That burning sensation in your chest after dinner has you wondering, “Is this acid reflux?” It’s a common question. While a one-off bout of heartburn is something most of us have felt, frequent symptoms can signal a more chronic issue known as Gastroesophageal Reflux Disease (GORD).
Getting to the bottom of that discomfort starts with understanding what’s really going on inside.
Unpacking That Burning Sensation

Acid reflux is what happens when stomach acid makes a wrong turn, flowing back up into your esophagus—the tube that connects your throat to your stomach. Think of the valve at the bottom of your esophagus, the lower esophageal sphincter (LES), as a tightly sealed gate. Its job is to swing open for food and then slam shut to keep stomach contents where they belong.
Imagine it like a high-quality lid on a blender. When it’s on tight, you can blend anything without a mess. But if that lid is loose or doesn’t seal properly, the contents can splash right back up. That’s exactly what’s happening during reflux. The LES muscle gets weak or relaxes at the wrong time, letting harsh stomach acid escape and irritate the sensitive lining of your esophagus.
This acidic backwash creates that classic burning feeling we call heartburn. Having it once after a huge holiday meal or a particularly spicy dish is normal. But when it becomes a regular unwelcome guest, it’s a different story.
How Common Is Acid Reflux?
If this sounds familiar, you’re in good company. Acid reflux is a massive global issue. Worldwide, about 1 in 7 adults deal with symptoms that point to GORD. The problem is even more widespread in North America, where the prevalence hits 19.1%—which explains why so many people complain about weekly heartburn. You can learn more about the global impact of GORD and its risk factors from recent medical analyses.
To figure out if what you’re experiencing is just a nuisance or a potential medical issue, it helps to compare the symptoms side-by-side.
Quick Symptom Checker: Occasional Heartburn vs. Potential GORD
This table helps distinguish between a common, isolated incident and a pattern that might suggest a chronic condition like GORD.
| Symptom Aspect | Occasional Heartburn | Potential Acid Reflux (GORD) |
|---|---|---|
| Frequency | Infrequent, maybe once a month or less. | Two or more times per week. |
| Triggers | Clearly linked to a specific large or spicy meal. | Happens with various foods or even on an empty stomach. |
| Duration | Lasts a short time and resolves on its own or with an antacid. | Can last for hours and may not respond well to antacids. |
| Severity | Mild to moderate burning discomfort. | Can be severe, disrupting sleep and daily activities. |
| Other Symptoms | Usually just chest discomfort. | May include regurgitation, chronic cough, hoarseness, or asthma. |
Seeing your symptoms in the “Potential GORD” column is a strong sign that it’s time to dig deeper.
The key distinction lies in frequency and severity. A single episode of heartburn is an event; recurring acid reflux is a condition that requires attention.
Understanding this difference is the crucial first step. It shifts the question from “Do I have acid reflux?” to identifying a clear pattern that can lead to a proper diagnosis and, ultimately, effective management.
Decoding Your Symptoms: From Classic Heartburn to Silent Signs

When you ask yourself, “Do I have acid reflux?”, your mind probably jumps straight to one thing: heartburn. That familiar burning in your chest is the classic calling card, but it’s just one piece of a surprisingly complex puzzle. The truth is, acid reflux can show up in ways that seem completely disconnected from your digestive system.
Think of it like this: the symptoms of reflux fall into two buckets. You have the classic, well-known signs, and then you have the “silent” or atypical ones that are much harder to pin down. Knowing how to spot both is the key to connecting the dots between how you feel and what’s really going on inside.
The Classic Red Flags of Acid Reflux
These are the symptoms everyone associates with reflux, and for good reason. They happen when stomach acid washes back up and directly irritates the lining of your esophagus, creating sensations that are hard to ignore. If these sound familiar, especially after a meal or when you lie down, acid reflux should be high on your list of suspects.
The usual suspects include:
- Heartburn: This is more than just a little indigestion. We’re talking about a distinct burning pain that starts behind your breastbone and can climb up toward your throat. It has a knack for getting worse right after you eat, bend over, or lie flat.
- Regurgitation: This is that awful sensation of stomach contents—acid and sometimes bits of undigested food—backing up into your throat or mouth. It can leave behind a sour, bitter taste and is a tell-tale sign that the valve at the bottom of your esophagus isn’t doing its job.
- Dysphagia: This is the medical term for feeling like food is getting stuck in your throat or chest. When acid repeatedly damages the esophagus, the inflammation can cause the passage to narrow, making it tough for food to go down smoothly.
If you’re dealing with this trio more than twice a week, you’re likely past the point of occasional indigestion and into the territory of a chronic condition.
Uncovering the Silent or Atypical Symptoms
This is where things get tricky. Atypical symptoms pop up when refluxed stomach acid travels beyond the esophagus, hitting the throat, airways, and even your mouth. Since they don’t cause that trademark chest burn, most people never make the connection to a digestive problem, sometimes for years.
It’s no surprise that many people with chronic reflux end up at an ear, nose, and throat (ENT) specialist or a lung doctor first. They go in complaining about a nagging cough or sore throat, never suspecting the real problem is starting in their stomach.
Keep an eye out for these less-obvious clues:
- Chronic Dry Cough: A nagging cough that just won’t quit—and isn’t from a cold or allergies—is a huge red flag. Tiny droplets of acid can irritate the nerve endings in your throat and lungs, triggering a constant cough reflex.
- Morning Hoarseness: If you wake up with a raspy voice that gets better as the day goes on, it could be a sign that acid is splashing up onto your voice box (the larynx) while you sleep.
- Globus Sensation: This is that maddening, persistent feeling of a lump in your throat. It’s not actually there, but the muscles in your throat tighten up in response to acid irritation, creating the sensation.
- Sore Throat: A recurring sore throat without any other cold symptoms can be caused by acid damaging the delicate tissues in the back of your throat.
- Dental Erosion: Sometimes your dentist is the first one to spot reflux. Over time, stomach acid can eat away at tooth enamel, especially on your back molars, leading to cavities and sensitivity.
Imagine someone who’s had a dry cough for six months. They’ve tried allergy pills and inhalers, but nothing helps. The real culprit could easily be silent reflux happening at night, irritating their airways without ever causing a single moment of heartburn. This scenario is incredibly common, and it’s exactly why understanding the full spectrum of symptoms is so critical.
Understanding What Else It Could Be
Just because you’re dealing with chest discomfort or an upset stomach doesn’t automatically mean it’s acid reflux. A lot of different conditions can masquerade with similar symptoms, and figuring out what’s really going on is the critical first step toward getting the right help. This isn’t about playing doctor at home, but about becoming an informed partner in your own healthcare.
When you’re asking, “Do I have acid reflux?”, it’s just as important to ask, “Could it be something else?” Let’s walk through some of the most common conditions that can mimic reflux, starting with the one you absolutely can’t ignore.
The Critical Distinction: Heart-Related Chest Pain
Any new or severe chest pain demands immediate attention because it could be a signal from your heart. While the heartburn from reflux is a burning feeling, the pain from a heart attack is more often described as a squeezing, pressure, or tightness in the chest. This is a vital distinction to understand.
Key differences to keep in mind:
- Pain Character: Heartburn usually feels like a sharp, burning sensation right behind your breastbone. Cardiac pain often feels like immense pressure, as if a heavy weight is sitting on your chest.
- Pain Radiation: Heart-related pain has a notorious habit of traveling, often radiating to the left arm, jaw, neck, or back. Heartburn pain, on the other hand, typically stays put in the chest and throat.
- Accompanying Symptoms: Heart attacks often bring friends to the party—shortness of breath, cold sweats, dizziness, and nausea are common. While reflux can certainly cause nausea, the other symptoms are far less likely.
If your chest pain is severe, sudden, or comes with any of these other signs, do not wait. Call 911 immediately. It’s always better to be safe than sorry when your heart is involved.
Beyond the Heart: Other Potential Culprits
Once you’ve ruled out an immediate cardiac emergency, several other digestive conditions can be mistaken for GORD. Getting familiar with their unique signatures can help you and your doctor narrow down the possibilities.
Peptic Ulcers
A peptic ulcer is an open sore on the lining of your stomach or the first part of your small intestine. Like reflux, it can cause a burning stomach pain. The tell-tale difference, however, is often in the timing. Ulcer pain frequently gets worse on an empty stomach and might even feel a bit better right after you eat, since food can temporarily buffer the stomach acid.
Functional Dyspepsia
This is a fancy term for chronic indigestion without an obvious cause, sometimes called non-ulcer dyspepsia. The symptoms include upper abdominal pain, bloating, and that frustrating feeling of being full after just a few bites. While there’s some overlap with GORD, the main event here is usually fullness and bloating rather than the classic fiery burn of heartburn.
Eosinophilic Esophagitis (EoE)
EoE is an immune-driven condition where a type of white blood cell, the eosinophil, decides to set up camp in your esophagus, causing inflammation. This can trigger symptoms that feel almost identical to GORD, including heartburn and chest pain. The big clue for EoE, however, is often significant difficulty swallowing (dysphagia), especially with solid foods that feel like they’re getting stuck. For individuals looking to understand more about conditions involving the immune system, a top-rated allergy and immunology specialist can offer deeper insights.
Recognizing these distinctions makes it clear why a professional diagnosis is so essential. While many signs might point toward acid reflux, your doctor can run the right tests to confirm what’s causing your discomfort and rule out these other conditions. This ensures you get the most effective treatment for whatever is really going on.
Your At-Home Symptom Assessment Plan
Before you even think about scheduling a doctor’s visit, there are a few practical steps you can take at home to get a much clearer picture of what your body is trying to tell you. This isn’t about self-diagnosing; it’s about gathering intelligence. By becoming a detective in your own health story, you can collect specific details that make your eventual conversation with a physician vastly more productive.
The most powerful tool for this is a simple symptom diary. Don’t overthink it—a small notebook or the notes app on your phone is perfect. The goal is to start connecting the dots between your symptoms, your diet, and your daily activities to pinpoint your personal triggers.
Keeping Your Symptom Diary
Commit to this for a week or two. Jotting down a few key details each day can reveal surprisingly powerful connections, helping you move from a vague suspicion to a data-backed answer to the question, “Do I have acid reflux?”
- When do symptoms occur? Note the exact time of day. Is it like clockwork after your morning coffee, in the middle of the night, or during a stressful afternoon meeting?
- What did you eat or drink? Specifics are everything. Instead of “lunch,” write down “spicy chicken sandwich, fries, and a cola.” This is how you find the culprits.
- How severe is the discomfort? Use a simple 1-10 scale. This helps track whether a symptom is just a minor annoyance or a major disruption to your day.
- What were you doing? Were you lying on the couch, out for a run, or hunched over your desk? Your posture and activity level play a huge role.
Running a Short Lifestyle Trial
While you’re keeping the diary, you can run a few small, evidence-based experiments to see if they move the needle. Think of it as gently testing your body’s response to a few common-sense adjustments.
Consider trying one or two of these changes:
- Elevate Your Head at Night: Use a wedge pillow or put blocks under the head of your bed to raise it by six to eight inches. Gravity can be your best friend in keeping stomach acid where it belongs.
- Avoid Late-Night Meals: Make a rule to stop eating at least three hours before you lie down for bed. This gives your stomach time to empty, dramatically reducing the risk of nighttime reflux.
- Mind Your Portions: Instead of three large meals, try eating smaller, more frequent ones. This reduces the pressure on your lower esophageal sphincter, that crucial valve between your stomach and esophagus.
These at-home steps aren’t a substitute for a real medical diagnosis, but they arm you with powerful information. When you see your doctor, you’ll be able to say, “My heartburn hits an 8/10 every time I have coffee after 3 p.m.,” instead of just, “I get heartburn sometimes.”
That level of detail is a game-changer for your doctor. But it’s just as important to know when a symptom isn’t just a pattern—it’s a red flag.
Knowing the Red Flag Symptoms
While most reflux symptoms are manageable, certain signs can point to a more serious problem that needs immediate medical attention. If you experience any of the following, don’t wait to see if they get better. Call your doctor right away.
- Unintended Weight Loss: If you’re losing weight without trying, your body is sending a signal that something else is going on.
- Severe Difficulty Swallowing (Dysphagia): A persistent feeling that food is getting stuck in your throat or chest is a major warning sign.
- Vomiting Blood or Material that Looks Like Coffee Grounds: This is a classic indicator of bleeding in your upper GI tract and requires urgent evaluation.
- Black, Tarry Stools: This is another potential sign of internal bleeding.
- Persistent Chest Pain: As we’ve covered, any chest pain needs to be taken seriously until a cardiac cause is ruled out.
This decision tree helps visualize that critical choice between calling 911 and scheduling a doctor’s visit when you have chest pain.
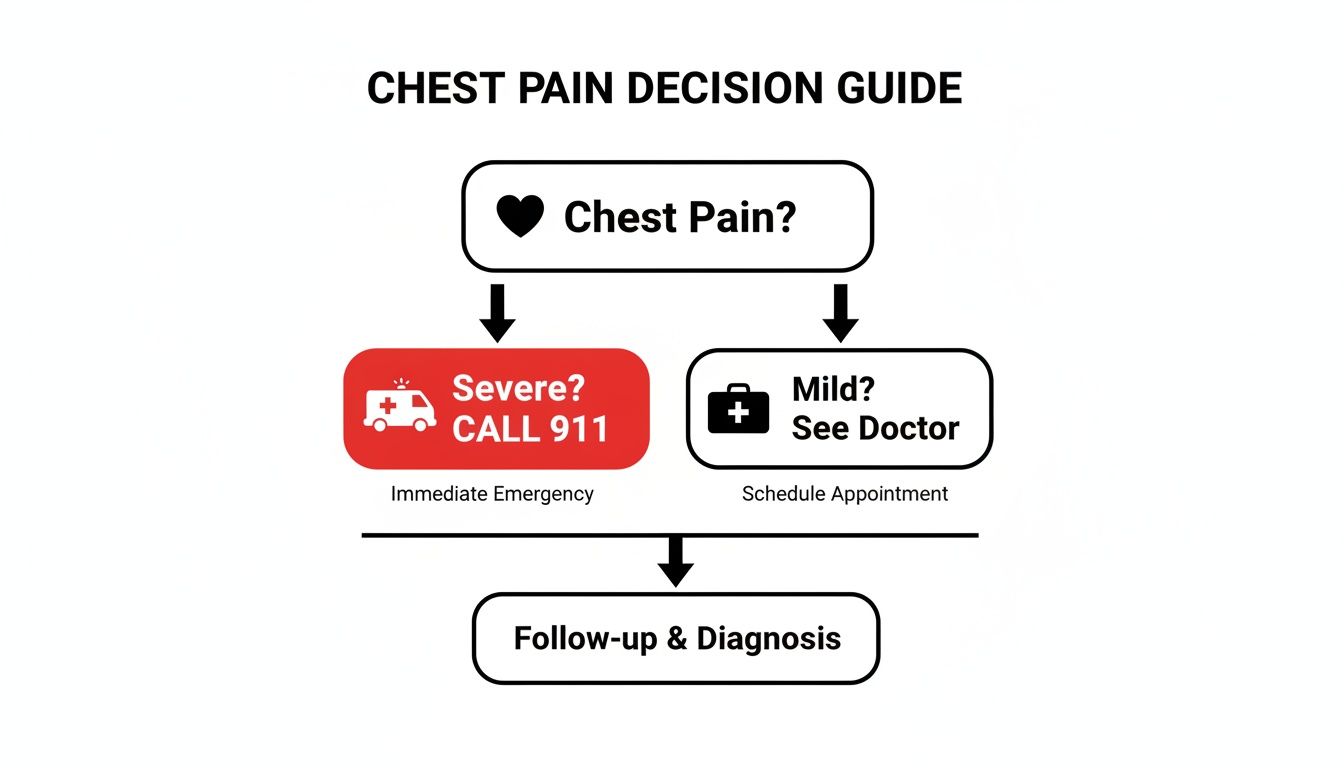
The takeaway here is absolute: severe chest pain is a 911 call, no questions asked. Milder, but persistent, pain warrants a prompt medical evaluation to get to the bottom of it.
How Doctors Diagnose Acid Reflux
If you’ve diligently tried at-home assessments and lifestyle tweaks but aren’t getting the relief you need, it’s time to bring in a professional. Getting a definitive answer to the question, “Do I have acid reflux?” requires a formal medical diagnosis to confirm GORD, assess any damage, and crucially, rule out other conditions.
During your first visit, the conversation is key. Your doctor will want to dive into the details you’ve tracked in your symptom diary—the frequency, the severity, and the specific triggers you’ve noticed. A detailed patient history is often so revealing that an experienced physician can make a strong presumptive diagnosis of GORD based on your story alone.
But if your symptoms are severe, don’t respond to initial treatments, or if you have any “red flag” symptoms, your doctor will likely recommend more specific tests to get a precise look at what’s happening.
Looking Inside with an Upper Endoscopy
Think of an upper endoscopy as a fact-finding mission inside your digestive tract. It’s the most direct way for a doctor to see the health of your esophagus, stomach, and the top part of your small intestine with their own eyes.
For this procedure, a thin, flexible tube with a tiny camera on the end—an endoscope—is guided down your throat while you’re comfortably sedated. This gives your doctor a live video feed, allowing them to spot:
- Esophagitis: Visible inflammation or irritation of the esophageal lining caused by acid exposure.
- Barrett’s Esophagus: A more serious condition where the cells lining the esophagus change to resemble intestinal cells, which increases the risk of cancer.
- Esophageal Strictures: A narrowing of the esophagus caused by scar tissue from years of acid damage.
The procedure itself is painless and provides invaluable visual evidence. It confirms not just if you have reflux, but how much of an impact it’s had over time.
Tracking Reflux with Ambulatory pH Monitoring
While an endoscopy shows the physical results of reflux, ambulatory pH monitoring measures the reflux itself. This test is like a 24-hour surveillance operation, recording every single time acid escapes from your stomach into your esophagus. It’s the gold standard for confirming a GORD diagnosis, especially when symptoms are unusual or don’t fit the classic pattern.
A very thin, flexible tube is passed through your nose and positioned just above your lower esophageal sphincter. This tube connects to a small recording device you wear on your belt for 24 hours. You’ll go about your normal day, pressing a button on the device whenever you feel symptoms, which helps your doctor correlate what you’re feeling with actual reflux events.
This test provides undeniable data. It quantifies how often acid reflux occurs, how long the acid stays in the esophagus, and whether your symptoms truly line up with these events.
The global impact of GORD is significant, causing 6.34 million Disability-Adjusted Life Years (DALYs) in 2021, a number that has nearly doubled since 1990. Projections show this trend continuing, highlighting the importance of accurate diagnostic tools to ensure people get effective treatment and maintain their quality of life. You can read the full research about these projections and their public health implications.
Measuring Muscle Strength with Esophageal Manometry
Finally, if your doctor suspects a muscle function issue is at the root of your problems, they may recommend an esophageal manometry test. This procedure is all about assessing the strength and coordination of the muscles in your esophagus, particularly how well the lower esophageal sphincter is doing its job.
For this test, a thin, pressure-sensitive tube is passed through your nose into your esophagus and stomach. As you take small sips of water, the sensors on the tube measure the rhythmic muscle contractions that move food down. The results can show if your LES is too weak to stay shut or if the esophageal muscles aren’t contracting properly to clear out refluxed material.
These diagnostic tools give your medical team a complete, evidence-based picture of your condition. Armed with this data, they can move beyond guesswork and create a treatment plan that’s built for you. If you’re seeking a top-tier physician to guide you through this process, exploring a network of vetted concierge internal medicine doctors can connect you with specialists known for their diagnostic precision.
Creating Your Path to Relief
Finding real, lasting relief from acid reflux isn’t about some miracle cure. It’s a journey—a systematic one that starts with simple but powerful lifestyle shifts and only moves to medical support when it’s genuinely needed. This tiered approach puts you back in the driver’s seat, helping you build a strategy that works for your body and your symptoms.
The foundation, always, is diet and daily habits. Think of these changes less as restrictions and more as reinforcing the gate—your lower esophageal sphincter—so it can do its job and keep acid where it belongs.
Starting with Lifestyle and Dietary Shifts
The evidence is clear: small, consistent changes can deliver huge results. For many, the single most impactful place to start is managing weight. Even a modest drop on the scale can dramatically decrease the pressure on your abdomen and, in turn, slash the frequency of reflux episodes.
Beyond weight, here are a few practical adjustments that make a real difference:
- Identify Your Triggers: You probably know the usual suspects—spicy foods, citrus, tomatoes, caffeine, chocolate, and fatty meals. Your symptom diary is your best friend here, helping you pinpoint exactly what sets you off.
- Adjust Meal Timing: Stop eating at least three hours before you go to bed. This gives your stomach plenty of time to empty, preventing acid from creeping up your esophagus the moment you lie down.
- Optimize Sleep Position: Elevating the head of your bed by six to eight inches is a game-changer. It puts gravity on your side, making it physically harder for stomach acid to travel upward. A good wedge pillow is a simple, effective tool for this.
These lifestyle modifications are the bedrock of managing reflux. For many people, they provide enough relief to avoid medication altogether.
The goal isn’t to overhaul your life overnight. It’s about making strategic, sustainable changes that reduce the frequency and severity of your symptoms, one habit at a time.
Understanding Your Medication Options
When lifestyle adjustments alone don’t cut it, medication offers the next line of defense. These treatments work in different ways, either neutralizing the acid that’s already there or, more powerfully, stopping your body from producing so much of it.
- Antacids: Think of these as the first responders. Tums, Rolaids, and others provide fast, temporary relief by neutralizing stomach acid on contact. They’re great for occasional heartburn but don’t do anything to prevent the next episode.
- H2 Blockers: Medications like Pepcid step it up a notch. They reduce acid production for a longer stretch than antacids, typically giving you up to 12 hours of relief.
- Proton Pump Inhibitors (PPIs): These are the heavy hitters. PPIs like Prilosec and Nexium are the most powerful option because they block acid production at the source for up to 24 hours. This gives an irritated, inflamed esophagus critical time to heal.
Choosing the right medication isn’t a DIY project. It’s essential to work with a healthcare professional who can guide you. They’ll help you weigh the benefits against potential long-term effects, making sure you’re on the lowest effective dose for the shortest possible time. Finding a trusted physician is key, and a curated network can show you how to find the best doctor for your specific needs.
Advanced Medical and Surgical Solutions
For a small slice of people with severe, unrelenting GORD that just won’t respond to anything else, more advanced options are on the table. We typically only consider these when reflux is destroying someone’s quality of life or leading to serious complications.
Procedures like a Nissen fundoplication surgery work by physically reinforcing the lower esophageal sphincter, creating a much stronger barrier against reflux. Other, less invasive techniques are also available. These are serious decisions reserved for specific cases, requiring a deep conversation with a gastroenterology specialist to make sure the long-term benefits truly outweigh the risks.
Common Questions About Acid Reflux
Once you’ve got a handle on the symptoms, causes, and treatment options, a few practical questions almost always come up. Getting clear answers to these day-to-day concerns is a huge part of feeling in control and finally figuring out, “Do I really have acid reflux?”
Every person’s experience with GORD is a little different, and understanding these nuances is what helps you build a management plan that actually works for you.
Can Stress Make My Acid Reflux Worse?
Absolutely. While stress isn’t the direct culprit causing the valve at the bottom of your esophagus to malfunction, think of it as a powerful amplifier for your symptoms. High levels of stress can actually ramp up stomach acid production while simultaneously making the lining of your esophagus more sensitive to it.
This kicks off a vicious cycle. Worse yet, when we’re stressed, we often reach for things that are well-known reflux triggers—comfort foods, extra coffee, or just poor sleep. This is why incorporating genuine stress-management techniques like meditation, deep breathing, or even a brisk walk can be a surprisingly effective part of your relief plan.
Your mind and your gut are deeply connected. Managing your stress isn’t just a “nice-to-have” for your mental health—it’s a non-negotiable part of getting long-term control over acid reflux.
Is It Safe to Take Medications Like PPIs Long-Term?
This is one of the most important conversations you need to have with your doctor. Medications like Proton Pump Inhibitors (PPIs) are incredibly good at what they do—reducing stomach acid and giving your esophagus a chance to heal. However, using them for years on end can come with certain risks, like potential nutrient deficiencies or other side effects.
The goal in medicine is always to use the lowest effective dose for the shortest time necessary. Your physician is the one who can help you weigh the very real benefits of controlling your GORD against any potential long-term risks for your specific health profile. This isn’t a one-and-done decision; it requires regular check-ins to make sure the balance is still right.
Do I Have to Give Up My Favorite Foods Forever?
Not necessarily. Successfully managing reflux is about finding your personal balance, not about total deprivation. While a few people might find they have to completely eliminate a very specific, severe trigger food, most discover they can still enjoy their favorites in moderation—it just takes some planning.
This is where keeping a food diary becomes your secret weapon. It helps you pinpoint your unique thresholds. You might learn that a small cup of coffee in the morning is perfectly fine, but that second cup in the afternoon is a guaranteed recipe for heartburn. Or maybe a spicy dinner is manageable as long as you stay upright for a few hours afterward. It’s all a process of learning your body’s specific rules of the road.
Navigating the complexities of acid reflux requires expert guidance from a physician who understands your unique health profile. The network of specialists at Haute MD connects you with top-tier, vetted doctors who can provide the precise diagnosis and personalized care you deserve. Find a leading specialist near you today on hauteliving.com/hautemd.

