Seeing a little blood mid-cycle can be unsettling, but it’s often a completely normal—and even reassuring—sign of a healthy, functioning reproductive system. This light spotting, known as ovulation bleeding, is typically a direct result of the rapid hormonal shifts that trigger the release of an egg.
Decoding Mid-Cycle Spotting
Think of your uterine lining (the endometrium) like a carefully prepared garden bed, waiting for a seed. It needs a steady supply of hormonal “water”—specifically estrogen—to stay thick, lush, and stable.
Right before ovulation, estrogen surges to a peak. But immediately after the egg is released, estrogen levels take a brief, sharp dip before progesterone rises to take over. This momentary hormonal dip is like turning off the sprinkler for just a second. It can cause a tiny part of that lush lining to shed, resulting in the light spotting you might see on your toilet paper or underwear.
For many women, this spotting is actually a positive indicator of fertility, not a cause for alarm. It’s a real-time signal that your body is doing exactly what it’s supposed to do.
How Common Is Ovulation Bleeding?
You might be surprised to learn how frequently this happens. Research shows that ovulation bleeding affects a significant number of women, with studies reporting that anywhere from 4.8% to 30% of women experience it.
One key study found that women who had mid-cycle spotting also had significantly higher peak levels of luteinizing hormone (LH) and estrogen—the exact hormones that drive ovulation. This strongly suggests the bleeding is tied to a robust ovulatory event. You can delve deeper into the science behind ovulation bleeding on avawomen.com.
It’s crucial to know how to distinguish this harmless spotting from your actual period or other types of bleeding.
Ovulation Spotting vs Menstrual Period At a Glance
Here’s a quick reference table to help you tell the difference at a glance. Understanding these distinctions is the first step in learning to interpret your body’s unique signals.
| Characteristic | Ovulation Spotting | Menstrual Period |
|---|---|---|
| Timing | Mid-cycle (around days 14-16) | The very beginning of your cycle (Day 1) |
| Volume | Very light; often just a few drops or streaks | A heavier flow requiring pads, tampons, or cups |
| Color | Light pink or brownish | Ranges from bright to dark red |
| Duration | Very brief, lasting only 1-2 days at most | Longer, typically lasting 3-7 days |
While mid-cycle spotting is usually nothing to worry about, persistent, heavy, or painful bleeding is a different story and should always be discussed with your specialist. In some cases, irregular bleeding can be an early sign of other issues, which is why it’s so important to understand the basics of infertility and know when it’s time to seek expert guidance.
The Hormonal Science Behind Mid-Cycle Spotting
To get to the bottom of why you might see a little blood around ovulation, we need to pull back the curtain on the intricate hormonal dance happening in your body. Your menstrual cycle isn’t a random event; it’s a beautifully coordinated sequence directed by a handful of key hormones, each with a very specific job to do.
Think of your brain’s pituitary gland as the conductor of a hormonal orchestra. The main players are Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), estrogen, and progesterone. Together, they create a symphony that culminates in the main event: ovulation.
This timeline shows exactly where ovulation spotting fits into the bigger picture of your cycle.
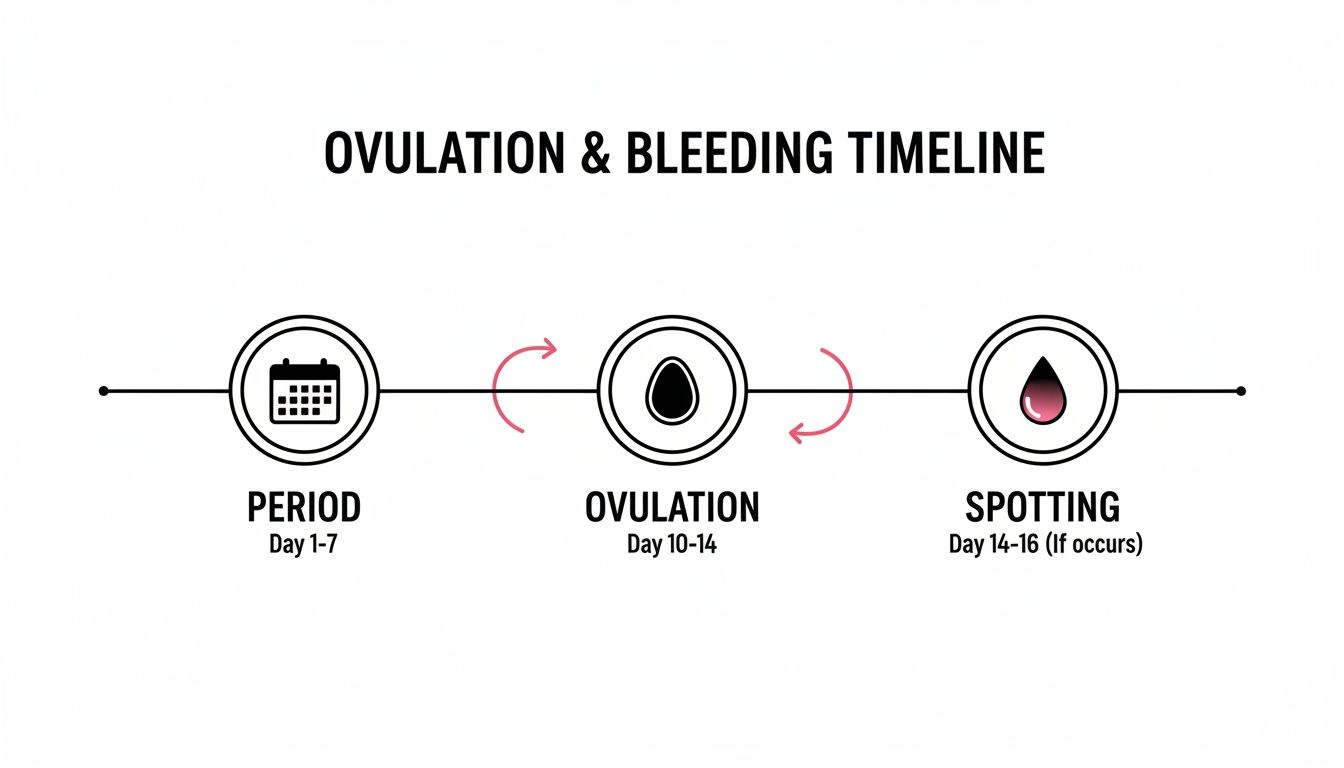
As you can see, this light bleeding happens right around ovulation—the most fertile point in your cycle—and is totally separate from your actual period.
The Role of Estrogen and the LH Surge
In the first half of your cycle, FSH gets things started by stimulating follicles in your ovaries to grow. As these follicles mature, they pump out estrogen. One of estrogen’s most important jobs is to thicken your uterine lining (the endometrium), creating a plush, welcoming environment for a potential pregnancy.
As you get closer to ovulation, your estrogen levels skyrocket, hitting a high peak. This peak is a critical signal to the pituitary gland, which responds with a massive surge of Luteinizing Hormone (LH). This LH surge is the powerful final crescendo of the hormonal orchestra—it’s the direct trigger that tells the dominant follicle to rupture and release a mature egg. That’s ovulation.
But right after this dramatic peak, there’s a planned, sharp drop in estrogen. Progesterone hasn’t had time yet to ramp up and take over as the main hormone supporting the uterine lining.
It’s in this brief hormonal gap—the rapid fall of estrogen after the LH surge and before progesterone takes over—that the endometrium can become a little unstable. This instability can cause a tiny amount of the lining to shed, resulting in the light spotting you might notice.
Why This Hormonal Shift Causes Spotting
This brief hormonal withdrawal is sometimes called estrogen breakthrough bleeding. It’s not a sign that something is wrong. Instead, it’s a direct physiological response to the rapid hormonal shift needed for ovulation to happen successfully.
Here’s a simple analogy to make sense of it: imagine you’re tending to a delicate houseplant. Estrogen is like the steady stream of water keeping the soil moist and stable. The LH surge is like a sudden, potent dose of fertilizer. Right after that dose, the water pressure (estrogen) drops for a moment before a different nutrient source (progesterone) kicks in. In that brief pause, a few grains of soil might shake loose.
This is almost exactly what happens in your uterus. The temporary dip in estrogen causes a minor shedding of the lining, which shows up as light pink or brownish spotting. The process is completely natural and, for many, serves as a physical confirmation that a strong ovulatory event has just occurred—empowering you with a medically sound understanding of your body’s unique cycle.
Other Common Reasons for Mid-Cycle Bleeding

While the hormonal ebb and flow is the usual suspect behind ovulation spotting, your body is an incredibly complex system. A number of other factors can also trigger a bit of mid-cycle bleeding, and understanding them helps build a complete picture of your health without jumping to the worst-case scenario.
One of the most talked-about reasons, especially for anyone trying to conceive, is implantation bleeding. It’s critical to understand this is a completely separate event from ovulation bleeding.
Distinguishing Implantation From Ovulation Bleeding
Implantation bleeding can happen when a fertilized egg snuggles into the uterine lining. The timing is the dead giveaway here: this event typically occurs 6 to 12 days after ovulation.
- Ovulation Spotting: This happens right around the main event—midway through your cycle when the egg is released.
- Implantation Spotting: This shows up much later in the cycle, often so close to your expected period that it’s easily mistaken for the real thing starting early.
Many women think they’re having a very light, early period when it’s actually one of the first potential signs of pregnancy. Ovulation bleeding, in contrast, is a sign that your most fertile window has just passed.
Another surprisingly simple cause of mid-cycle spotting is just increased sensitivity. The same hormonal shifts that trigger ovulation also make the cervix softer and more vascular—meaning it’s packed with more tiny blood vessels near the surface.
Because of this heightened sensitivity, friction from intercourse can sometimes cause minor, totally harmless spotting. This is often called postcoital bleeding, and when it only happens around ovulation, it’s generally nothing to worry about.
Lifestyle and Medication Influences
Never underestimate how much your daily life can affect your cycle. Your body’s hormonal symphony is incredibly sensitive to outside influences.
A period of intense life stress, starting a grueling new workout routine, or even making a major shift in your diet can disrupt the delicate conversation happening between your brain and your ovaries. That disruption can easily show up as unexpected spotting.
It’s important to remember that your reproductive system doesn’t operate in a vacuum. It is deeply interconnected with your overall physical and emotional well-being. A sudden change in your routine can sometimes manifest as a change in your cycle.
Hormonal birth control is another major player. Whether you’re starting, stopping, or just missed a pill, your body might react to the shifting hormone levels with breakthrough bleeding. This is a common and usually temporary side effect as your system adjusts.
Knowing these other potential causes gives you valuable context. While the hormonal dance of ovulation is the main driver, everything from physical sensitivity to lifestyle changes can play a role. Understanding these distinctions allows for a much more informed, and less anxious, approach to monitoring your body.
When Spotting Could Signal Something More
While a little light spotting during ovulation is usually just a harmless side effect of your natural hormonal rhythm, it’s also a signal from your body that’s worth paying attention to. The goal isn’t to worry, but to become aware. Learning to distinguish between a normal, one-off event and a pattern that might point to an underlying issue is key to taking proactive control of your health.
Think of it like your car’s check-engine light. If it flickers on for a second and then disappears, you probably write it off as a temporary glitch. But if that light stays on, starts flashing, or shows up with strange noises from the engine, you know it’s time to see a mechanic. The same logic applies here. Certain red flags can elevate mid-cycle spotting from a minor “glitch” to a symptom that warrants a conversation with a specialist.
Red Flags That Deserve a Doctor’s Attention
Not all spotting is created equal. While the cause is often completely benign, some signs are clear indicators that it’s time to dig a little deeper with your doctor. It’s really about recognizing when the bleeding deviates from the typical, faint pattern of ovulation spotting.
Get it checked out if you experience any of these:
- Heavier Than Spotting: The bleeding is heavy enough to require more than a panty liner, feeling more like a light period.
- Lasting Too Long: The bleeding continues for more than two or three consecutive days.
- Significant Pain: You’re dealing with sharp, intense, or debilitating cramps that interfere with your life—far beyond the mild twinge of ovulation pain (mittelschmerz).
- It’s a Recurring Pattern: Mid-cycle bleeding happens month after month, becoming a predictable and unwelcome part of your cycle.
- Any Postmenopausal Bleeding: This is a critical one. Any bleeding after you have fully gone through menopause demands an immediate medical evaluation.
If you’re experiencing these symptoms, the bleeding might not be connected to that simple hormonal dip of ovulation.
Potential Underlying Medical Causes
When mid-cycle bleeding is persistent, painful, or heavy, it can be a sign that a structural or systemic issue is throwing your cycle’s rhythm off course. A thorough workup with a trusted specialist is the only way to get a clear diagnosis and the right care plan.
Some of the more common conditions that can trigger abnormal bleeding include:
- Uterine Fibroids or Polyps: These are common, noncancerous growths that can develop on the uterine wall or lining and cause irregular bleeding at any time.
- Pelvic Inflammatory Disease (PID): This is an infection of the reproductive organs, often stemming from an untreated STI, which can cause inflammation and lead to abnormal bleeding.
- Cervical Issues: Benign polyps on the cervix or general cervical inflammation (cervicitis) can cause spotting, which is often noticed after intercourse.
- Thyroid Imbalances: Your thyroid is the master regulator of your metabolism and hormones. When it’s not working correctly—either overactive (hyperthyroidism) or underactive (hypothyroidism)—it can wreak havoc on your menstrual cycle and cause all sorts of irregular bleeding patterns.
Knowing about these possibilities isn’t meant to cause alarm. It’s about equipping you with the knowledge to be a better advocate for your own health. Understanding what could be causing abnormal bleeding is the first step toward getting answers, finding a solution, and protecting your long-term well-being.
How a Specialist Investigates Abnormal Bleeding
If you’ve decided it’s time to get professional answers about mid-cycle bleeding, knowing what to expect can make the whole process feel much less intimidating. A top-tier specialist won’t jump straight to invasive tests. The investigation always starts with a simple conversation.
This initial consultation is the foundation of your entire workup. Your doctor will want to know everything about your cycles, your lifestyle, and your medical history. Be prepared for questions about the timing, color, and amount of bleeding, as well as any other symptoms you’ve noticed, like pain or cramping. This detailed history is like a roadmap, guiding every step that comes next.

Common Diagnostic Tools and Tests
After your discussion and a physical exam, your doctor might suggest a few specific tests to get a clearer picture of what’s happening internally. Think of these as different tools in a toolkit, each designed for a specific job.
The most common diagnostic steps include:
- Pelvic Ultrasound: This is usually the first imaging test ordered. Using sound waves, an ultrasound creates a detailed image of your uterus, ovaries, and fallopian tubes. It’s an incredibly effective way to spot structural issues like fibroids or ovarian cysts that could be causing the bleeding.
- Blood Tests: A simple blood draw can reveal a treasure trove of information about your hormonal health. Your specialist will be looking at key hormone levels—like estrogen, progesterone, LH, and thyroid-stimulating hormone (TSH)—to see if an imbalance is disrupting your cycle.
- Hysteroscopy: If the ultrasound hints at an issue inside the uterus, your doctor might recommend this procedure. A very thin, lighted camera is gently inserted through the cervix, allowing for a direct look at the uterine lining. This makes it possible to identify and sometimes even remove small polyps or fibroids on the spot.
The goal of this diagnostic journey is clarity. A skilled specialist uses these tools not just to find a problem, but to rule out potential issues, providing you with peace of mind and a definitive path forward.
Understanding what a top-tier clinician is looking for can make you feel more prepared and empowered. For anyone seeking specialized care on their path to pregnancy, learning what a fertility specialist does can offer even more insight into the advanced diagnostics and treatments available to support your reproductive health.
Your Top Questions About Ovulation Bleeding, Answered
Let’s dive into some of the most common questions that come up around mid-cycle spotting. My goal here is to give you direct, clear answers to help you make sense of your body’s signals and feel more confident about what’s going on.
Does Bleeding During Ovulation Mean I Am More Fertile?
Not necessarily, but it’s definitely not a bad sign. Think of ovulation spotting as a side effect of the powerful hormonal surge required to release an egg. Some research suggests women who experience it have higher peak levels of key fertility hormones like LH and estrogen.
So, while it doesn’t guarantee you’ll conceive this cycle, it’s a strong indicator that a robust ovulatory event is happening. If you’re trying to get pregnant, it’s an excellent real-time signal that you’re squarely in your fertile window.
How Can I Tell Ovulation and Implantation Bleeding Apart?
Timing is everything here. It’s the single biggest clue to figuring out which type of spotting you’re seeing.
- Ovulation Spotting: This happens right around ovulation, which is typically about 14 days before your next period is due to start.
- Implantation Bleeding: This occurs much later in your cycle, usually about 6 to 12 days after ovulation. This is when a fertilized egg snuggles into the uterine lining.
Implantation bleeding is often one of the very first signs of pregnancy and shows up much closer to when you’d be expecting your period anyway.
Can Stress Cause Ovulation Bleeding?
Yes, absolutely. High levels of stress—whether from a demanding job, a big life change, or even intense travel across time zones—can scramble the delicate conversation happening between your brain and your ovaries. The same goes for sudden, significant shifts in your diet or exercise routine.
This hormonal disruption can throw your cycle off, leading to all sorts of irregular bleeding patterns, including spotting around ovulation. If you’ve been through a period of major change recently, it could very well be the culprit.
Should I See a Doctor for One Episode of Spotting?
If you have a single, isolated episode of very light pink or brown spotting that lasts only a day or two and happens mid-cycle—with no other symptoms—it’s generally not a reason to panic.
However, if it becomes a recurring theme each month, or if it comes with pain, heavy flow, or other concerning symptoms, it’s smart to schedule a visit with your doctor. And for anyone actively trying to conceive, going into that appointment prepared with the right questions to ask a fertility doctor can make all the difference in getting the clarity and answers you need.
Navigating your reproductive health requires access to trusted, top-tier specialists. Haute MD is a curated medical network that connects discerning patients with the nation’s leading, rigorously vetted physicians in fertility, hormone optimization, and more. Find the expert care you deserve.

