When you hear the terms bioidentical hormones vs synthetic hormones, the conversation really boils down to one thing: molecular structure. It’s a simple but profound difference. Bioidentical hormones are engineered to be exact replicas of the hormones your body produces naturally, down to the last molecule. Non-bioidentical synthetic hormones are not.
That single distinction is the starting point for understanding how each one works inside your body.
Understanding Your Hormone Therapy Options
Hormone therapy is all about restoring balance. As we age, declining hormone levels—often linked to menopause in women or andropause in men—can bring a wave of unwelcome symptoms. Navigating your treatment options means getting familiar with the language, and the debate usually centers on two main types of hormones, each with a unique chemical design and origin story.
This isn’t a niche conversation anymore. The global market for bioidentical hormones was valued at around USD 4.06 billion and is expected to climb to USD 6.77 billion by 2032. This growth is fueled by patients actively seeking out these therapies and the rising prevalence of hormonal disorders that need effective management.
Bioidentical vs Synthetic Hormones At A Glance
To get our bearings, a side-by-side comparison is the best place to start. The core difference is their chemical blueprint, which dictates how they interact with your body’s hormone receptors. From there, you’ll see other key distinctions emerge, from their source materials to how they’re regulated.
Having this foundational knowledge is critical. Our comprehensive bioidentical hormone replacement therapy guide explores the treatment protocols in much greater detail.
The table below offers a high-level summary to frame your understanding before we dive deeper into the nuances of each approach.
| Attribute | Bioidentical Hormones | Synthetic Hormones (Non-Bioidentical) |
|---|---|---|
| Molecular Structure | Chemically identical to human hormones (e.g., estradiol, progesterone). | Chemically altered structure; similar but not identical to human hormones (e.g., conjugated equine estrogens, medroxyprogesterone acetate). |
| Primary Source | Derived from plant sources like wild yams and soy, then synthesized to be bioidentical. | Can be entirely lab-created or derived from non-human sources, such as pregnant mare urine (Premarin). |
| FDA Approval Status | Many are available as standardized, FDA-approved manufactured products. Also available as custom-compounded formulas, which are not FDA-approved. | Widely available as standardized, FDA-approved manufactured products with consistent, fixed dosages. |
| Customization | Compounded versions can be highly customized in dosage and delivery method based on individual needs. | Available in standardized, pre-set dosages determined by the manufacturer, offering less flexibility. |
Think of this table as your starting point. It captures the essential differences, but the real story is in how these attributes play out in a clinical setting and affect patient outcomes.
How Molecular Differences Impact Your Body
To really get to the heart of the bioidentical hormones vs synthetic hormones debate, you have to look past their origins and get down to the molecular level. This is where the most critical distinctions are found. The easiest way to think about it is to picture your body’s hormone receptors as highly specific locks; only a key with the perfect shape can fit and trigger the correct biological signal.
Bioidentical hormones are engineered to be that perfect key. Their molecular structure is an exact copy of the hormones your body produces naturally, like estradiol or progesterone. Because your body recognizes them as its own, they bind smoothly to the right receptors and do their job just as intended.
On the other hand, non-bioidentical synthetic hormones are designed with a slightly different molecular architecture. They are similar enough to interact with hormone receptors, but they aren’t a perfect match. This structural tweak is intentional—it’s what allows a pharmaceutical company to patent the molecule—but it can absolutely change how the hormone behaves once it’s in your system.
Receptor Binding And Biological Response
The precision of that hormone-receptor connection is everything. A perfectly fitting bioidentical hormone initiates a predictable, natural cascade of cellular signals. An imperfectly fitting synthetic hormone might activate that same receptor differently—sometimes stronger, sometimes weaker, and sometimes triggering a slightly different biological effect altogether.
Let’s look at a common clinical example with estrogens:
- Bioidentical Estradiol: This is the same molecule your ovaries produce. It docks with estrogen receptors in a familiar way, kicking off the standard physiological processes we associate with estrogen.
- Synthetic Ethinyl Estradiol: This is the workhorse of most birth control pills. Its structure is modified to make it more potent and to resist breakdown by the liver. While this change makes it effective orally, it also alters its interaction with receptors throughout the body.
The difference between progesterone and progestins is another classic example.
Bioidentical progesterone supports the uterine lining and often has calming, neuroprotective effects. Synthetic progestins, like medroxyprogesterone acetate (MPA), can have very different side-effect profiles because they don’t just bind to progesterone receptors; they cross-react with other hormone receptors, too.
This difference in receptor interaction and specificity is a fundamental reason why patients might experience completely different outcomes or side effects when comparing bioidentical versus synthetic options.
How Your Body Breaks Down Hormones
Metabolism—how your body processes and eliminates hormones—is the other side of the molecular coin. Your body has evolved specific enzymatic pathways designed to break down the hormones it produces naturally. Since bioidentical hormones are molecularly identical, they get processed through these same well-worn pathways.
This means they break down into metabolites that the body already knows how to handle and excrete. The whole process is generally efficient and predictable because it’s just mirroring normal physiology.
Synthetic hormones, with their altered structures, force the body to use different or modified enzymatic pathways for metabolism. This can lead to the creation of metabolites—byproducts that aren’t normally found in the body.
The clinical significance of these unique metabolites is a major topic of ongoing research and debate. Some evidence suggests these foreign byproducts could be responsible for some of the unwanted side effects linked to certain synthetic hormones. The takeaway is simple: molecular structure dictates not just how a hormone acts, but also how it leaves the body, which can have significant downstream health implications.
The Clinical Evidence on Safety and Efficacy: What the Science Really Says
When you strip away the marketing, the core question is simple: does the clinical evidence show that one type of hormone is definitively safer or more effective than the other? While it’s tempting to assume “bioidentical” means better, a hard look at the data reveals a far more complex reality.
The entire conversation around hormone safety was upended by the Women’s Health Initiative (WHI), a massive study launched in the early 1990s. Its initial findings, published in 2002, sent shockwaves through the medical community. The study linked a specific combination of synthetic hormones—conjugated equine estrogens (CEE) and medroxyprogesterone acetate (MPA)—to a higher risk of breast cancer, heart disease, stroke, and blood clots.
This landmark report triggered a major exodus from hormone therapy. But as researchers dug deeper into the WHI data, a more nuanced picture emerged. They realized many of the risks were primarily tied to the synthetic progestin (MPA) and its combination with oral estrogens. This crucial distinction cracked open the door for a serious investigation into whether different hormone formulations might carry entirely different risk profiles.
Evaluating Efficacy for Symptom Relief
When it comes to the primary job of hormone therapy—relieving miserable symptoms like hot flashes, night sweats, and vaginal dryness—the evidence is pretty straightforward. Both FDA-approved bioidentical hormones and conventional synthetic hormones work incredibly well.
Time and again, clinical trials have confirmed that standard doses of both types of estrogen therapy dramatically cut down the frequency and intensity of vasomotor symptoms. From a pure efficacy standpoint, there’s no strong scientific evidence proving one is superior for symptom control. The best choice often boils down to how an individual patient responds and which side effects they experience.
The goal of modern hormone therapy is to use the lowest effective dose for the shortest time needed to manage your symptoms. Both FDA-approved bioidentical and synthetic hormones can achieve this perfectly when managed by a skilled physician.
The Safety Debate and Where We Stand Now
The heart of the safety argument is whether the molecular structure of bioidentical hormones truly leads to a better long-term risk profile, especially for cardiovascular health and cancer. Proponents argue that since these hormones are identical to what your body makes, they should be safer. It’s a logical theory, but it demands proof from robust clinical trials.
A key battleground in this debate is the difference between bioidentical progesterone and synthetic progestins. Some studies do suggest that bioidentical progesterone might be kinder to cardiovascular markers and have a less stimulating effect on breast tissue compared to synthetics like MPA. Still, these findings aren’t definitive enough to declare all compounded bioidentical therapies universally safer.
Major medical organizations have weighed in, and the consensus is clear. The available body of evidence does not prove that custom-compounded bioidentical hormones are safer or more effective than their FDA-approved counterparts. You can dig into a detailed analysis of the evidence from reputable sources like the Mayo Clinic’s discussion on bioidentical hormone safety.
This consensus drives home a critical point: words like “natural” and “bioidentical” don’t automatically mean “safer.” The safety of any hormone therapy hinges on several factors:
- The specific hormone used (e.g., bioidentical progesterone vs. a synthetic progestin).
- The route of administration (a transdermal patch carries different risks than an oral pill).
- The patient’s individual health profile and unique risk factors.
- Proper dosing and consistent monitoring.
Ultimately, the surest path to safety is using FDA-approved products, whether they are bioidentical or synthetic. These formulations have been through the wringer—rigorously tested for purity, consistent dosing, and proven effectiveness. While the theoretical appeal of bioidentical hormones is strong, any decision has to be grounded in the scientific evidence we have today, combined with a personalized risk-benefit analysis you conduct with your doctor.
Navigating Regulation And Quality Control
Knowing the molecular structure of a hormone is one thing; understanding where it comes from is another matter entirely. The regulatory environment is a critical factor in the bioidentical hormones vs. synthetic hormones debate, and it directly impacts your safety and the consistency of your treatment. This landscape is split into two distinct worlds: products meticulously vetted and approved by the Food and Drug Administration (FDA), and custom preparations made in compounding pharmacies.
FDA-approved hormones, whether they’re bioidentical or synthetic, have to clear an incredibly high bar. Before a manufacturer can market an estradiol patch or a progesterone capsule, they must submit exhaustive clinical trial data proving the product is both safe and effective for its intended use.
But the scrutiny doesn’t stop once it’s on the market. The FDA also enforces rigid manufacturing standards, known as Good Manufacturing Practices (GMP), to guarantee that every single dose is pure, stable, and contains the exact amount of active ingredient stated on the label. This is your assurance that your body receives a consistent, predictable dose every single time.
The World Of Compounded Hormones
Compounding pharmacies play by a different set of rules. These specialized pharmacies create custom-mixed hormone formulations tailored to an individual patient’s prescription. This is an indispensable service for patients with specific needs, like an allergy to a dye in a commercial product or the need for a dosage that simply isn’t available off the shelf.
However, and this is a crucial distinction, these custom-mixed preparations are not individually FDA-approved. While the pharmacies themselves are licensed and regulated by state boards of pharmacy, the specific hormone creams, gels, or lozenges they create don’t undergo the same rigorous, large-scale clinical trials required for mass-marketed drugs.
This creates a significant gap in oversight. As the National Academies of Sciences, Engineering, and Medicine has pointed out, compounded bioidentical hormone therapy (cBHT) isn’t held to the same safety and efficacy testing standards. Compounding pharmacies aren’t required to report adverse side effects to the FDA or provide the detailed patient information leaflets that come with approved drugs. This lack of oversight can lead to inconsistencies in quality and safety, sometimes fueling a mistaken belief that compounded hormones are inherently “safer” when, in reality, your physician may not have complete data on their potential side effects. You can dig deeper into the market dynamics and regulatory status of bioidentical hormones to understand the landscape more fully.
The fundamental difference comes down to pre-market approval. FDA-approved products are tested for safety and efficacy before they ever reach a patient. Compounded formulas are mixed for individuals without any prior large-scale clinical validation of that specific mixture.
This isn’t a minor detail; it’s central to understanding the risk-benefit equation. Without FDA oversight on the final product, the potential for variability in potency and purity from one batch to the next is a real concern.
Regulatory and Quality Comparison
To make a truly informed decision, it helps to see the oversight differences side-by-side. The level of scrutiny applied to a product directly correlates to the quality control you can expect. Let’s break down what this means for your treatment.
| Oversight Factor | FDA-Approved Hormones (Bioidentical & Synthetic) | Compounded Bioidentical Hormones (cBHT) |
|---|---|---|
| Safety & Efficacy Testing | Must be proven through extensive clinical trials before marketing. | The specific formula is not tested for safety or efficacy. |
| Dosing Consistency | Guaranteed through strict manufacturing standards; each dose is precise. | Potential for variability between batches; consistency is not guaranteed. |
| Purity & Contaminants | Rigorously tested to ensure purity and freedom from contaminants. | Relies on the compounding pharmacy’s internal quality control standards. |
| Adverse Event Reporting | Manufacturers are legally required to report adverse events to the FDA. | Reporting is not mandatory, leading to incomplete safety data. |
| Patient Information | Must include a detailed package insert outlining risks and benefits. | Often lacks the standardized, comprehensive patient information leaflet. |
Ultimately, choosing between an FDA-approved product and a compounded preparation is a decision about balancing personalization with certainty. While compounding offers valuable flexibility for specific patient needs, FDA-approved therapies provide a guarantee of consistency and a safety profile backed by extensive scientific evidence and regulatory review. This is a crucial conversation to have with your physician.
Choosing The Right Hormone Therapy For You
The debate over bioidentical hormones vs synthetic hormones ultimately moves from the clinic to your real life. There’s no single “best” choice here. The right therapy is the one that fits your unique medical history, personal comfort level, and specific health goals—a decision you and your physician make together.
The entire process should start with a deep dive into your health history. Certain conditions, like a personal history of blood clots, breast cancer, or liver disease, will immediately steer the conversation. For example, a transdermal patch bypasses the liver, making it a potentially safer route for some women than oral hormones.
Patient Scenarios And Personalized Decisions
To see how this plays out in the real world, let’s walk through a few common scenarios. Each one shows how different factors can lead to different, but equally correct, treatment decisions.
- Scenario 1: The Patient with a Specific Allergy A 52-year-old woman is struggling with severe menopausal symptoms. Her doctor suggests an FDA-approved bioidentical progesterone capsule, a standard and effective option. But there’s a catch: she has a severe peanut allergy, and many commercial progesterone capsules use peanut oil as a filler. The solution? A custom-compounded progesterone from a specialty pharmacy, formulated with an alternative oil, becomes the only safe and appropriate path forward.
- Scenario 2: The Patient Prioritizing Consistency A 48-year-old executive is dealing with disruptive hot flashes and brain fog that are impacting his work. For him, consistency and reliability are paramount. He chooses an FDA-approved bioidentical estradiol patch and oral progesterone. He’s reassured by the rigorous quality control and predictable dosing that come with manufactured pharmaceuticals, giving him the peace of mind that his therapy will be stable and effective.
- Scenario 3: The Patient Needing a Unique Dose A 65-year-old man needs testosterone therapy, but he finds that standard commercial gel dosages are too potent, leading to unwanted side effects. After careful evaluation, his physician prescribes a lower-strength compounded testosterone cream. This allows for precise micro-dosing that simply isn’t available in mass-produced options, giving him symptom relief without the adverse effects.
These examples make it clear: the choice is rarely about one hormone type being inherently superior. It’s about what is most suitable for an individual’s specific clinical picture. For a deeper look at how these therapies fit into a comprehensive wellness plan, you can explore the principles of hormone optimization for longevity.
Navigating The Decision With Your Doctor
A productive conversation with your doctor is the foundation of a successful treatment plan. It isn’t just about reciting symptoms; it’s about discussing your lifestyle, your risk tolerance, and what you truly hope to achieve with hormone therapy.
The most important part of choosing a hormone therapy is the shared decision-making process. Your provider brings the medical expertise, and you bring the knowledge of your own body and life priorities. The right choice lies where those two perspectives meet.
This flowchart helps visualize that initial fork in the road, showing how your journey can lead to either an FDA-approved product or a custom-compounded solution.
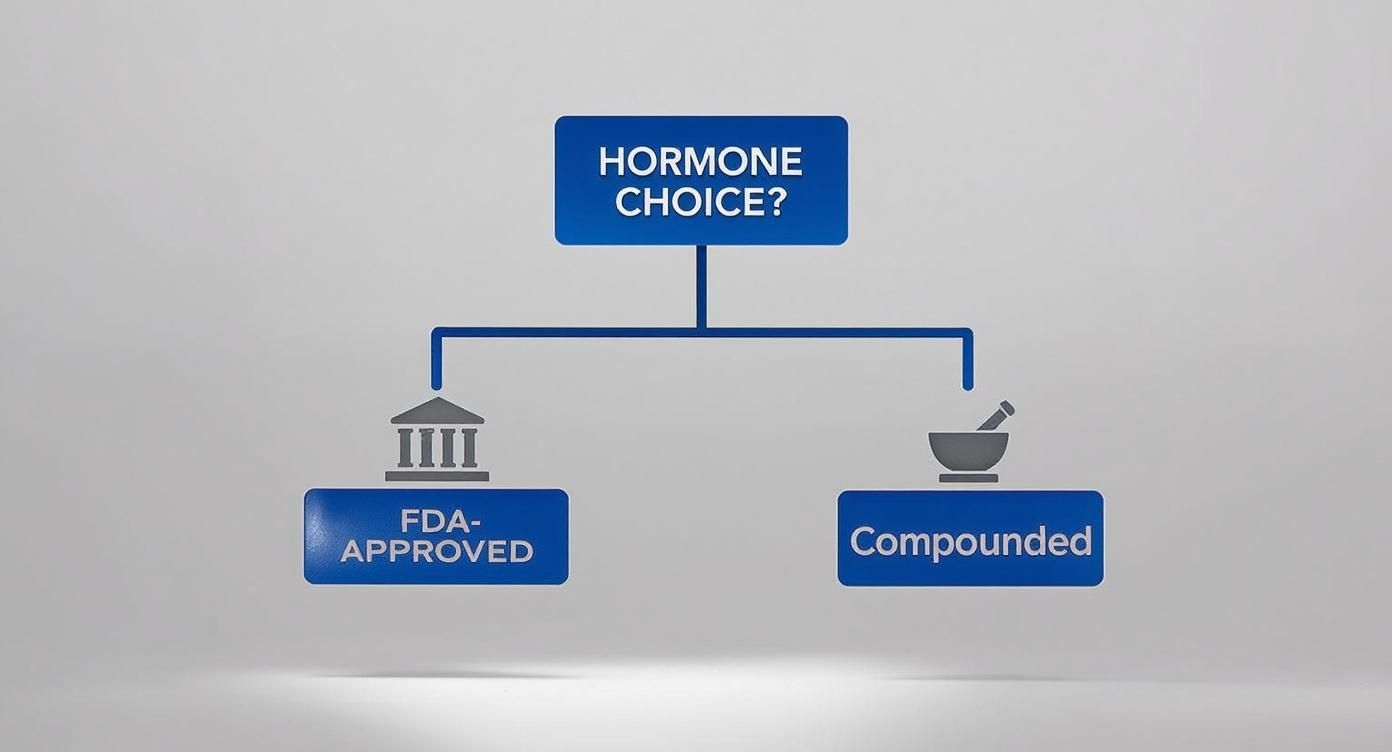
As you can see, the path always starts with your unique needs. From there, it branches toward either regulated, standardized options or personalized, compounded ones, depending on your specific clinical requirements.
Ultimately, whether you land on an FDA-approved bioidentical, a conventional synthetic, or a custom-compounded formula, the decision must be informed, intentional, and revisited over time. Your hormonal needs will change, and your therapy has to adapt right along with them, always guided by a thorough risk-benefit analysis and transparent communication with your physician.
Considering The Practical Details Of Treatment
Beyond the molecular science, the day-to-day experience of hormone therapy is what really matters. When we compare bioidentical hormones vs synthetic hormones, it’s critical to look at how treatment is delivered, how progress is monitored, and what the financial reality looks like for each path. These real-world factors often make or break long-term success and a patient’s willingness to stick with it.

FDA-approved therapies—both bioidentical and synthetic—are straightforward. They usually come in standardized forms like patches, pills, and gels. This standardization is great for dose consistency, but it doesn’t leave much room for adjustment. On the other hand, compounded bioidentical hormones are highly customizable, available as creams, troches (lozenges), or capsules mixed to a doctor’s exact specifications.
Monitoring Progress And Ensuring Safety
No matter which type of hormone you use, diligent monitoring is non-negotiable. This process isn’t just about feeling better; it’s a critical safety measure to ensure you’re on the lowest effective dose that still achieves your goals.
Best practices for monitoring are quite clear:
- Symptom Tracking: Keeping a detailed log of your symptoms and how they respond to treatment provides invaluable real-world data for both you and your physician.
- Regular Lab Work: Blood tests are the gold standard for tracking hormone levels and making sure they stay within a safe, therapeutic range. Saliva testing, despite its popularity in some circles, is not considered a reliable diagnostic method by major medical organizations.
- Annual Health Screenings: This includes mammograms and pelvic exams for women, which remain absolutely essential for monitoring overall health while on any form of hormone therapy.
This continuous feedback loop helps us fine-tune your treatment over time. For men, understanding all the available methods is crucial, and it’s worth exploring the nuances of various testosterone replacement therapy options.
A key differentiator in practice is that while FDA-approved drugs have well-established dosing guidelines, compounded therapies rely heavily on the practitioner’s expertise and consistent lab monitoring to validate safety and efficacy.
Analyzing Cost And Insurance Coverage
Let’s talk about the financial side—it’s a significant and practical part of the equation. FDA-approved hormone therapies, whether bioidentical or synthetic, are widely covered by most insurance plans. This makes them a more accessible and affordable option for many patients.
In contrast, custom-compounded bioidentical hormones are rarely covered by insurance. This means patients typically shoulder the full cost, which can be substantial and ongoing. The price includes not only the custom-made medication but often more frequent consultations and specialized lab testing, all leading to significantly higher out-of-pocket expenses. This financial reality is a critical factor to weigh when deciding on the most sustainable treatment path for your long-term health.
Answering Your Key Questions
When you’re navigating the world of hormone therapy, a few questions always seem to surface. Misconceptions are common, and getting clear, evidence-based answers is critical before making any decisions about your health.
Let’s cut through the noise and tackle some of the most frequent questions about bioidentical vs. synthetic hormones.
Are ‘Natural’ Hormones A Safer Choice?
The word “natural” is one of the most misused terms in medicine. While many bioidentical hormones are synthesized from plant sources like soy or yams, they still undergo extensive processing in a lab to become molecularly identical to the hormones in your body. They don’t come straight from a plant into a pill.
The key factor for safety isn’t the origin—it’s the final chemical structure and, most importantly, whether the final product has been through the fire of FDA testing for purity, potency, and consistent dosing.
Major medical organizations, including The Endocrine Society, are clear on this: there is no credible scientific evidence showing that custom-compounded bioidentical hormones are safer or more effective than their FDA-approved counterparts. Safety comes from regulation and rigorous testing, not a marketing label.
The crucial takeaway is that “natural” does not automatically mean “safer.” The most reliable indicator of safety is FDA approval, which guarantees a product has been thoroughly evaluated for risks and benefits based on extensive clinical data.
Why Would A Doctor Recommend Compounded Hormones?
So why would a well-qualified physician ever opt for a compounded bioidentical hormone therapy (cBHT)? The legitimate clinical reasons are actually quite narrow.
The most common one is a documented allergy to an inactive ingredient in a commercially available, FDA-approved product. Think dyes, fillers, or preservatives. If a patient reacts to something in the standard formulation, compounding can create a version without that specific allergen.
Another scenario might involve the need for a very specific dose or delivery system that isn’t mass-produced—for instance, a micro-dose that falls outside the standard manufactured options. But this is a rare case, and it always requires a serious conversation about the trade-offs. You’re weighing the potential benefit of customization against the known risks of using products that lack FDA oversight and guaranteed dose-to-dose consistency.
Is Saliva Testing Reliable For Hormone Therapy?
Despite being heavily promoted by some anti-aging clinics, saliva testing is not considered a reliable or accurate tool for guiding hormone therapy. Mainstream medical bodies, including The Endocrine Society, strongly advise against it.
Why? Hormone levels in your saliva can swing wildly throughout the day and simply don’t correlate well with the biologically active hormone levels in your blood and tissues, which is what actually matters.
Effective, safe hormone management is built on a combination of a thorough clinical evaluation of your symptoms and standardized blood testing. Treatment decisions should always be based on this complete picture, with the goal of using the lowest effective dose to get you feeling better and improve your quality of life.
Finding a physician who is a true expert in hormone optimization is the single most critical step in your wellness journey. Haute MD provides a curated network of the nation’s leading, board-certified specialists who are vetted for their commitment to evidence-based, patient-centered care. Connect with a top-tier hormone expert in your area by visiting Haute MD.

