Feeling tired after a meal when you have diabetes is more than just a minor inconvenience—it’s a direct signal from your body that your blood sugar is on a rollercoaster. This profound fatigue, known as postprandial fatigue, is almost always driven by a sharp spike in blood sugar (hyperglycemia) or the rapid crash that follows (reactive hypoglycemia). Getting this energy drain under control is the key to reclaiming your day.
Understanding the Post-Meal Energy Crash
That overwhelming wave of exhaustion that hits you after a meal isn’t just in your head. It’s a frustrating and common reality for many living with diabetes, and it’s a powerful metabolic clue your body is sending. While a big holiday dinner can make anyone feel a bit sleepy, the experience of diabetes fatigue after eating is distinctly more intense.
Think of your body’s energy system as a finely tuned high-performance engine. For it to run smoothly, it needs a steady, controlled supply of fuel—glucose. When blood sugar swings wildly after a meal, it’s like flooding that engine with a volatile, unregulated fuel mixture. The result? The engine sputters, stalls, and leaves you feeling completely drained.
More Than Just “Food Coma”
It’s crucial to distinguish this debilitating fatigue from the typical drowsiness one might feel after a large meal. The fatigue associated with diabetes is often severe and comes with other tell-tale signs of metabolic distress.
You might also experience:
- Brain fog: A frustrating mental cloudiness that makes it impossible to concentrate or think clearly.
- Irritability: Sudden mood swings or impatience that seem to appear from nowhere.
- Intense cravings: A powerful urge for more sugary or high-carb foods, which only perpetuates the vicious cycle.
This isn’t a sign of weakness or a simple need for a nap. It’s a clear message that your body is struggling to manage the glucose from your last meal.
Your post-meal fatigue is not a personal failing; it is a physiological response. Framing it as a crucial metabolic signal is the first step toward effectively managing it and reclaiming your energy.
Understanding this dynamic is essential. Once you recognize that post-meal fatigue is a direct result of blood sugar instability, you can start to pinpoint the specific cause. Whether it’s a “sugar traffic jam” from hyperglycemia or an “insulin overreaction” triggering a crash, identifying the pattern is the first step toward a solution.
This guide will help you decode those signals. We’ll explore the hidden culprits behind your energy crashes and outline sophisticated, practical strategies to help you take back control. By understanding the science, you can shift from feeling powerless against fatigue to proactively managing your energy, one meal at a time. The goal is to transform diabetes management from a reactive chore into a powerful tool for a more vibrant, energized life.
The Hidden Causes of Your Post-Meal Fatigue
To solve the puzzle of your post-meal energy drain, we need to look at the intricate metabolic drama unfolding inside your body. That feeling of diabetes fatigue after eating isn’t a single problem but a symptom pointing to several potential imbalances. Each one disrupts your body’s ability to convert food into fuel, leaving you depleted right when you should feel energized.
Getting to the bottom of these triggers is the first step toward reclaiming your vitality. Let’s break down the most common culprits.
Hyperglycemia: The Sugar Traffic Jam
More often than not, the prime suspect behind post-meal fatigue is hyperglycemia, or high blood sugar. Think of your bloodstream as a highway and glucose molecules as cars trying to deliver fuel to their destinations—your body’s cells. Insulin is the traffic controller, opening the gates to the cells so the glucose can get inside.
With diabetes, you either don’t have enough insulin or your cells ignore its signals. This creates a massive “sugar traffic jam.” Glucose piles up in your bloodstream, unable to enter the cells.
Even though you’ve just eaten and have plenty of fuel available, your cells are effectively starving. They send powerful fatigue signals to your brain, creating a profound energy crisis that leaves you feeling completely drained.
Reactive Hypoglycemia: The Insulin Overreaction
On the flip side of the coin is reactive hypoglycemia, a phenomenon where your blood sugar plummets after an initial spike. This often happens after a meal loaded with simple carbohydrates or sugars. Your body senses the rapid flood of glucose, panics, and unleashes a massive surge of insulin to handle it.
Sometimes, this response is just too aggressive. The flood of insulin works overtime, clearing not just the excess glucose but driving your blood sugar levels well below normal. This is the “crash” that follows the “high,” leading to intense fatigue, shakiness, and brain fog a few hours after your meal. It’s a classic overcorrection that empties your energy tank.
This concept map shows how both high and low blood sugar scenarios—the traffic jam and the overcorrection—ultimately lead to the same exhausting outcome.
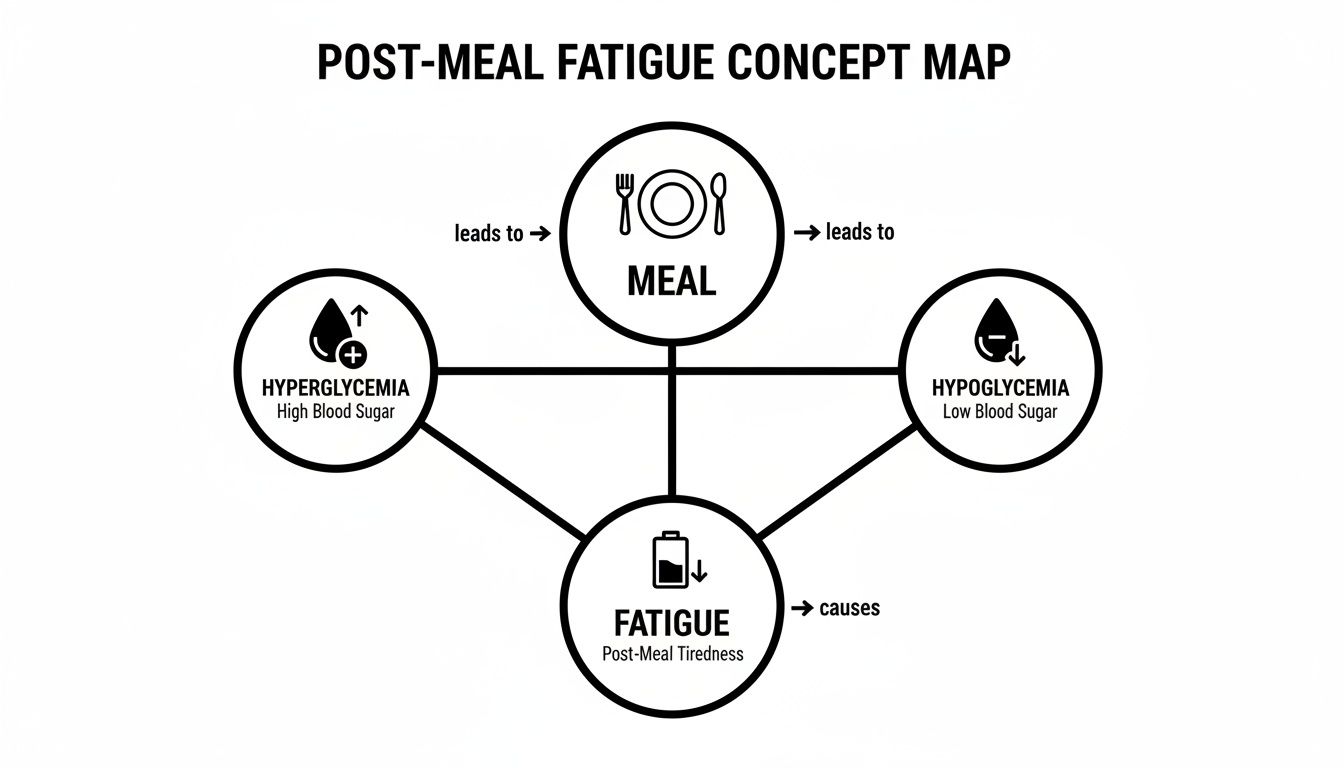
As you can see, managing post-meal energy isn’t just about avoiding high sugar. It’s about maintaining stability to prevent the exhausting crashes that follow.
Beyond Blood Sugar: Other Key Factors
While glucose fluctuations are the main event, several other factors can compound the problem, making your energy management even more complex.
Here’s a quick look at the primary drivers of post-meal fatigue and what they feel like.
Common Causes of Fatigue After Eating with Diabetes
| Cause | Mechanism | Typical Experience |
|---|---|---|
| Hyperglycemia | Cells are “starved” of energy as glucose remains trapped in the bloodstream. | A heavy, sluggish feeling that sets in within 1-2 hours of eating. Often described as brain fog or lethargy. |
| Reactive Hypoglycemia | An excessive insulin release causes a rapid drop in blood sugar after an initial spike. | A sudden “crash” 2-5 hours after a meal, accompanied by shakiness, anxiety, sweating, and intense fatigue. |
| Medication Mismatch | Insulin or oral medication timing doesn’t align with meal digestion and glucose absorption. | Unpredictable energy levels, with fatigue appearing at inconsistent times after eating. |
| Gastroparesis | Delayed stomach emptying creates a disconnect between food intake and nutrient availability. | Feeling overly full long after a meal, combined with bloating and a slow, creeping fatigue. |
Each of these factors requires a different strategic approach, highlighting why a one-size-fits-all solution rarely works.
- Medication Effects: The very tools used to manage diabetes can sometimes contribute to fatigue. Certain oral medications can impact energy, and insulin therapy demands precise timing. Fatigue is a huge issue, affecting up to 50% of patients with diabetes. Research shows that for those starting insulin, fatigue can worsen with higher doses, partly due to the risk of hypoglycemia and the mental load of management. You can find more details about the connection in this detailed study.
- Gastroparesis: This complication involves delayed stomach emptying. When food sits in your stomach too long, nutrient absorption becomes slow and unpredictable. This throws off the delicate timing between your insulin dose and glucose release, leading to blood sugar volatility and fatigue.
- Macronutrient Composition: What you eat matters just as much as when. A meal heavy on refined carbs without enough protein, fiber, and healthy fats is a recipe for a rapid blood sugar spike and the inevitable crash. These other nutrients act as a brake, slowing down digestion and promoting a more gradual, stable release of glucose into your bloodstream.
By understanding these interconnected causes—from cellular energy deficits to the simple mechanics of digestion—you and your physician can begin to build a precise, personalized plan to conquer your post-meal fatigue and restore your vitality.
How to Pinpoint Your Personal Fatigue Triggers
Guesswork has no place in managing your health. To get a real handle on the diabetes fatigue after eating, you have to stop making assumptions and start acting like a detective, uncovering the specific patterns of your own metabolism. Pinpointing what’s really causing your energy to crash requires a systematic approach that combines your personal observations with hard medical data.
This whole process is about gathering the right intelligence. By meticulously connecting what you eat with how you feel, both you and your physician can build a clear, actionable picture. This is how you create a plan that genuinely restores your vitality instead of just patching over symptoms.

Start with a Symptom and Food Journal
The first and most fundamental step is to keep a detailed log. It might sound old-school, but a well-maintained journal is an incredibly powerful tool for revealing the direct cause-and-effect relationships between your meals and your energy. For just a few weeks, be diligent about recording everything.
Make sure your journal tracks a few key data points for every single meal:
- What You Ate: Get specific. Note the exact foods, ingredients, and portion sizes.
- Time of Meal: Log the precise time you started and finished eating.
- Fatigue Level: Using a simple 1-10 scale, rate your energy one and three hours after eating.
- Other Symptoms: Make a note of any brain fog, irritability, shakiness, or sudden cravings.
After a couple of weeks, you’ll start to see patterns emerge that were previously invisible. You might find that a “healthy” fruit smoothie consistently triggers a mid-afternoon crash, or that adding a specific protein to your lunch keeps you sharp and focused. This is the first layer of data you need.
Leverage Continuous Glucose Monitoring
While your journal helps you see what is happening, a Continuous Glucose Monitor (CGM) shows you precisely why it’s happening, in real-time. For anyone serious about optimizing their metabolic health, this technology is an absolute game-changer. A CGM uses a tiny sensor just under the skin to stream a minute-by-minute view of your glucose levels directly to your smartphone.
Instead of relying on random, infrequent fingerpricks, a CGM paints the entire picture of your glucose curve. You see the immediate and delayed impact of every meal, every snack, and every bit of activity.
A CGM shifts metabolic management from being reactive to proactive. It provides the objective, hard data needed to truly understand your unique physiology, allowing you to anticipate and head off energy crashes before they even start.
With a CGM, you can directly correlate that feeling of exhaustion with a specific event—a rapid glucose spike, a steep drop into hypoglycemia, or a long, drawn-out period of high blood sugar. This level of insight is simply impossible with traditional monitoring, giving your doctor the granular data needed to fine-tune your treatment with incredible precision.
The Bigger Picture with Key Lab Tests
Finally, to complete your metabolic profile, your physician will order a few essential lab tests. These diagnostics provide a high-level view of your long-term glucose control and underlying insulin dynamics, giving critical context to the real-time data from your CGM. For those who want to dig deeper into their body’s efficiency, learning about how metabolic testing for weight loss is a practical guide can offer valuable additional insights.
Key tests almost always include:
- Hemoglobin A1C (HbA1c): This is a snapshot of your average blood sugar levels over the past three months, offering a crucial benchmark for your overall glucose management.
- Fasting Insulin and Glucose: Measuring these together allows for the calculation of insulin resistance, revealing how hard your body is working to keep your blood sugar in check.
- C-Peptide Test: This test measures how much insulin your own pancreas is still producing, which is critical for distinguishing between different types of diabetes and guiding medication strategy.
By combining the subjective insights from your journal, the real-time data from a CGM, and the long-term context from lab work, you and your medical team can build a truly comprehensive and accurate understanding of your personal fatigue triggers. This data-driven strategy is the foundation for conquering post-meal fatigue and reclaiming sustained, all-day energy.
Practical Strategies for Sustained All-Day Energy
Understanding why you’re tired after eating is the first step. Turning that insight into action is how you reclaim your day. This isn’t about reactive fixes or restrictive diets. It’s about a strategic, data-driven approach to food, medication, and lifestyle that creates metabolic stability and delivers unwavering energy from morning to night.
The fundamental goal is to prevent the dramatic blood sugar fluctuations that trigger diabetes fatigue after eating. By engineering your meals and habits to create a gentle, rolling glucose curve—instead of sharp peaks and freefalls—you can completely transform how you feel.
Architecting Your Meals for Stable Energy
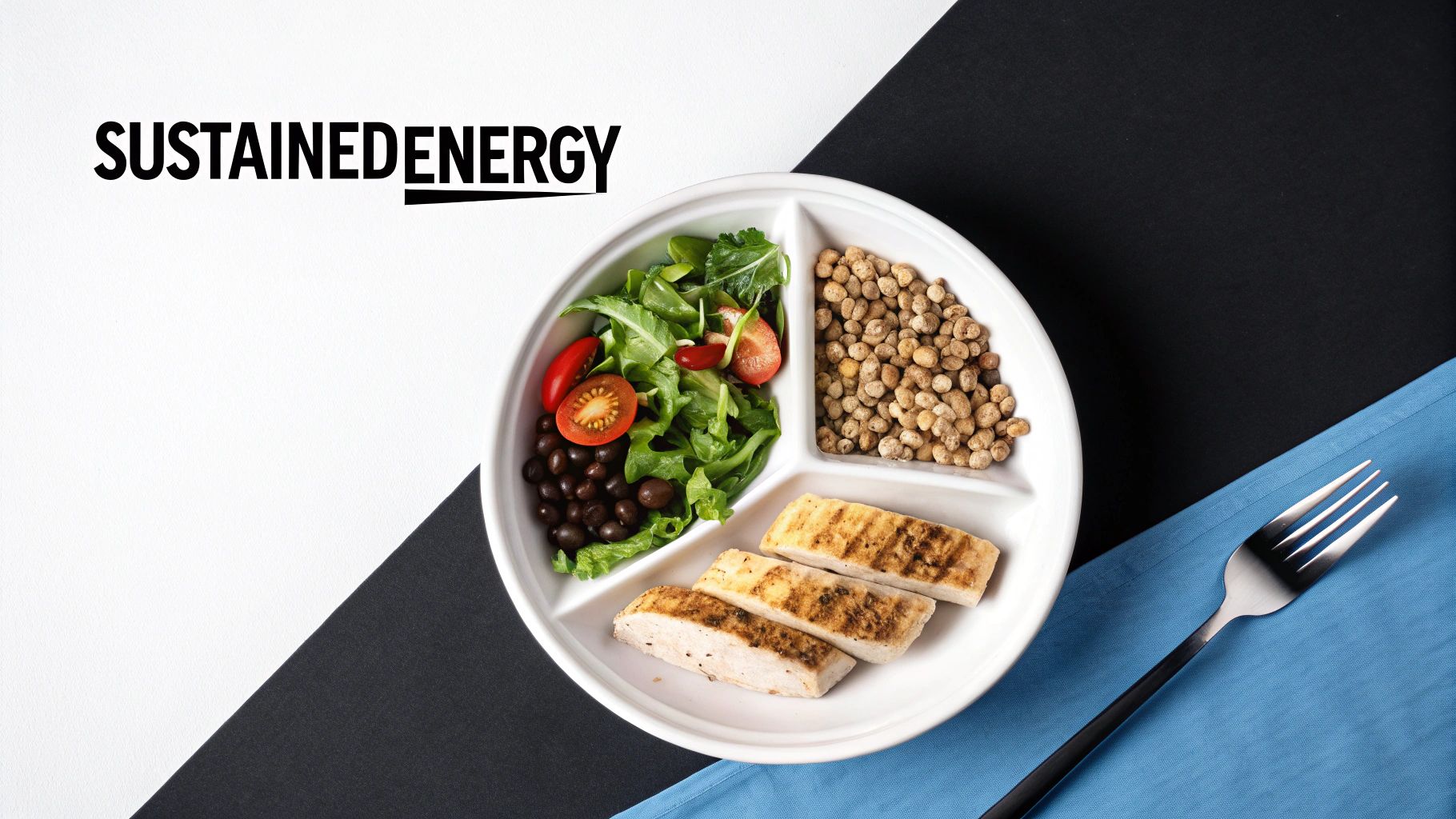
Think of your plate as a blueprint for your energy levels. The specific combination of foods you eat directly controls the speed and intensity of your body’s glucose response. The objective is to slow down digestion and absorption, ensuring a steady, measured release of fuel into your bloodstream.
You can achieve this by focusing on three core elements:
- Embrace Low-Glycemic Foods: The glycemic index (GI) is a simple measure of how quickly a food spikes your blood sugar. High-GI foods like white bread or sugary drinks act like kindling—they burn hot and fast, causing a rapid energy surge followed by an inevitable crash. In contrast, low-GI foods like non-starchy vegetables, legumes, and whole grains are like slow-burning logs, providing a gradual, sustained release of energy.
- Master Macronutrient Pairing: A carbohydrate should never go to a party alone. Pairing carbs with protein, healthy fats, and fiber is the single most effective way to put the brakes on glucose absorption. For instance, instead of eating an apple by itself, have it with a handful of almonds. The protein, fat, and fiber in the nuts will dramatically blunt the glucose spike and keep you feeling full longer, preventing the fatigue that so often follows a carb-only snack.
- Strategic Meal Timing and Portions: Consistency is everything. Eating balanced meals at regular intervals helps your body maintain stable blood sugar and prevents the kind of ravenous hunger that leads to poor choices. It’s also important to recognize that very large meals can simply overwhelm your system. Many of my clients find that smaller, more frequent meals provide a more manageable glucose load for their body to process.
Fine-Tuning Medication with Precision
While nutrition is the foundation, your medication regimen is a powerful tool for smoothing out that glucose curve. If you’re still experiencing post-meal slumps despite making smart food choices, it’s a clear signal that your medication may need a tune-up. This is always a collaborative process guided by your physician.
Even small, precise adjustments can make a world of difference. Your doctor might suggest:
- Adjusting Insulin Timing: Shifting the timing of your pre-meal insulin bolus by just 15 minutes can better synchronize its peak action with your food’s glucose absorption, effectively heading off a post-meal spike.
- Exploring Different Formulations: A simple switch from a rapid-acting to an ultra-rapid-acting insulin (or vice versa) could provide a much better match for your unique metabolic response to certain meals.
- Reviewing Oral Medications: Certain oral agents are far more effective than others at controlling post-meal glucose excursions. A review could reveal a more optimal choice for your needs.
Proactive Management with Your CGM Data
A Continuous Glucose Monitor (CGM) is more than just a diagnostic tool—it’s your personal energy dashboard. The key is to use its real-time data to anticipate and prevent energy dips, not just react to them. If you see a familiar pattern of rising glucose after a certain meal, you can intervene before fatigue ever sets in. A brisk 15-minute walk right after eating, for example, forces your muscles to start pulling glucose from the bloodstream, effectively blunting the spike.
This proactive approach is critical, especially when you consider how widespread this problem is. Research shows that fatigue prevalence in patients with diabetes can be as high as 50%, with these post-meal dips being a major culprit. One study documented a telling case where a young adult’s extreme drowsiness directly corresponded with a glucose peak of 224 mg/dL—a symptom that vanished once treatment was adjusted to lower his glucose and insulin levels.
By integrating these strategies, you shift from simply managing a condition to actively optimizing your performance. For a broader look at improving your body’s efficiency, explore our practical guide on how to improve metabolic health. It’s all about building a system that supports consistent, all-day energy, so you can focus on what truly matters.
When to Escalate: Moving Beyond Lifestyle Tweaks
While smart diet and lifestyle changes can manage a lot of the fatigue that follows a meal, there are times when your body sends signals that demand a physician’s attention. Self-management is a powerful tool, but it has its limits. Knowing when to bring in your doctor isn’t a sign of failure—it’s a strategic move to protect your long-term health and performance.
Think of it like this: you’re the CEO of your own health, making daily operational decisions. Your physician is the specialist consultant you bring in for the high-stakes challenges that require deep expertise. You wouldn’t guess on a critical business decision, and you shouldn’t guess when your health is on the line.
Recognizing Red Flag Symptoms
Some symptoms are more than just post-meal sluggishness. They are non-negotiable reasons to schedule a consultation. If the fatigue is so severe that it consistently torpedoes your work, disrupts family life, or makes daily responsibilities feel impossible, it’s time to act. It’s one thing to feel a little tired; it’s another entirely to be unable to function.
Keep a sharp eye out for these specific warning signs:
- Severe or Disruptive Fatigue: The exhaustion is so profound it stops you from performing routine tasks, from leading a meeting to driving safely.
- Cognitive Impairment: Your fatigue is paired with significant dizziness, confusion, or a persistent brain fog that feels genuinely unsafe.
- Unpredictable Blood Sugar Swings: Despite your best efforts with diet and medication, your glucose numbers are all over the map.
- Symptoms of Hypoglycemia: You’re frequently experiencing shakiness, sweating, anxiety, or heart palpitations after you eat.
When your symptoms start to actively limit your life or feel out of your control, this is no longer about simple lifestyle adjustments. It’s a clear signal from your body that a deeper medical evaluation is needed to find the root cause and recalibrate your treatment plan.
When Gastroparesis Might Be the Culprit
Sometimes, fatigue is just one piece of a bigger puzzle involving your digestive system. If your post-meal exhaustion consistently arrives with a side of gastrointestinal distress, you could be dealing with gastroparesis—a condition where the stomach empties too slowly. It’s a common but frequently overlooked complication of diabetes.
Be vigilant for this cluster of symptoms, especially if they show up together after eating:
- Persistent bloating or feeling uncomfortably full after even small meals
- Nausea or even vomiting hours after you’ve finished eating
- Heartburn or acid reflux that won’t quit
- A poor appetite and unintended weight loss
These signs require a formal diagnosis from your doctor, who might order tests like a gastric emptying study. Trying to manage these issues on your own is often ineffective and can delay the right treatment.
Partnering with the Right Medical Expert
Navigating these complex symptoms demands a strong partnership with a sharp, attentive physician. Your doctor’s job is to connect the dots between your symptoms and your data, creating a precise and effective strategy. If you feel your concerns are being brushed aside or you’re seeking a higher caliber of specialized care, it might be time to find a better fit.
For those who demand a premium, outcome-focused approach to their health, understanding how to find the best doctor is the first step in building an elite medical team. This isn’t just about managing symptoms—it’s about partnering with an expert who can help you optimize your health and get your energy back.
You Don’t Have to Settle for Post-Meal Fatigue
Feeling drained after every meal doesn’t have to be your new normal. If you’ve been on this journey with us, you now understand that post-meal fatigue is a solvable problem—a clear, actionable signal from your body that’s demanding a more strategic approach. It’s a sign of metabolic inefficiency, not a permanent sentence.
We’ve pulled back the curtain on the core causes, from the cellular “traffic jams” of hyperglycemia that literally starve your cells of energy to the jarring, hypoglycemic crash-and-burn cycles. These aren’t random events. They are predictable, mechanical responses to the interplay between your food choices, medication timing, and your unique physiology.
The Path to Metabolic Mastery
The real takeaway here is empowerment. You can now move beyond merely coping with the symptoms of diabetes fatigue after eating and begin mastering the underlying mechanics of your metabolism.
- Pinpoint Your Triggers: Forget guesswork. Tools like a symptom journal are a start, but a Continuous Glucose Monitor (CGM) is the game-changer. It provides the hard data you need to connect your actions—that specific meal, that workout, that stressful meeting—to their direct metabolic consequences.
- Implement Smarter Strategies: By focusing on meal architecture—pairing every carbohydrate with quality protein and fiber—and fine-tuning your medication timing, you can flatten those energy-sapping blood sugar curves.
- Take Proactive Control: A brisk 15-minute walk after lunch or a subtle adjustment in insulin timing can be the difference between an afternoon slump and sustained, focused energy.
This is about fundamentally shifting from a reactive posture to a proactive one. Your body is giving you constant feedback. With the right tools and knowledge, you can finally interpret those signals and make intelligent, real-time adjustments.
The goal is to graduate from managing a condition to optimizing your personal performance. By applying these principles, you are taking direct control of your metabolic health to reclaim the consistent, stable energy you deserve.
The fatigue that once felt inevitable can become a relic of the past. Mastering your metabolism means you are no longer at the mercy of volatile blood sugar swings. Instead, you become the architect of your own energy, building a foundation for a more vibrant, productive, and resilient life.
Frequently Asked Questions
When you’re dealing with post-meal fatigue, a lot of specific questions come up. Getting to the bottom of why you feel drained is the first step toward taking control. Here are some straightforward answers to the most common questions about the link between diabetes fatigue after eating, your diet, and how your body is responding.
Think of this as your starting point for a more productive conversation with your doctor, arming you with the insights needed to reclaim your energy.
Can the Type of Carbohydrate I Eat Affect My Fatigue?
Absolutely. The kind of carbs you choose is one of the biggest levers you can pull to manage your post-meal energy.
High-glycemic carbs—think white bread, pastries, and sugary drinks—are digested almost instantly. This sends your blood sugar on a steep climb, which is almost always followed by an energy-sapping crash.
On the other hand, complex, high-fiber carbohydrates from sources like vegetables, legumes, and whole grains are broken down slowly. This leads to a much more gradual, stable release of glucose into your bloodstream. The result is sustained energy, not the extreme peaks and valleys that leave you feeling exhausted.
A core strategy for steady energy is to never eat a carbohydrate alone. Always pair it with a quality protein and a healthy fat. This combination acts like a brake on digestion, slowing down glucose absorption and preventing that metabolic rollercoaster.
How Soon After Eating Does Diabetes Fatigue Usually Start?
The timing of your fatigue is a critical clue. It can help you and your physician pinpoint the root cause because the window in which exhaustion hits often correlates directly with what your blood sugar is doing.
Here’s a general timeline:
- Hyperglycemia Fatigue (High Blood Sugar): If the fatigue is from high blood sugar, it typically kicks in 1 to 2 hours after a meal. This is the point when glucose from your food floods the bloodstream.
- Reactive Hypoglycemia Fatigue (Blood Sugar Crash): If a blood sugar crash is the real culprit, the fatigue may show up later, often 2 to 4 hours after you eat. This happens when an overzealous insulin response has pushed your glucose levels too low.
A Continuous Glucose Monitor (CGM) is the single best tool for this kind of detective work. It lets you match your feelings of fatigue to your real-time glucose data, revealing your unique pattern with precision.
Is It Normal to Feel Tired After Eating Without Diabetes?
Yes, it can be. A mild drowsiness after a very large meal—sometimes called postprandial somnolence or a “food coma”—is fairly common. It happens as your body diverts blood flow and energy to the massive task of digestion.
However, the diabetes fatigue after eating is a completely different beast. It’s typically far more intense and debilitating. It feels less like simple sleepiness and more like someone pulled your emergency power cord.
This profound exhaustion is a direct signal that your body is struggling to manage blood sugar efficiently. While someone without diabetes might feel a bit groggy, a person with diabetes can experience an overwhelming wave of fatigue that makes it impossible to concentrate or function. That significant difference in intensity is a clear sign that better glucose control is needed to get your vitality back.
When standard care isn’t enough to solve persistent fatigue, you need an elite physician who specializes in metabolic optimization. Haute MD offers direct access to a curated network of the nation’s top doctors, ensuring you receive the sophisticated, outcome-driven care you deserve. Find a specialist through Haute MD who can help you master your metabolism and reclaim your performance.

