The physician shortage by specialty isn’t a single, uniform crisis. It’s a series of specific, critical gaps where certain fields—especially primary care, surgical subspecialties, and psychiatry—are facing a severe deficit of doctors. This imbalance puts a tremendous strain on the entire U.S. healthcare system, and the consequences for patient care are already being felt nationwide.
The Widening Gaps in US Healthcare
Think of the healthcare system as an intricate ecosystem. Each specialty is a vital species, and when a foundational one like primary care is threatened, the whole environment becomes unstable. When patients can’t get in to see a family doctor for preventive care or an initial diagnosis, they often delay treatment.
This delay means small problems can escalate into severe health issues, eventually forcing them into emergency rooms or to highly specialized doctors. It’s a domino effect that overloads already-strained specialists and hospitals.
The numbers here are stark. By 2025, the U.S. is projected to be short somewhere between 61,700 and 94,700 physicians. The deficit in non-primary care specialties alone—including critical surgical and medical fields—is expected to hit between 37,400 and 60,300 physicians. This isn’t some distant problem; it’s a reality impacting millions of Americans right now.
Primary Care: The First Line of Defense Is Crumbling
The epicenter of the physician shortage has always been primary care. These are the generalists—your family medicine doctors, internists, and pediatricians—who are absolutely essential for managing chronic diseases, providing routine screenings, and acting as the quarterback for your entire health journey.
The shortfall here is particularly alarming because the impact is immediate and direct:
- Longer wait times for a simple check-up or a sick visit.
- Reduced access to the very preventive care that stops major health problems before they start.
- An increased burden on emergency rooms, which become the de facto clinic for non-urgent issues.
This deficit is forcing many to re-evaluate how they approach their health. For those who can’t afford to wait, understanding the key differences between concierge medicine vs traditional healthcare is becoming less of a luxury and more of a necessity.
Top 5 Medical Specialties Facing Critical Shortages
While primary care feels the brunt of the shortage, several specialized fields are also under intense pressure. The following table highlights the specialties where the gaps are projected to be most severe, creating significant challenges for patient access and care delivery across the country.
| Specialty | Projected Shortfall by 2025 | Primary Driving Factors |
|---|---|---|
| Primary Care | 21,100 – 55,200 | Aging population, high burnout rates, lower reimbursement |
| Psychiatry | 14,280 – 31,109 | Increased demand for mental health services, stigma, low residency fill rates |
| General Surgery | 13,800 – 23,000 | Grueling training, demanding lifestyle, retirement of older surgeons |
| Neurology | ~1,800 (11% deficit) | Aging population (Alzheimer’s, Parkinson’s), complex chronic disease mgmt |
| Cardiology | ~7,080 | Rise in chronic heart conditions, lengthy training, high stress |
These numbers aren’t just statistics; they represent delayed diagnoses, postponed surgeries, and communities left without access to the specialized care they desperately need. Each shortage has its own unique story, driven by a complex mix of economic, educational, and professional pressures.
Specialized Fields Under Intense Pressure
Beyond the top five, other specialties are feeling an intense squeeze. Psychiatry, for instance, is facing a profound shortage that leaves countless people struggling with mental health conditions unable to find care.
Similarly, general surgery and various surgical subspecialties are grappling with deficits that can delay crucial procedures. This is especially true in rural and underserved communities where a single specialist might be the only option for hundreds of miles.
The physician shortage is more than a statistic; it’s a direct threat to patient access and quality of care. When one specialty is understaffed, the ripple effects are felt across the board, from delayed diagnoses in primary care to postponed life-saving surgeries.
Each specialty shortage is driven by its own distinct set of factors, whether it’s the grueling training periods, staggering burnout rates, inadequate reimbursement, or simply an aging physician workforce heading for retirement. As we dig into these deficits, it’s clear that a one-size-fits-all solution won’t work. We need a targeted approach that understands the unique pressures each medical field is facing.
Which Surgical and Medical Specialties Are Most Affected?
While headlines talk about a general physician shortage, the reality on the ground is much more specific. The impact isn’t spread evenly; some surgical and medical specialties are facing deficits so severe they’re creating dangerous bottlenecks in patient care. The result is long waits for critical procedures and consultations that can turn a manageable condition into a crisis.
Ever tried to book an appointment with a urologist for a pressing issue, only to be told the next opening is six months away? Or found yourself living in a rural area where the nearest thoracic surgeon is a four-hour drive? These aren’t just hypotheticals—they are the direct, frustrating consequences of a deepening specialty-specific physician shortage.
This chart gives you a clear visual breakdown of just how stark these shortages are across the board.
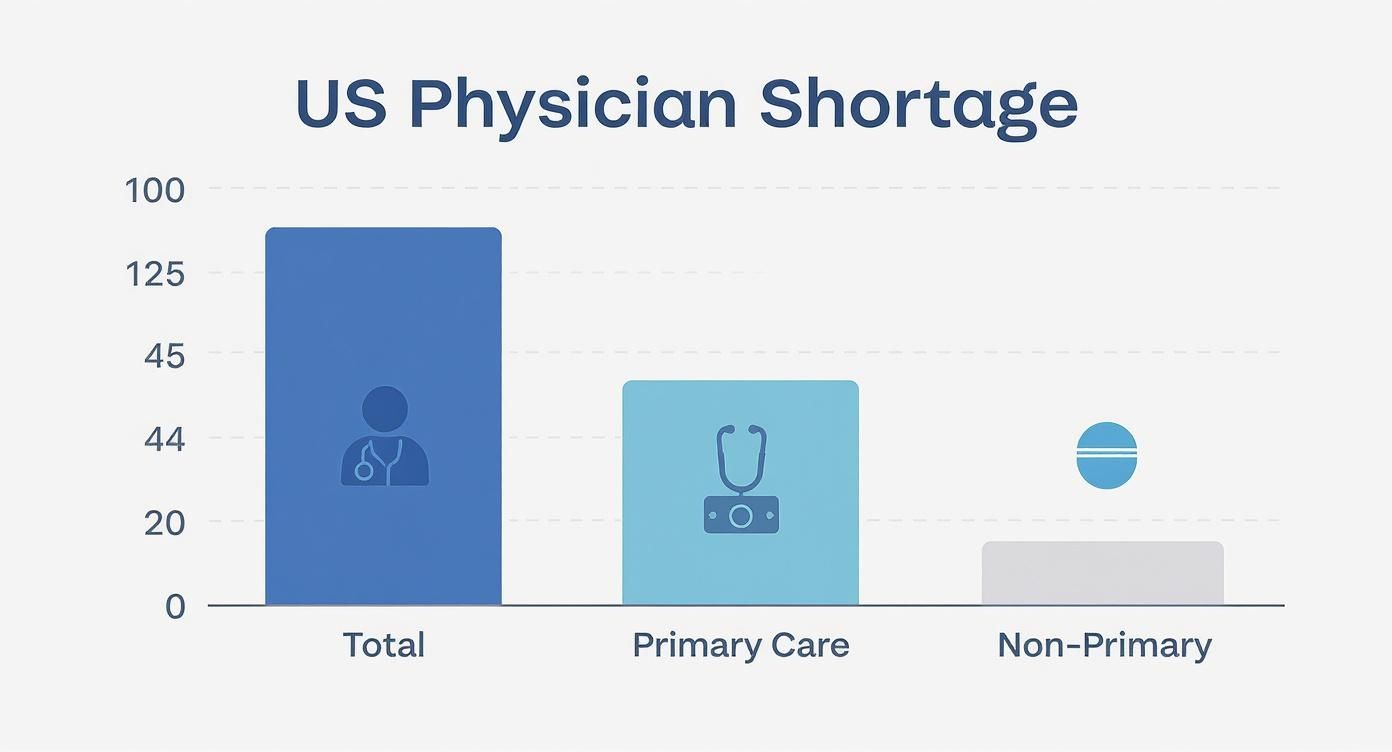
As the data shows, the gap in non-primary care—the highly specialized fields—is substantial. This is where demand is rapidly outpacing the supply of trained professionals.
The Surgical Squeeze
Surgical fields are uniquely vulnerable. The training pipeline is brutally long, often demanding a decade or more of post-graduate education and residency. This massive commitment, paired with a high-stress environment and grueling lifestyle, makes it incredibly difficult to replace the wave of surgeons now heading into retirement.
Certain surgical specialties are facing the most extreme shortfalls. Projections show thoracic surgery with a supply adequacy of just 69%, meaning we’re facing a massive 31% deficit of qualified surgeons. It’s a similar story in urology, which is staring down a staggering 41% shortage. You can dig deeper into these numbers by reviewing the official physician projections factsheet.
This dangerous imbalance means that while major cities might still have options, smaller communities are often left with critical, life-threatening gaps in care.
Medical Specialties Facing Unprecedented Demand
On the medical side, specialties that serve our aging population are under immense strain. As the baby boomers get older, the rates of chronic and complex diseases are soaring, creating a surge in demand that the physician supply simply can’t handle.
Neurology is a perfect example of this crunch. The demand for neurologists is expected to jump by 16% by 2025, driven by the rising prevalence of conditions like Alzheimer’s, Parkinson’s, and stroke. The problem? The supply of neurologists is only projected to grow by 11%, leaving a significant deficit.
That gap isn’t just a statistic. It translates directly into longer wait times for diagnosis and treatment, which can have devastating consequences for patients with time-sensitive neurological conditions.
Other medical specialties are feeling similar pressure:
- Ophthalmology: With an aging population comes a higher incidence of cataracts, glaucoma, and macular degeneration, straining the capacity of available eye surgeons.
- Oncology: As cancer treatments become more complex and survival rates improve, the need for long-term oncological care is growing faster than the number of practicing oncologists.
- Rheumatology: The management of autoimmune diseases requires specialized, ongoing care, a field where patient loads are high and new physicians are scarce.
These shortages don’t exist in a vacuum. They intersect with other complex medical needs, like reproductive health. Patients navigating these challenges may find it helpful to learn how to find top-tier fertility specialists who can provide expert guidance in a strained system.
Ultimately, understanding which fields are most affected is the first step toward navigating the healthcare landscape and advocating for the timely, specialized care you need.
The Driving Forces Behind the Specialty Shortage
To really get a handle on the physician shortage, you have to look past the surface-level numbers. This isn’t just a simple supply-and-demand issue; it’s a perfect storm of powerful, interconnected forces that are cranking up the need for specialized care while simultaneously shrinking the pool of doctors available to provide it.
An Unfolding Demographic Collision
First and foremost, we’re in the middle of a massive demographic shift. The “Silver Tsunami”—the aging of the Baby Boomer generation—means millions more Americans are living longer. That’s great news, but it also means they’re managing more chronic conditions that require ongoing, specialized attention. This has placed an unprecedented strain on fields like cardiology, neurology, and oncology.
At the exact same time, the physician workforce is graying, too. A huge slice of our most experienced specialists are nearing retirement, creating a knowledge and experience vacuum that is incredibly difficult to fill. This collision course—soaring patient demand meeting a wave of physician retirements—is ground zero for the care gaps we see today.
The Physician Pipeline Problem
Even with a steady stream of brilliant and motivated medical school graduates, we physically can’t train new specialists fast enough. The real bottleneck is in graduate medical education (GME)—specifically, the limited number of residency slots where new doctors get their hands-on specialty training.
For over two decades, a federal cap on funding for these residency positions has choked the system’s ability to grow. It’s like having a four-lane highway of med school grads all trying to merge onto a two-lane bridge of residency programs.
Because of this structural limit, thousands of qualified medical school graduates can’t secure a residency spot each year. Their careers are delayed, sometimes permanently, before they even start. This creates an artificial ceiling on the number of new specialists entering the field, no matter how desperately patients need them.
The Burnout Epidemic
Beyond demographics and training caps, a more corrosive force is hollowing out the medical profession from the inside: physician burnout. This isn’t just about feeling stressed; it’s a full-blown crisis of emotional exhaustion, cynicism, and a feeling of ineffectiveness driven by systemic pressure.
Doctors today are buried in administrative tasks. They spend countless hours wrestling with clunky electronic health records and battling insurance companies for prior authorizations—work that steals time and energy away from actual patient care.
The fallout from this burnout directly fuels the physician shortage:
- Early Retirement: Veteran physicians are leaving medicine years ahead of schedule.
- Reduced Hours: Others are cutting back their clinical time simply to achieve a sustainable work-life balance, which shrinks overall patient capacity.
- Leaving the Profession: A growing number are abandoning clinical practice entirely for careers in different industries.
This exodus of talent makes the existing shortages even worse.
Projections paint a stark picture: a total shortage of over 81,000 full-time equivalent physicians by 2035. With 26 out of 36 specialties expected to face deficits, the supply in critical fields like thoracic surgery and ophthalmology is projected to meet only 69% and 70% of demand, respectively. You can discover more insights about these recruiting challenges and workforce projections.
Economic and Regulatory Pressures
Finally, the economic realities of modern medicine can’t be ignored. Reimbursement rates from Medicare, Medicaid, and private insurers have consistently failed to keep up with the ballooning costs of running a practice, hitting independent specialists particularly hard.
Scope-of-practice laws—which dictate the services that non-physician providers like nurse practitioners can offer—also shape the landscape. While expanding these roles can help ease the burden in primary care, the debate over how and where they fit into complex specialty fields is ongoing.
To get a clearer view, let’s break down these interconnected drivers.
Root Causes of the Physician Shortage
| Category | Specific Driver | Impact on Physician Supply |
|---|---|---|
| Demographics | Aging “Baby Boomer” Population | Increases demand for specialists (cardiology, oncology, etc.) |
| Aging Physician Workforce | Shrinks supply as experienced doctors retire | |
| Training & Education | Residency Slot Cap (GME) | Artificially limits the number of new specialists trained each year |
| Long Training Pathways | Delays entry into the workforce for 7-10+ years post-medical school | |
| Workforce Dynamics | Physician Burnout | Drives early retirement, reduced hours, and career changes away from medicine |
| Administrative Burden | Reduces time available for direct patient care, lowering capacity | |
| Economic & Policy | Declining Reimbursement | Makes certain specialties less financially viable, discouraging new entrants |
| Scope-of-Practice Laws | Creates uncertainty and debate around care delivery models |
Together, these forces create an incredibly difficult environment. They don’t just explain the current physician shortage by specialty; they pose a direct threat to the long-term stability of our entire healthcare system.
How Patients Can Navigate a Strained System
Let’s be honest: the data on physician shortages can feel overwhelming. It translates into real-world frustrations—waiting months for a specialist, feeling rushed through a 10-minute consultation, and the nagging sense that getting the care you need has become a full-time job.
But a strained system doesn’t mean you have to accept subpar care. It just means you have to be more strategic. By becoming a proactive, informed advocate for your own health, you can secure timely access to the specialists you need.

Embrace New Models of Care
The traditional office visit is no longer your only—or even best—option. Modern healthcare now offers flexible alternatives that can help you bypass the long queues for in-person appointments, especially for follow-ups, prescription refills, or initial consults for non-urgent issues.
- Leverage Telehealth: Virtual consultations give you direct access to specialists from the comfort of your home. This is a game-changer for fields like psychiatry and dermatology, where a visual assessment is key but a physical exam isn’t always necessary.
- Utilize Advanced Practice Providers (APPs): For routine primary care, wellness visits, and managing stable chronic conditions, consider seeing a Nurse Practitioner (NP) or Physician Assistant (PA). These highly skilled professionals work alongside physicians and can often offer more immediate appointments for less complex needs.
These modern tools help you get care faster, saving in-person physician time for the complex diagnostic work and treatment challenges that truly require it. And for those seeking even greater access, it’s worth exploring the ways to find top-rated physicians near me who may offer more personalized concierge or direct care models.
Become a Proactive Patient
In a system defined by scarcity, waiting for problems to become urgent is a losing game. The key is to get ahead of the curve by planning your healthcare needs well in advance and meticulously managing your own medical journey.
Don’t wait for symptoms to become urgent. The best time to book your annual check-ups and routine screenings with in-demand specialists is months ahead. Getting on their schedule early ensures you have a confirmed spot and avoids last-minute scrambles for an appointment.
Here are a few actionable steps you can take today:
- Schedule in Advance: Before you leave your current appointment, book your next annual physical or specialist follow-up. Get it on the calendar now.
- Keep Meticulous Records: Maintain your own file with test results, medication lists, and visit summaries. This makes you an efficient, prepared patient who gets the most out of every single consultation.
- Prepare for Appointments: Show up with a clear, concise list of questions and concerns. This ensures your limited time with the physician is focused and incredibly productive.
Advocate for Your Health
Ultimately, you are the CEO of your own health. When you’re told there’s a three-month wait for a specialist, don’t just accept it. Politely ask to be put on a cancellation list. If your condition is worsening, clearly communicate this to your primary care provider’s office so they can advocate on your behalf for a sooner appointment.
Being persistent, organized, and informed empowers you to navigate the complexities of today’s healthcare system. By taking these steps, you can secure the high-quality care you deserve, even when the best specialists are in high demand.
Strategic Opportunities for Healthcare Practices
For savvy healthcare leaders, the physician shortage isn’t just a crisis—it’s a market correction that creates enormous opportunities. The challenges are real, of course. Recruiting and retaining top talent has never been more competitive. But the intense demand for specialized care is also a powerful driver of innovation.
The old models are breaking. High demand and scarce supply mean elite physicians now have unprecedented leverage. This reality forces practices to compete on more than just salary. They have to build a better place to work, an environment that actively prevents burnout and offers a sustainable, rewarding career path.
Embracing New Care Delivery Models
One of the most powerful responses to the broken traditional system is the rise of alternative care models. These frameworks completely rethink the physician-patient relationship, shifting the focus from volume to value and accessibility. For practices willing to adapt, they offer a clear roadmap to success.
Two models, in particular, are proving to be game-changers:
- Concierge Medicine: This is the pinnacle of personalized care. By charging a membership fee, physicians dramatically shrink their patient panel. This allows for unhurried, 60-minute appointments, 24/7 direct access, and a deep dive into proactive, preventive medicine—exactly what high-net-worth patients are actively searching for.
- Direct Primary Care (DPC): Think of DPC as a more accessible version of the same philosophy, typically focused on primary care. By cutting out the insurance middleman, DPC practices slash administrative waste, lower costs, and let doctors concentrate on one thing: patient health.
Both models directly solve the biggest frustrations patients face today: endless wait times, rushed visits, and feeling like a number. For physicians, they offer a lifeline out of the high-volume, low-margin burnout factory, making them incredibly potent tools for both recruitment and retention.
The Crucial Role of Technology
In today’s healthcare environment, technology isn’t a line item on the budget; it’s a core strategic asset. For practices stretched thin, the right tech acts as a force multiplier, allowing them to care for more patients without compromising the quality of that care.
In an era of scarcity, efficiency isn’t just a goal; it’s a survival strategy. The practices that not only survive but thrive will be those that master technology to automate grunt work, streamline clinical flows, and extend their reach far beyond their physical walls.
Here are the key technologies that deliver a real competitive edge:
- Telehealth Platforms: The clinic is no longer defined by four walls. Telehealth offers incredible flexibility for scheduling, boosts patient convenience, and creates highly efficient workflows for follow-ups and routine check-ins.
- AI-Powered Diagnostic Tools: Artificial intelligence can shoulder repetitive, data-heavy tasks like analyzing medical images or flagging anomalies in patient charts. This frees up a physician’s most valuable resource—their cognitive bandwidth—for complex, high-stakes decisions.
- Streamlined Electronic Health Records (EHRs): Clunky, outdated EHR systems are a primary driver of physician burnout. Investing in a modern, intuitive platform is one of the single most effective ways to reduce the administrative drag that saps physician morale and productivity.
By investing smartly in these areas, healthcare practices can turn the physician shortage from a threat into a defining opportunity. It’s a chance to build a more resilient, efficient, and physician-centric organization—one that’s perfectly positioned to meet the needs of patients and providers for years to come.
Common Questions About the Physician Shortage
As you dig into the physician shortage, a few key questions always come up. Here are some straightforward answers to help you make sense of the real-world impact.
Which Single Specialty Is Facing the Worst Physician Shortage?
It’s a great question, and the honest answer is: it depends on how you measure it.
If you’re talking about sheer numbers, primary care is in the toughest spot. The absolute deficit of family doctors, internists, and pediatricians is massive, and that creates the access problems we all feel—longer waits for physicals, trouble finding a new doctor, and overwhelmed ERs.
But if you look at it by percentage, some highly specialized surgical fields are in a more critical state. Think of specialties like thoracic surgery or urology. While they need fewer doctors overall, the proportional gap between the number of specialists we have and the number we need is often much wider. So, the “worst” shortage is a matter of perspective: the widespread crisis in primary care or the acute, razor-thin supply in certain surgical fields.
How Does the Physician Shortage Affect Rural Versus Urban Areas?
The shortage hits rural America disproportionately hard. It’s a completely different reality. In a major city, you might face a frustrating six-month wait to see a top neurologist. In a rural community, that neurologist might not exist for a hundred miles or more.
This geographic divide is one of the most challenging parts of the shortage. It forces people to take a full day off work, drive for hours, and pay for gas and lodging just to get basic specialty care that city dwellers take for granted. Without major changes, this healthcare gap between urban and rural communities is only going to get wider.
The physician workforce has grown in absolute numbers but is severely maldistributed. An increasing supply of doctors doesn’t automatically mean rural or underserved communities get better access to care, a problem worsened by how medical training is funded and located.
What Is Being Done to Solve the Physician Shortage?
There’s no single silver bullet, so the strategy has to be multi-faceted. Progress is slow, but the efforts generally fall into two buckets: training more doctors and making the current workforce more efficient. The main plays are:
- Increasing Residency Slots: The biggest bottleneck is the number of doctors we can train after medical school. The primary focus is lobbying to lift the federal cap on Medicare-funded residency positions.
- Expanding Scope of Practice: This involves empowering highly skilled Advanced Practice Providers, like Nurse Practitioners (NPs) and Physician Assistants (PAs), to handle more services independently.
- Using Telehealth: Technology is a huge help in bridging geographic gaps. A specialist in New York can consult with a patient in rural Montana, dramatically improving access where it’s needed most.
- Improving Retention: We’re losing too many experienced doctors to burnout. Solutions focus on improving working conditions and creating systems that prevent physicians from leaving the profession early.
Will Technology Like AI Solve the Doctor Shortage?
Technology is an incredibly powerful ally, but it’s not a replacement for a doctor. It’s a force multiplier.
Think of AI as the ultimate physician’s assistant. It can crush the administrative burden—charting, paperwork, insurance claims—that burns doctors out. It can also help analyze scans and data, pointing out potential issues a human eye might miss. This frees up a physician to focus on what really matters: complex problem-solving and direct patient interaction.
Telehealth works the same way, extending a doctor’s reach but not replacing their expertise. You still need a trained clinician for hands-on procedures, managing complicated cases, and providing the kind of empathetic care that technology can’t replicate. AI helps us manage the crisis, but it won’t solve the fundamental need for more highly trained doctors.
Finding a trusted, board-certified specialist shouldn’t feel impossible, even in a strained system. Haute MD is the premier network connecting discerning patients with the nation’s most elite, rigorously vetted physicians. From executive health to advanced surgical care, our platform provides direct access to the innovators and leaders in medicine. Explore our curated network of top doctors.

