blood vessels, and bones, letting radiologists examine your anatomy layer by layer.
This 3D perspective makes CT scans ideal for:
- Diagnosing internal injuries from trauma, like bleeding in the brain or organ damage.
- Pinpointing tumors, abscesses, and other abnormalities in the chest, abdomen, and pelvis.
- Visualizing blood vessels to find blockages or aneurysms, often with the help of a contrast dye.
The Soft Tissue Specialist: Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) is in a class of its own. It uses no ionizing radiation at all. Instead, it combines a powerful magnetic field and radio waves to generate breathtakingly clear images of the body’s soft tissues.
Here’s the basic idea: your body is mostly water. The MRI machine’s magnet temporarily aligns the water molecules in your body. When radio waves are pulsed through, these molecules are knocked out of alignment. As they snap back into place, they emit signals that a computer translates into a detailed image.
This process gives MRI an unmatched ability to tell the difference between various types of soft tissue. It’s the undisputed champion for:
- Examining the brain and spinal cord for conditions like tumors, multiple sclerosis, or herniated discs.
- Visualizing joints, ligaments, and tendons, making it essential for diagnosing sports injuries like a torn ACL.
- Assessing organs like the liver, kidneys, and heart with incredible precision.
The detail is so fine that an MRI can show subtle differences between healthy and diseased tissue that other scans would almost certainly miss, making it indispensable for neurology, orthopedics, and oncology.
Seeing Function With Nuclear Medicine
While X-rays, CTs, and MRIs are brilliant at showing anatomy (what your body looks like), nuclear medicine is designed to show physiology (how your body works). This advanced field uses tiny amounts of radioactive materials, called radiotracers, to see disease at the molecular level.
A radiotracer is usually injected, swallowed, or inhaled. It travels through the body and collects in the specific organ or tissue being studied. A special camera then detects the energy given off by the tracer, creating images that map out biological activity.
Two of the most common nuclear medicine scans are:
- PET Scans (Posron Emission Tomography): A cornerstone of modern cancer care, PET scans can light up areas of high metabolic activity, a tell-tale sign of a growing tumor.
- Bone Scans: These can reveal bone cancers, infections, or tiny fractures that aren’t visible on a standard X-ray.
By focusing on function instead of just structure, nuclear medicine provides a uniquely powerful diagnostic view. For those interested in this cutting-edge field, learning more about the role of a nuclear medicine doctor reveals how it is merging diagnosis with therapy—a concept known as “theranostics.”
To help clarify the role of each primary imaging tool, this table provides a quick side-by-side comparison.
Comparing Key Medical Imaging Modalities
A quick-reference comparison of the primary diagnostic imaging technologies, outlining their core principles, primary uses, and key considerations for patients.
| Modality | How It Works | Best For Visualizing | Key Patient Consideration |
|---|---|---|---|
| X-Ray | Passes a small amount of ionizing radiation through the body to create a 2D image. | Bones, certain lung conditions (pneumonia), dense objects. | Very fast and widely available; low radiation dose. |
| CT Scan | Uses a rotating series of X-rays to create detailed 3D cross-sectional “slices.” | Internal injuries, tumors, blood clots, complex bone fractures. | Provides much more detail than X-ray; uses a higher radiation dose. |
| MRI | Employs a powerful magnetic field and radio waves to create highly detailed images. | Soft tissues like the brain, spinal cord, muscles, ligaments, and tendons. | No radiation; can be loud and feel enclosed; may not be suitable for patients with certain metal implants. |
| Ultrasound | Uses high-frequency sound waves to create real-time images of organs and blood flow. | Organs (liver, kidneys), developing fetus, blood vessels, guiding biopsies. | No radiation, very safe, and portable; image quality can be operator-dependent. |
| PET Scan | A radioactive tracer is injected to highlight areas of high metabolic activity. | Cancer (staging and response), brain disorders, heart conditions. | Shows biological function, not just anatomy; involves a small radiation dose from the tracer. |
| Fluoroscopy | A continuous X-ray beam creates a “movie” of the body in motion. | Digestive tract (barium swallow), blood vessel blockages, guiding joint injections. | Shows movement in real-time; radiation dose varies with procedure length. |
Each of these technologies gives physicians a different piece of the puzzle, and the skill of the radiologist lies in knowing exactly which one to use to get the clearest picture of what’s happening inside you.
The Critical Role of the Radiologist
The powerful imaging technologies we’ve explored are truly remarkable, but they are only half the story. An MRI or CT scanner produces incredibly detailed pictures, yet those images are essentially complex data sets—silent and meaningless without an expert interpreter. This is where the radiologist, a highly specialized medical doctor, steps in.
They are the human intelligence that transforms pixels into a diagnosis. An image is only as valuable as the mind analyzing it. The radiologist is the indispensable “medical detective” who meticulously examines every detail, searching for the subtle clues that point to injury or disease. Their work is a blend of deep scientific knowledge and sharp observational skill, honed over more than a decade of intense education and training.
The Rigorous Path to Becoming an Expert Interpreter
Becoming a radiologist is one of the most demanding journeys in medicine. It’s a commitment that ensures every report you receive is backed by an exceptional level of expertise. This extensive process is designed to create physicians who can reliably identify thousands of conditions from images alone.
The typical path includes:
- Four years of medical school, providing a broad foundation in all aspects of human health and disease.
- A one-year medical or surgical internship, offering hands-on clinical experience with patients.
- A four-year diagnostic radiology residency, which involves intensive, focused training in interpreting all imaging modalities. During this time, a resident will interpret hundreds of thousands of images under expert supervision.
The American Board of Radiology (ABR) ensures these high standards are met through a rigorous board certification process. This certification is a critical credential, signifying that a radiologist has demonstrated the knowledge and skill required for high-quality practice.
But for many, the training doesn’t stop there.
The Power of Subspecialization
After residency, many radiologists pursue a fellowship, dedicating another one to two years to mastering a specific area of the body or disease type. This is where true mastery is developed. Think of it like the difference between a general contractor and a master cabinet maker; both are skilled, but one has a focused expertise that is unmatched in their specific craft.
Common subspecialties include:
- Neuroradiology: Focusing on the brain, spine, head, and neck.
- Musculoskeletal (MSK) Radiology: Specializing in joints, bones, muscles, and sports injuries.
- Breast Imaging (Mammography): Concentrating on detecting and diagnosing breast cancer.
- Body Imaging: Centered on the abdomen and pelvis, including organs like the liver and kidneys.
- Pediatric Radiology: Focusing exclusively on diagnosing conditions in infants and children.
This subspecialty training is what separates a good diagnosis from a great one. A fellowship-trained neuroradiologist might spot a subtle brain abnormality that a general radiologist could overlook. Similarly, an MSK specialist can provide a far more nuanced interpretation of a complex knee injury.
When they analyze an image, they bring a depth of experience with thousands of similar cases, allowing them to recognize even the faintest patterns of disease. For instance, after a mammogram and a subsequent biopsy, the insights from a breast imaging specialist are vital. Understanding what comes next is crucial, and you can learn more by reading a guide to care after a breast biopsy for a clearer picture of the patient journey.
In essence, the radiologist acts as a crucial consultant to your entire medical team. They provide the definitive answers your doctor needs to create an effective treatment plan, making their role absolutely central to your care. Choosing a provider who employs subspecialist radiologists ensures you benefit from the highest possible level of diagnostic accuracy.
How Imaging Guides Minimally Invasive Treatments
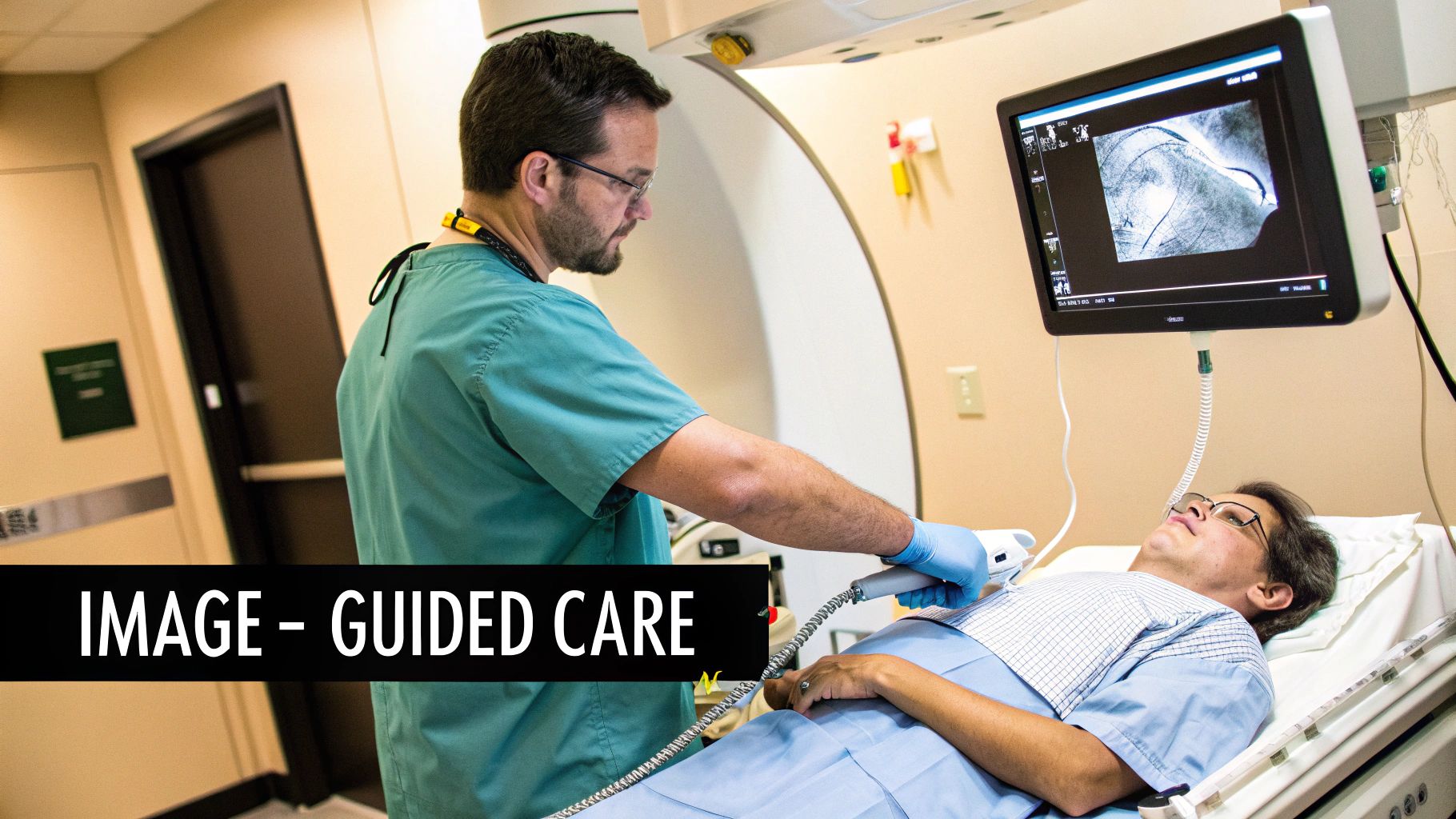
Diagnostic radiology isn’t just about finding problems—it’s also about fixing them with incredible precision. This is the world of interventional radiology, an exciting field where radiologists step out from behind the screen and become active participants in your treatment.
These specialists use their deep knowledge of imaging to perform minimally invasive procedures that, not long ago, would have required open surgery.
Think of an interventional radiologist as a medical navigator with a real-time, high-definition map of your body. Using live imaging from technologies like ultrasound, fluoroscopy (a type of moving X-ray), or CT scans, they can guide tiny instruments—needles, wires, and catheters—through your blood vessels or directly to a target deep inside your body.
This image-guided approach allows for incredibly complex treatments to be performed through an incision no larger than a pinprick. The result is a profound shift in patient care, moving away from large surgical wounds and toward safer, faster, and less painful solutions.
From Diagnosis to Direct Intervention
The applications for interventional radiology are stunningly broad, addressing conditions all over the body with remarkable accuracy. Instead of major surgery, these targeted treatments offer powerful, effective alternatives.
Radiologists can now directly intervene in ways that were pure science fiction just a few decades ago.
Some of the most compelling examples of image-guided procedures include:
- Tumor Ablation: Radiologists insert a special needle-like probe directly into a cancerous tumor in the liver, kidney, or lung. Using either extreme heat (radiofrequency ablation) or cold (cryoablation), they destroy cancer cells without harming surrounding healthy tissue.
- Uterine Fibroid Embolization: To treat noncancerous uterine fibroids, a radiologist guides a catheter to the arteries supplying them with blood. They then inject tiny particles to block these arteries, causing the fibroids to shrink and symptoms to resolve—all without a hysterectomy.
- Chemoembolization: For certain liver cancers, chemotherapy drugs can be delivered directly to the tumor through a catheter. This method concentrates the powerful medicine exactly where it’s needed, maximizing its effect while minimizing side effects elsewhere in the body.
The Benefits for the Patient
The move toward minimally invasive techniques is a massive leap forward in patient-centered care. By avoiding the trauma of open surgery, interventional radiology delivers huge advantages that improve both safety and quality of life. The impact is felt almost immediately and can completely change the recovery experience.
The core principle is simple: achieve the same or better clinical outcome with less impact on the body. This means less pain, fewer risks, and a dramatically shorter recovery period.
For patients, the benefits are crystal clear:
- Reduced Pain and Scarring: Small incisions mean far less post-procedure pain and almost no scarring compared to traditional surgery.
- Lower Risk of Complications: Less trauma to the body significantly reduces the risk of infection and other complications tied to large surgical wounds.
- Faster Recovery Times: Many of these procedures are done on an outpatient basis. Patients often return to their normal lives in days, not the weeks or months required after major surgery.
This accelerated healing is especially valuable in fields like orthopedics, where patients are desperate to regain mobility. To see the difference, exploring the recovery from minimally invasive spine surgery recovery highlights just how much these methods have transformed patient outcomes. Interventional radiology truly embodies the future of medicine—smarter, safer, and far more precise.
The Future of Diagnostic Radiology
The relentless innovation that defined radiology’s first century is now hitting an inflection point. Two advances, in particular, are pushing the boundaries of what’s medically possible: Artificial Intelligence (AI) and a revolutionary field called Theranostics.
These aren’t just incremental improvements; they are fundamentally reshaping how we find, understand, and ultimately treat disease.
To grasp the scale of this change, consider the sheer volume of data. In the late 2010s, American hospitals were performing an estimated 84 million CT scans and over 40 million MRI exams every single year. That’s a staggering increase from virtually zero before the 1970s and 80s—a trend of double-digit annual growth that shows the incredible expansion in medical imaging. You can explore the history and innovation of medical radiation to fully appreciate this journey.
This explosion of information has created the perfect environment for AI to make a massive impact.
AI as the Radiologist’s Super-Powered Assistant
Let’s be clear: AI isn’t coming to replace radiologists. It’s emerging as an incredibly powerful partner—a tireless assistant that can analyze thousands of scans in seconds, recognizing subtle patterns that might be invisible to the human eye. This is poised to dramatically improve both diagnostic speed and accuracy.
Here’s how it works in the real world:
- Catching Disease Earlier: AI excels at spotting the almost-imperceptible signs of early disease. Think of tiny lung nodules or the faintest abnormalities on a mammogram. Finding these sooner means starting treatment when it’s most effective.
- Smarter Workflows: By automatically flagging urgent cases for immediate review or handling routine measurements, AI frees up radiologists to dedicate their expertise to the most complex and nuanced diagnostic challenges.
- Predictive Insights: The most advanced AI models go beyond simple detection. They can analyze imaging features to help predict how a disease might progress or which specific treatments are most likely to work for a particular patient.
Think of AI as an ever-vigilant collaborator, providing a second set of expert eyes on every single scan. This human-machine teaming enhances the radiologist’s ability to deliver a more precise, confident, and timely diagnosis.
Theranostics: Seeing and Treating at the Molecular Level
Another mind-bending frontier is Theranostics, a name that perfectly blends “therapy” with “diagnostics.” This represents a monumental shift toward truly personalized medicine, especially in cancer care. The concept is as elegant as it is powerful: use one molecule to see a specific target on cancer cells, then use a nearly identical molecule to treat only those cells.
It’s a two-step “see it, treat it” process.
First, a patient gets a diagnostic scan (often a PET scan) using a tracer engineered to bind to a unique protein found only on their tumor cells. If the scan lights up, it’s confirmation—the target is there.
Next, a therapeutic agent is administered. It’s a near-identical molecule, but this one carries a potent radioactive payload. This “magic bullet” travels through the body, seeking out and delivering targeted radiation directly to the cancer cells while leaving healthy tissue almost completely untouched.
This approach ensures that powerful therapies are given only to the patients who will actually benefit, maximizing effectiveness and dramatically reducing side effects. It’s a perfect example of how the future of radiology is becoming more integrated, more intelligent, and deeply personal.
Common Questions About Diagnostic Radiology
It’s completely normal to have questions before an imaging scan. Feeling prepared is a huge part of the process, so let’s walk through some of the most common things patients ask.
Getting clear, direct answers can help demystify the experience and put your mind at ease.
Is Radiation From X-Rays and CT Scans Dangerous?
This is a totally valid and important question. Yes, X-rays and CT scans use ionizing radiation, but the doses in modern medical imaging are tiny and meticulously controlled. Radiologists live by a principle called ALARA—As Low As Reasonably Achievable.
Your doctor always weighs the very small potential risk against the massive benefit of getting a clear and accurate diagnosis. For a single scan, the risk is generally considered extremely low. Still, you should always feel comfortable asking your physician to explain why the scan is crucial for your specific situation.
Why Do I Need an Injection of Contrast Dye for My Scan?
Think of contrast material—often called “dye”—like turning on a floodlight in a dark room. It’s a special substance that dramatically highlights certain organs, blood vessels, or tissues, making them pop on the final images with incredible clarity.
For example, a contrast agent in a CT scan can light up your arteries, making it easy to spot a dangerous blockage. It allows the radiologist to see subtle details that might otherwise be invisible, leading to a much more precise and confident diagnosis.
What Is the Difference Between a Radiologist and a Technologist?
This is a key distinction that trips a lot of people up. They are two different experts with two critical roles.
The Radiologic Technologist is the highly skilled medical professional who positions you correctly and operates the complex imaging equipment. Their expertise is in capturing the perfect, high-quality images your doctor needs.
The Radiologist is the medical doctor who has gone through years of specialized training to interpret those images. They analyze the visual evidence, spot signs of injury or disease, and write the detailed diagnostic report that guides your treatment.
Think of it this way: The technologist is the expert photographer capturing the scene, while the radiologist is the master detective who solves the clinical puzzle using that photographic evidence.
How Should I Prepare for My Imaging Appointment?
Preparation really depends on the specific scan you’re having. For some procedures, like an abdominal ultrasound or certain CT scans, you might need to fast—meaning nothing to eat or drink—for several hours beforehand.
For an MRI, the main rule is no metal. You’ll need to remove all jewelry, piercings, and any clothing with metal zippers or buttons. Your imaging center or doctor’s office will give you very specific instructions ahead of time. Following them to the letter is the best way to ensure top-quality results and keep your appointment running on schedule.
Finding a physician who practices at the forefront of medical science is essential for receiving the best care. Haute MD provides a curated network of the nation’s most respected, board-certified specialists who are leaders in their fields. Discover an elite provider dedicated to precision, innovation, and exceptional patient outcomes by exploring the Haute MD network.

