Cardiac electrophysiology is the highly specialized field of medicine that deals with your heart’s electrical system and its rhythm. Think of it as the intersection of cardiology and electrical engineering, focused entirely on diagnosing and fixing problems with the heart’s internal wiring.
When that wiring is working perfectly, you never notice it. But if there’s a short circuit, the results can be anything from a minor flutter to a life-threatening emergency.
Decoding Your Heart’s Electrical System
Your heart isn’t just a muscle; it’s a remarkably sophisticated electrical pump. Every single beat—more than 100,000 times a day—is triggered by a tiny, precise electrical impulse. This signal travels along specific pathways, telling your heart’s chambers to contract in a perfectly coordinated sequence. It’s this flawless timing that allows your heart to pump blood efficiently to your brain and body.
But what happens when that system goes awry? If the signal gets blocked, takes a detour, or fires erratically, your heart’s rhythm can become too fast, too slow, or just plain chaotic. This is called an arrhythmia.
This is precisely where the specialized field of cardiac electrophysiology comes in. A cardiac electrophysiologist, or EP, is a cardiologist who has dedicated years to extra training to become a master of the heart’s electrical functions. Their job is to be the expert electrician for your heart.
The Role of an Electrophysiologist
An electrophysiologist focuses on one thing: diagnosing and treating heart rhythm disorders. Their expertise goes far beyond general cardiology, homing in on the specific electrical signals that govern your heartbeat. They are the specialists you see for conditions that cause symptoms like:
- Palpitations: That unsettling feeling of a fluttering, racing, or pounding heart.
- Dizziness or Lightheadedness: A sign that the heart isn’t pumping enough oxygen-rich blood to the brain.
- Syncope (Fainting): A temporary loss of consciousness caused by a sudden drop in blood flow.
- Fatigue: A deep, persistent tiredness that rest doesn’t seem to fix.
- Shortness of Breath: Difficulty breathing, especially when you’re active.
A Growing Field of Medicine
The importance of electrophysiology is growing at an incredible pace. As our diagnostic tools get more sophisticated and public awareness of arrhythmias increases, the demand for EP procedures is skyrocketing.
The global electrophysiology market was valued at around $4.3 billion and is projected to surge past $10.82 billion by 2033. This isn’t just a number—it reflects the rising prevalence of conditions like atrial fibrillation and the stunning success of modern treatments in giving people their lives back. You can explore the full market projections for a deeper dive into these trends.
To help simplify these concepts, here’s a quick overview of what cardiac electrophysiology covers.
Cardiac Electrophysiology at a Glance
| Concept | Simple Explanation |
|---|---|
| Electrical Conduction | The system of natural “wires” that sends signals through the heart to make it beat. |
| Sinoatrial (SA) Node | The heart’s natural pacemaker. It’s where the electrical signal originates. |
| Arrhythmia | Any abnormal heart rhythm—too fast (tachycardia), too slow (bradycardia), or irregular (like atrial fibrillation). |
| Electrophysiologist (EP) | A cardiologist who is an expert in diagnosing and treating arrhythmias. Essentially, a “heart electrician.” |
| EP Study | A diagnostic procedure that maps the heart’s electrical activity to find the source of an arrhythmia. |
| Catheter Ablation | A treatment that uses heat or cold energy to eliminate the small area of heart tissue causing the arrhythmia. |
This table is just a starting point, but it captures the essence of this vital medical specialty.
The bottom line is this: while a general cardiologist manages the heart’s overall health—its arteries, valves, and muscle—an electrophysiologist is the definitive expert for any problem related to its rhythm. They are the specialists called in when the heart’s natural pacemaker or electrical pathways fail, working to restore stability and improve quality of life for millions.
How a Healthy Heartbeat Works
To really understand what cardiac electrophysiology fixes, you first have to appreciate the masterpiece that is a healthy heart. Think of it like a world-class orchestra. Every single musician has to play their part in perfect time to create a beautiful symphony. If even one instrument is slightly off-key or out of sync, the whole performance can fall apart.
Your heart’s electrical system is a lot like that. It runs on a precise, coordinated sequence of electrical signals to pump blood with maximum efficiency. A healthy, steady rhythm is the bedrock of cardiovascular wellness, making sure your entire body gets the oxygen it needs to thrive.
The Conductor of the Heart
At the very top of the heart, nestled in the right atrium (the upper right chamber), is a tiny cluster of highly specialized cells called the sinoatrial (SA) node. This is the heart’s natural pacemaker—the orchestra’s conductor. It spontaneously generates an electrical impulse that sets the pace for your entire heartbeat, usually somewhere between 60 to 100 beats per minute when you’re at rest.
This initial spark from the SA node is the downbeat that starts the whole piece. It’s the origin of what doctors call a normal sinus rhythm—the medical term for a healthy, steady heartbeat that starts from the correct place.
Tracing the Electrical Signal’s Journey
Once the SA node fires, the electrical signal doesn’t just flood the heart all at once. It travels along very specific pathways, almost like sheet music being passed between musicians in a precise order.
- Step 1: The Atria Contract: The impulse first spreads across the two upper chambers, the atria. This electrical wave causes them to contract, squeezing blood down into the two lower chambers, the ventricles. Think of this as the string and woodwind sections playing their opening notes together.
- Step 2: The AV Node Pause: The signal then arrives at the atrioventricular (AV) node, which sits right between the atria and the ventricles. The AV node is a critical gatekeeper; it intentionally holds the signal for a fraction of a second. This brief pause is absolutely crucial—it gives the ventricles just enough time to fill completely with blood before they get the signal to contract.
- Step 3: The Ventricles Contract: After that calculated delay, the AV node releases the signal. It shoots down a pathway called the bundle of His and into the Purkinje fibers that spread throughout the ventricles. This powerful surge causes the ventricles to contract with force, pumping blood out to the lungs and the rest of the body. This is the grand finale from the brass and percussion sections.
This entire, intricate sequence happens in less than a second, over and over, for your entire life. Understanding this pathway is a core part of both cardiac electrophysiology and proactive heart care. For those interested in staying ahead of potential issues, you can learn more by exploring what is preventive cardiology in our detailed guide.
This process highlights the three core pillars of an electrophysiologist’s work: understanding the heart’s wiring, diagnosing the problem, and fixing the electrical issue.
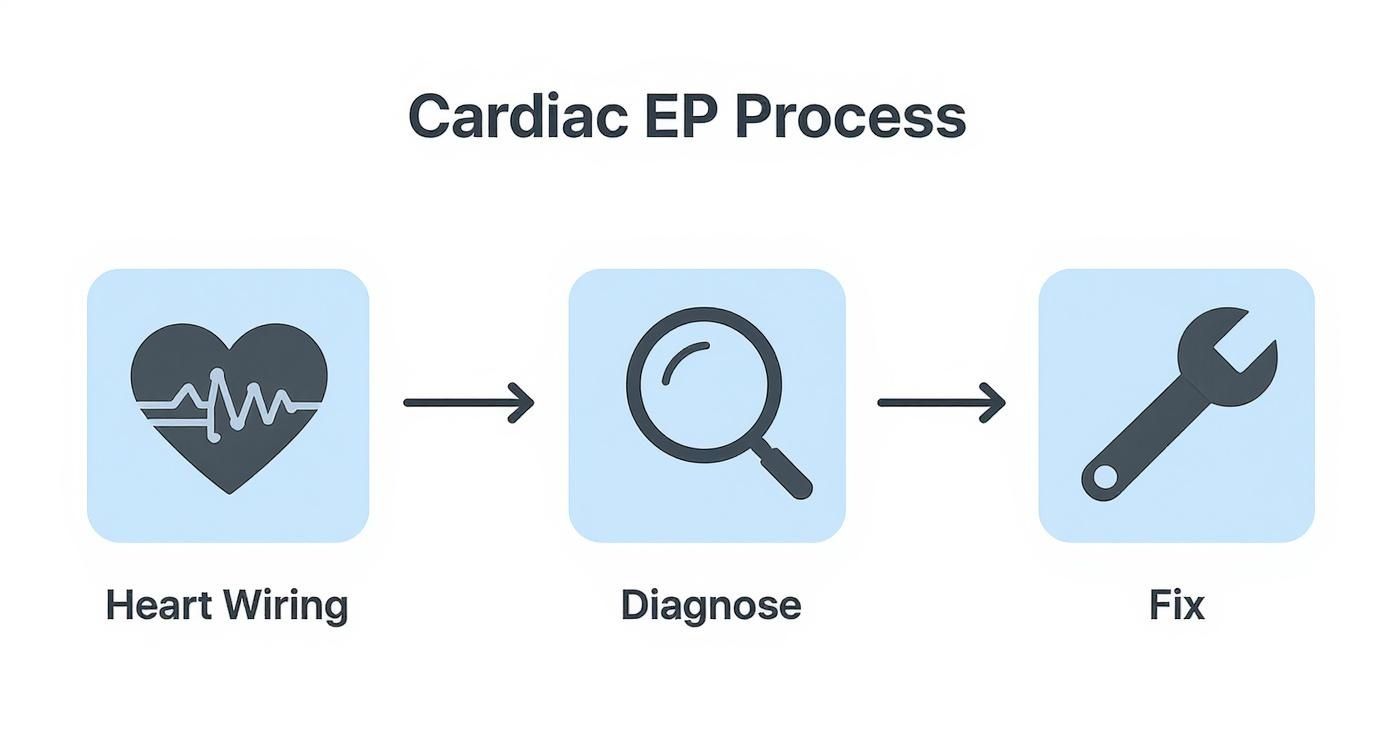
This simple visual breaks the process down: first, you map the heart’s wiring, then you diagnose the fault, and finally, you implement a fix to restore its natural rhythm.
In short, a healthy heartbeat is a testament to perfect timing and flawless communication. The SA node sets the rhythm, the pathways ensure orderly delivery, and the AV node’s pause guarantees peak efficiency. When this system works as designed, blood flows smoothly and your body gets the fuel it needs. It is only when a breakdown occurs in this electrical symphony that an arrhythmia is born—and the expertise of a cardiac electrophysiologist becomes essential to restore harmony.
When Your Heart’s Rhythm Is Disrupted
When the heart’s perfectly timed electrical symphony falters, the result is an arrhythmia—an abnormal heart rhythm. These disruptions can feel like a brief flutter, a racing pulse, or a slow, heavy thud. Each sensation signals a different kind of electrical malfunction.
Understanding what cardiac electrophysiology is really starts with recognizing these different rhythm disturbances. Arrhythmias generally fall into three buckets: those that make the heart beat too quickly (tachycardia), too slowly (bradycardia), or in a completely disorganized, chaotic way.
Each type stems from a unique electrical issue—the very problem a cardiac electrophysiologist is trained to solve.
Rhythms That Are Too Fast
Tachycardia is what happens when the heart’s electrical system starts firing way too rapidly, pushing the resting heart rate above 100 beats per minute. This frantic firing can start in different parts of the heart, leading to distinct conditions with their own sets of symptoms.
One of the most common is Supraventricular Tachycardia (SVT). Here, the abnormally fast rhythm kicks off in the heart’s upper chambers, the atria. People often describe an SVT episode as if a switch was suddenly flipped on, causing a racing heartbeat that can bring on dizziness or shortness of breath.
A far more serious condition is Ventricular Tachycardia (VT), where the rapid rhythm originates in the heart’s lower chambers, the ventricles. Because the ventricles do the heavy lifting of pumping blood to the body, VT can severely compromise blood flow and quickly become life-threatening.
Atrial Fibrillation (AFib): A Special Case of Tachycardia Atrial Fibrillation is the most common arrhythmia out there, affecting millions. Think of it as a complete breakdown in command and control. Instead of beating in a coordinated way, the atria just quiver chaotically. It’s as if the conductor walked out, leaving hundreds of drummers to play a frantic, disorganized solo all at once. The result is an irregular and often very rapid heartbeat.
Rhythms That Are Too Slow
On the other end of the spectrum is bradycardia, defined as a resting heart rate below 60 beats per minute. While a slow pulse can be a sign of elite physical conditioning in an athlete, for most people, it signals an electrical problem.
Bradycardia often happens when the heart’s natural pacemaker, the SA node, simply isn’t firing fast enough. Another common cause is heart block, a condition where the electrical signals get delayed or completely stopped on their way from the atria to the ventricles. It’s like a communication breakdown between the orchestra’s conductor and its musicians—the message just isn’t getting through.
The symptoms of bradycardia are driven by the heart’s inability to pump enough oxygen-rich blood to the body. Watch for:
- Persistent fatigue and weakness
- Dizziness or lightheadedness
- Fainting or near-fainting spells (syncope)
- Shortness of breath with even minimal effort
These issues can seriously impact a person’s quality of life, making even simple daily tasks feel exhausting.
Recognizing Common Arrhythmia Symptoms
While every arrhythmia has a unique electrical signature, many of their symptoms can feel similar. It takes the advanced diagnostic tools of cardiac electrophysiology to pinpoint exactly what’s going on.
To help you get a clearer picture, here’s a quick comparison of common rhythm disorders and what they typically feel like.
Common Arrhythmias Symptoms and Characteristics
| Arrhythmia Type | Heart Rate Characteristic | Common Symptoms |
|---|---|---|
| Atrial Fibrillation (AFib) | Irregularly fast and chaotic | Palpitations, fatigue, shortness of breath, increased stroke risk |
| Supraventricular Tachycardia (SVT) | Abruptly fast and regular | Racing heart, dizziness, chest discomfort |
| Bradycardia | Consistently slow (under 60 bpm) | Fatigue, fainting, lightheadedness, weakness |
If you experience recurring symptoms like palpitations, unexplained dizziness, or fainting spells, it’s a clear signal that your heart’s electrical system needs a closer look. An electrophysiologist has the specialized expertise to decipher these signals, diagnose the specific arrhythmia, and map out a precise plan to get your heart back into its natural, healthy rhythm.
Diagnosing Arrhythmias: From educated guesses to electrical certainty
To fix a faulty electrical circuit, you first need a detailed wiring diagram. The same logic applies to your heart. When your heart’s rhythm goes haywire, an electrophysiologist acts like a master electrician, using a specialized toolkit to map out your heart’s entire electrical grid and find the exact source of the short circuit.

This diagnostic journey usually starts with simple, non-invasive tests. Think of these as initial snapshots that give us a broad overview of your heart’s electrical activity, helping to decide if we need to zoom in for a closer look.
Starting with Non-Invasive Monitoring
The first step is almost always an Electrocardiogram (ECG or EKG). It’s a quick, painless test that records a few seconds of your heart’s electrical signals. An ECG is great for catching an arrhythmia that’s happening right then and there, but it’s just a brief snapshot in time. It can easily miss problems that come and go.
That’s where portable monitors come in. If your symptoms are intermittent, your doctor will likely recommend one of these:
- Holter Monitor: This is a small, wearable device that records your heart’s rhythm continuously for 24 to 48 hours. You simply go about your daily life while it captures a complete log of your heart’s electrical behavior.
- Event Monitor: For symptoms that are less frequent, an event monitor can be worn for several weeks. When you feel a symptom, you press a button to activate the device, giving your doctor crucial data at the exact moment the arrhythmia strikes.
These tools are fantastic for gathering initial clues. But to definitively find the source of a complex arrhythmia, specialists need something more powerful. They need an Electrophysiology Study.
The Electrophysiology Study Explained
The Electrophysiology (EP) Study is the gold standard for diagnosing arrhythmias. It’s a minimally invasive procedure where a cardiac electrophysiologist can go inside the heart to create a live, three-dimensional electrical map. Forget the snapshots; this is like sending a team of highly specialized technicians directly to the circuit board to test every single wire and connection in real time.
During an EP study, the specialist gently guides several thin, flexible wires called catheters—each with sensors on its tip—through a blood vessel in your groin and up into your heart. These catheters are remarkable; they can both record the heart’s natural electrical signals and deliver tiny, controlled electrical pulses.
By doing this, the electrophysiologist can safely trigger the problematic arrhythmia under completely controlled conditions. This allows them to see exactly where the faulty signal is coming from and the precise path it takes through the heart.
An EP study isn’t just about finding the problem—it’s about recreating it in a safe environment to understand its exact mechanism. This detailed map is the key that unlocks the most effective treatment, which can often be delivered in the very same session.
What to Expect During the Procedure
The idea of a procedure involving your heart can sound intimidating, but an EP study is designed with your comfort and safety as the top priorities. You’ll receive a sedative to help you relax, though you’ll likely be awake enough to follow simple instructions. The specialist numbs the area where the catheters are inserted with a local anesthetic, so you shouldn’t feel pain there.
You might feel your heart beat faster or stronger when the arrhythmia is induced, but this is a normal and expected part of the test. The medical team is in complete control and can stop it at any moment. The entire study typically lasts between one and four hours.
This procedure has become a cornerstone of modern heart care. Globally, the infrastructure is growing, with a median of 3.3 hospitals per million people now performing these highly specialized studies. Pacemakers, a related technology, are even more common, with implantation rates hitting 739 per million people, showing just how impactful these rhythm-correcting technologies have become. To see the data for yourself, you can learn more about the worldwide state of arrhythmia care.
Ultimately, the goal of these diagnostic tests—from a simple ECG to a detailed EP study—is to move from uncertainty to clarity. By meticulously mapping your heart’s electrical network, your specialist can create a precise, effective strategy to restore its natural rhythm and give you back your quality of life.
Modern Treatments to Restore Heart Rhythm
Once a cardiac electrophysiologist has a precise electrical map of your heart, the next step is to correct the faulty wiring. The goal isn’t a temporary patch; it’s about restoring a stable, healthy rhythm with advanced treatments designed to provide a lasting solution, improving both your safety and your quality of life.

The strategy can range from medications that manage symptoms to minimally invasive procedures that offer a potential cure. Your specialist will walk you through the best approach based on the type of arrhythmia you have, your symptoms, and your overall health.
Medications as a First Line of Defense
For many people, the first step in managing an arrhythmia is medication. These drugs don’t fix the electrical short circuit itself, but they can effectively control its effects, making the heart less susceptible to those erratic signals.
Think of it like adding insulation to a faulty wire to prevent dangerous sparks. Common medications include:
- Beta-blockers: These drugs slow the heart rate, reducing the workload on the heart and preventing episodes of tachycardia.
- Calcium channel blockers: Similar to beta-blockers, these help rein in a rapid heart rate by moderating the electrical signals.
- Antiarrhythmic drugs: This class of medication works directly on the heart’s electrical properties to maintain a normal sinus rhythm.
While effective, medications often require lifelong use and can come with side effects. For a more definitive solution, specialists often turn to procedural interventions.
Catheter Ablation: The Precision Fix
When medication isn’t enough, or when a permanent fix is the goal, catheter ablation is the gold standard. This minimally invasive procedure is a cornerstone of modern cardiac electrophysiology, designed to eliminate the exact cluster of heart cells causing the trouble.
If the EP study is the diagnostic mapping mission, ablation is the targeted repair that often follows right away. Using the same catheter technology, the electrophysiologist navigates to the precise location of the faulty circuit. Once there, they deliver a focused beam of energy—either heat (radiofrequency) or cold (cryoablation)—to create a tiny, targeted scar.
This scar is strategically placed to act as an electrical barrier. It permanently blocks the abnormal signal from spreading, effectively silencing the source of the arrhythmia without damaging the surrounding healthy tissue. It’s the ultimate precision strike against a rogue electrical pathway.
Incredible technological advancements have made this procedure highly effective, especially for common conditions like Atrial Fibrillation. In fact, the market for electrophysiology ablation is projected to grow from $3.6 billion to an impressive $9.06 billion by 2035—a clear sign of its success and the rising demand for minimally invasive solutions. You can discover more insights about the electrophysiology market growth on futuremarketinsights.com.
Implantable Devices: The Heart’s Safety Net
For some arrhythmias, particularly those that are dangerously slow or life-threateningly fast, the best solution is an implantable device that acts as a constant guardian for your heart’s rhythm. These small, sophisticated devices are placed just under the skin of the chest during a minor surgical procedure.
There are two main types:
- Pacemakers: A pacemaker is the definitive treatment for bradycardia, a dangerously slow heart rate. Think of it as a smart, on-demand backup generator. It constantly monitors your heart’s rhythm and, if it detects a beat that’s too slow or a pause that’s too long, it sends a tiny, painless electrical impulse to get the heart back on track.
- Implantable Cardioverter-Defibrillators (ICDs): An ICD is a more advanced device designed to protect against life-threateningly fast heart rhythms like ventricular tachycardia. It functions like a pacemaker for slow rhythms but also has a critical, life-saving capability: if it detects a dangerously rapid, chaotic rhythm, it can deliver a controlled electrical shock to instantly reset the heart and restore a normal beat. An ICD is your personal, 24/7 emergency response team.
From carefully selected medications to pinpoint ablation and intelligent implantable devices, the field of cardiac electrophysiology offers a powerful array of tools. These treatments are designed not just to manage symptoms but to restore the heart’s natural harmony, allowing you to return to your life with confidence and peace of mind.
When to Consult a Cardiac Electrophysiologist
Knowing when to see a specialist can feel overwhelming. While your general cardiologist is the expert on your heart’s overall plumbing—its arteries, valves, and muscle function—a cardiac electrophysiologist (EP) is the definitive expert for its intricate wiring. Think of them as the master electricians of the heart.
If you’re experiencing recurring or unexplained symptoms tied to your heart’s rhythm, it’s likely time to seek a referral. An EP has completed years of extra fellowship training focused solely on diagnosing and treating these electrical disturbances. It’s a crucial distinction that can make all the difference in getting to the root of the problem.
Red Flags That Warrant an EP Consultation
Certain symptoms are clear signals that your heart’s electrical system needs an expert evaluation. Consider these the non-negotiable red flags that should prompt a conversation with your doctor about seeing an electrophysiologist.
Key warning signs include:
- Recurring Palpitations: A persistent feeling of a fluttering, pounding, or racing heart that comes and goes without a clear cause.
- Unexplained Fainting (Syncope): Losing consciousness, even for just a moment, can indicate a serious arrhythmia is preventing adequate blood flow to the brain. This is never normal.
- Dizziness or Lightheadedness: Frequent episodes of feeling unsteady or on the verge of fainting, especially when not tied to obvious triggers like dehydration or standing up too quickly.
- Diagnosed Arrhythmias: If you’ve already been diagnosed with a condition like Atrial Fibrillation (AFib) or Supraventricular Tachycardia (SVT), an EP can offer advanced, definitive treatment options that go far beyond initial medications.
A significant family history of heart rhythm problems or, tragically, sudden cardiac death is another compelling reason to consult an EP for a proactive evaluation. Don’t wait for symptoms to appear.
It’s important to understand the roles here: while a general cardiologist can identify an arrhythmia, a cardiac electrophysiologist is the specialist who can perform an EP study to precisely map its origin and deliver targeted treatments like catheter ablation.
Advocating for Your Heart Health
Navigating the healthcare system is much easier when you know exactly what to ask for. If your symptoms persist despite initial treatment from your primary care doctor or even a general cardiologist, don’t hesitate to be direct. Specifically asking for a referral to a cardiac electrophysiologist is a powerful, proactive step.
This ensures you get access to the most advanced diagnostic tools and therapies available. Making informed decisions is your right, and finding the right specialist is a huge part of that process. For those seeking the highest level of care, exploring the best hospital for heart surgery options can provide valuable insight into where the leading experts practice. Taking control of your health journey is the only way to ensure you receive the specialized attention your heart’s electrical system truly deserves.
Common Questions About Electrophysiology
Stepping into the world of cardiac electrophysiology naturally brings up questions. Getting clear, straightforward answers is the best way to feel confident and prepared for your care. Here are some of the most common things patients ask before a procedure.
Is an Electrophysiology Study Painful?
No, the entire process is designed for your comfort. You’ll receive a sedative to help you relax, and a local anesthetic will completely numb the area where the catheters are inserted. You shouldn’t feel any pain there.
What you might notice is your heart beating faster or stronger for a moment when the specialist tests the arrhythmia. This is a normal, controlled part of the study. Your team is right there with you and can provide more medication if you feel any discomfort at all.
How Long Is the Recovery After Catheter Ablation?
Recovery is usually quite fast. Most people are back to light, normal activities within just a day or two.
The key is to let the insertion site heal properly. Your doctor will ask you to avoid any strenuous exercise or heavy lifting for about one week. Following their specific instructions is the fastest way to ensure a smooth recovery.
What Are the Risks of an EP Procedure?
Every medical procedure has some degree of risk, but EP studies and ablations are considered very safe. The most common issues are minor and related to the catheter insertion site—things like bleeding, bruising, or a small infection.
Serious complications, like damage to a blood vessel or the heart’s natural electrical system, are rare. Your specialist will walk you through all the potential risks beforehand. Full transparency is essential so you can make a decision that feels right for you. When it’s time to choose a specialist, you can find a doctor in our curated network to connect with trusted, top-tier professionals.
At Haute MD, we connect you with the nation’s leading medical experts who specialize in advanced, patient-focused care. Find a rigorously vetted physician who can provide the clarity and expertise you deserve by exploring our network today at https://www.hauteliving.com/hautemd.

