Imagine your body has its own internal repair crew, a team of biological specialists ready to fix damage right at the source. At its heart, regenerative medicine is the science of harnessing and amplifying your body’s innate healing abilities to repair, replace, or even regrow damaged tissues and organs.
It’s a fundamental shift in thinking—moving away from just managing symptoms and toward addressing the root causes of disease and injury.
A New Perspective on Healing
Traditional medicine often focuses on treating the downstream effects of a problem. A pain reliever, for instance, might quiet the discomfort of an arthritic knee, but it does nothing to fix the worn-down cartilage causing the pain.
Regenerative medicine flips the script entirely. It asks a far more powerful question: What if we could help the body rebuild that cartilage itself? This approach uses the body’s own biological toolkit—its cells, signals, and structures—to restore function from the inside out.
This field represents a significant move toward more personalized and potentially curative treatments. Instead of always relying on external solutions like pills or surgery as the first line of defense, the goal is to empower the body to heal itself. This is why you’ll hear it discussed in contexts ranging from orthopedic injuries to advanced anti-aging strategies.
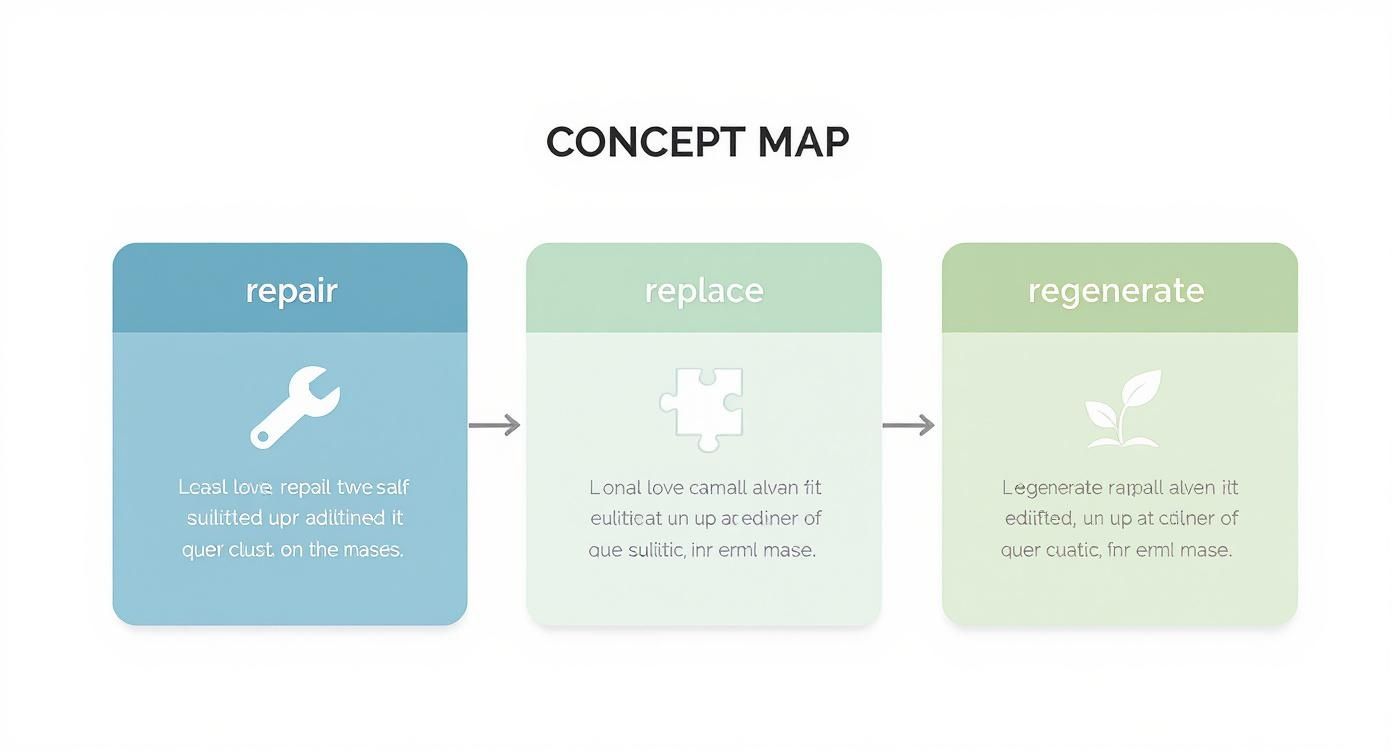
The Three Core Goals of Regenerative Medicine
The entire field can be broken down into three primary objectives. Each one represents a different level of intervention, from giving your body a simple boost to prompting it to build new tissues from scratch.
- Repair: This is about stimulating the body’s existing healing processes to mend injured tissue. Think of it as sending in reinforcements and better supplies to an existing construction crew.
- Replace: This goal focuses on swapping out damaged or diseased cells with new, healthy ones. It’s like replacing a faulty component in a high-performance engine to restore its original function.
- Regenerate: The most ambitious goal is to prompt the body to regrow entire parts of tissues or even organs, creating functional new structures where they were lost.
This growing interest isn’t just academic; it’s making a massive economic impact. Driven by urgent clinical needs and incredible new technologies, the market hit USD 7.02 billion in one recent year and is projected to skyrocket to USD 148.42 billion by 2033.
This explosive growth underscores the rapid adoption of cell therapies and tissue engineering in healthcare worldwide. You can explore more data on the regenerative medicine market growth on Straits Research.
To put it simply, regenerative medicine isn’t about putting a bandage on a problem. It’s about providing the raw materials and biological instructions for the body to fix the problem itself.
To clarify these concepts, let’s look at the core principles in a simple framework.
Core Principles of Regenerative Medicine at a Glance
This table breaks down the three primary goals, explaining what each one means and where you might see it applied.
| Principle | Explanation | Example Application |
|---|---|---|
| Repair | Stimulating the body’s natural healing mechanisms to mend injured or degraded tissue. | Using PRP injections to accelerate tendon or ligament healing. |
| Replace | Introducing new, healthy cells to take over the function of damaged or diseased cells. | Stem cell therapy for conditions like osteoarthritis or certain blood disorders. |
| Regenerate | Prompting the body to regrow functional tissues or parts of organs that have been lost or damaged. | Tissue engineering to grow new skin grafts for burn victims. |
These principles guide every therapy and treatment developed under the regenerative medicine umbrella, from the straightforward to the incredibly complex.
Key Takeaway: Regenerative medicine is not about masking symptoms. Its purpose is to leverage the body’s powerful, built-in healing systems to restore function at a cellular and tissue level, offering a proactive and restorative approach to health.
Exploring the Body’s Toolkit: The Therapies Driving Regeneration
To really get what regenerative medicine is all about, we have to look inside its biological toolkit. This isn’t about one magic bullet. Instead, think of it as a collection of powerful, distinct therapies, each designed to work with the body’s own healing systems in a very specific way.
Imagine you’re in a high-tech workshop. You wouldn’t use a sledgehammer to fix a Swiss watch, right? It’s the same idea here. Regenerative medicine deploys different “tools” for different jobs. Let’s break down the four main players you’ll hear about most often.
Stem Cell Therapy: The Master Builders
At the heart of many regenerative strategies are stem cells, your body’s foundational raw material. These are truly remarkable cells with two defining superpowers: they can divide to create more of themselves, and they can differentiate—or transform—into specialized cells like muscle, bone, or cartilage.
Think of a stem cell as a master key that can be cut to fit any lock in a building. When they’re introduced into a damaged area and get the right signals, they have the potential to become the exact type of cell needed for the repair job, replacing old or injured cells to bring function back online.
This is the core concept behind using stem cells for conditions like osteoarthritis, where the goal is to help form new cartilage, or in certain neurological disorders, where the hope is to replace damaged nerve cells.
Platelet-Rich Plasma (PRP): The Emergency Response Crew
If stem cells are the master builders, then Platelet-Rich Plasma (PRP) is the highly concentrated emergency response crew. Your blood has several components, including red cells, white cells, plasma, and platelets. Platelets are famous for clotting blood, but they also carry hundreds of incredibly powerful proteins called growth factors.
When you get a cut, platelets flood the area, stop the bleeding, and unleash these growth factors, which act as powerful signals to kickstart the healing cascade. PRP therapy simply takes this natural process and puts it on steroids.
A small sample of your own blood is drawn and spun in a centrifuge, which separates and concentrates the platelets. This “liquid gold” is then injected directly into an injured area—like a torn tendon or an arthritic joint—delivering a massive dose of healing signals right where the body needs them most.
It’s like sending a highly concentrated team of medics and construction foremen directly to an accident site to manage the crisis and direct the repair work.
Exosome Therapy: The Cellular Messengers
While stem cells are the workers and PRP provides the on-site signals, exosomes are the critical messengers that carry instructions from one cell to another. These aren’t cells themselves. They are tiny, nano-sized vesicles released by cells, especially stem cells.
Picture exosomes as microscopic delivery drones. They come packed with genetic information (mRNA and microRNA), proteins, and lipids from their parent cell. As they travel through the body and merge with other cells, they deliver this payload, essentially telling the recipient cells what to do.
They might instruct a sluggish cell to start repairing itself, tell an inflamed cell to calm down, or signal other cells to produce more collagen. Because they’re so small and carry such specific instructions, they are absolutely vital for cell-to-cell communication and coordinating the whole regenerative process. The body’s intricate immune system is central to this coordination, and you can explore this connection further in our guide on what an immunologist treats.
This infographic gives you a simple, at-a-glance summary of how these core principles work together.
As you can see, the goal is to leverage these tools to repair, replace, and ultimately regenerate tissue, restoring the body’s natural function from the inside out.
Tissue Engineering: The Biological Scaffolding
The final tool in the kit, tissue engineering, is the most construction-oriented of them all. This field combines cells, engineering principles, and biocompatible materials to actually build functional tissues. The key component here is often a scaffold.
Imagine trying to build a new wall without any framework. It would be a mess. A scaffold acts as a temporary, biocompatible structure that is implanted into the body. This structure has two crucial jobs:
- Provide a framework: It gives cells a physical place to attach and grow in the correct shape and orientation.
- Guide tissue formation: It can be infused with growth factors to encourage cells to form the exact tissue needed, like bone or cartilage.
Over time, as the patient’s own cells populate the scaffold and build new, healthy tissue, the scaffold itself safely dissolves, leaving only the newly generated tissue behind. We already see this in action for creating skin grafts for burn victims, and incredible research is underway to build far more complex organs.
How Regenerative Medicine Is Actually Changing Patient Lives

Understanding the science behind stem cells, PRP, and exosomes is one thing. Seeing how these tools are being put to work is where the real story unfolds. The true potential of regenerative medicine isn’t just in a lab—it’s in helping people move with less pain, feel more confident in their own skin, and even begin to tackle some of our most complex diseases.
This isn’t some far-off, futuristic concept. In clinics right now, these therapies are offering new solutions for problems that were historically managed with symptom-masking drugs or invasive surgery. Let’s look at the fields where regenerative approaches are making the biggest impact.
Rebuilding Mobility in Orthopedics
Orthopedics is arguably where regenerative medicine has made its most visible mark. Chronic joint pain from conditions like osteoarthritis affects millions, chipping away at their mobility and quality of life day by day. Instead of just managing the pain, regenerative therapies aim to address the root cause: the breakdown of cartilage and tissue.
For someone with a painful knee, this changes the entire conversation. We can now move beyond temporary fixes. Instead of relying solely on anti-inflammatory pills or steroid shots that wear off, a forward-thinking specialist might recommend:
- Platelet-Rich Plasma (PRP) Injections: This involves concentrating the healing growth factors from your own blood and injecting them directly into the joint. The goal is to quell inflammation and send a powerful signal to local cells to kickstart the repair process.
- Stem Cell Therapy: Here, the idea is to introduce potent “master builder” cells that can potentially develop into new cartilage, helping to patch up and rebuild the damaged joint surface from the inside out.
The objective isn’t just pain relief—it’s to slow down the disease, restore function, and help the body rebuild what’s been lost. For those dealing with this kind of chronic pain, connecting with the top doctors who treat arthritis is key, as these are the experts pioneering these advanced treatments.
Revitalizing Skin and Hair in Aesthetics
The world of aesthetics is also being completely reshaped by regenerative principles. The old model was about adding external products or fillers to temporarily change your appearance. The new focus is on stimulating your body’s own rejuvenation machinery at the cellular level.
This approach works by reactivating the natural biological engines that keep skin firm and hair follicles productive. It’s about cultivating healthier, more vibrant tissue from within.
A Real-World Example: Consider the “vampire facial.” It’s not just a gimmick. It combines microneedling with PRP. The tiny punctures from microneedling create a controlled injury that triggers a healing cascade, and the PRP supplies a super-dose of growth factors that tell your skin to ramp up collagen and elastin production. The result over time is genuinely firmer, smoother skin.
In the same way, PRP has become a go-to treatment for certain types of hair loss. By injecting it into the scalp, doctors can awaken dormant hair follicles and improve blood flow, encouraging the growth of new, healthier hair.
Charting New Frontiers in Complex Diseases
While orthopedics and aesthetics have the most established track record, the core ideas of regenerative medicine are pushing into some of the most difficult areas of health. Researchers are working tirelessly to see how these therapies could one day treat conditions affecting the heart, brain, and beyond.
- Cardiology: Scientists are exploring how stem cells might repair heart muscle scarred by a heart attack, which could improve cardiac function and prevent the slide into heart failure.
- Neurology: For devastating conditions like Parkinson’s or spinal cord injuries, the ultimate dream is to use stem cells to replace lost neurons or help repair damaged neural pathways.
- Fertility: Regenerative techniques are being studied to see if they can improve ovarian function or the health of the uterine lining, offering new hope for those struggling with fertility.
It’s important to be clear: many of these applications are still in clinical trials and aren’t standard care yet. But they represent the incredible promise of this field—a commitment to finding truly restorative solutions for conditions once thought to be permanent.
Common Applications of Regenerative Therapies
To make sense of which therapies are used where, it helps to see it all laid out. The table below gives a snapshot of the most common applications across different medical specialties.
| Medical Field | Common Condition | Primary Regenerative Therapy Used |
|---|---|---|
| Orthopedics | Osteoarthritis, Tendon Injuries, Ligament Sprains | Platelet-Rich Plasma (PRP), Stem Cell Therapy |
| Aesthetics | Skin Aging (Wrinkles, Laxity), Hair Loss | PRP Therapy, Microneedling with Growth Factors, Exosome Therapy |
| Cardiology | Heart Muscle Damage (Post-Heart Attack) | Stem Cell Therapy (Primarily Investigational) |
| Neurology | Spinal Cord Injury, Parkinson’s Disease, Stroke | Stem Cell Therapy, Exosome Therapy (Largely in Clinical Trial Stages) |
| Urology | Erectile Dysfunction | PRP Therapy, Shockwave Therapy |
This table underscores just how versatile regenerative medicine is. By matching the right biological “tool” to the specific needs of different tissues, physicians can create an environment that encourages genuine healing and functional recovery, changing the very definition of patient care.
Navigating Your Options: Safety and Regulations
The promise of regenerative medicine is undeniably exciting. But with that excitement comes a critical need for you, the patient, to be incredibly discerning. As money and interest flood into this space, the market is awash with information—and a dangerous amount of misinformation.
Learning to navigate this landscape is the single most important step you can take. You have to know the difference between a legitimate, evidence-based therapy and an unproven claim that might be ineffective at best and harmful at worst.
This isn’t just a minor issue. The field is expanding at a breakneck pace. Stem cell therapies alone recently made up nearly 43.8% of the entire regenerative medicine market, signaling massive clinical interest and investment. North America is currently the epicenter, thanks to our advanced healthcare infrastructure and research. You can get a deeper look at these trends from these regenerative medicine market insights from Future Market Insights. But rapid growth often outpaces regulation, creating a “Wild West” environment for patients.
Understanding The Regulatory Landscape
In the United States, the Food and Drug Administration (FDA) is the gatekeeper. Their job is to make sure any medical treatment hitting the market is both safe and effective. But the way regenerative therapies are regulated is complex, and shady clinics often exploit the gray areas.
It helps to break treatments down into three clear categories:
- FDA-Approved Therapies: These are the gold standard. They have survived years of rigorous, multi-phase clinical trials to prove they work for a specific condition. Very, very few regenerative therapies have cleared this high bar for widespread use.
- Investigational Therapies (Clinical Trials): These are treatments being formally studied in a controlled research setting. When you participate in a trial, you’re helping to gather the data needed to prove safety and effectiveness, but the outcome is not guaranteed.
- Unproven or Unregulated Therapies: This is the danger zone. These treatments are often marketed directly to consumers with big promises but have never been through the FDA gauntlet. Clinics offering them may make broad, unsubstantiated claims about curing everything under the sun.
Knowing which bucket a potential treatment falls into is non-negotiable for protecting your health and your wallet.
The Critical Role of Clinical Trials
Clinical trials are the absolute backbone of medical progress. They are how we find out if a brilliant idea in a lab actually helps people in the real world. Without them, we’re just guessing.
For a field as new as regenerative medicine, trials are everything. They’re the only way to separate what works from what’s just wishful thinking. While participating in a trial can give you access to innovative care, it’s crucial to remember that it’s still an experiment.
A legitimate clinical trial will always be registered on a public database like ClinicalTrials.gov. It will be overseen by an institutional review board (IRB) to protect your safety, and you will never be charged a fee to participate in the research itself.
How to Spot Red Flags and Unproven Claims
As you explore your options, you need to have your radar up. A reputable specialist will be upfront about the evidence, the risks, and what remains unknown. A questionable clinic, on the other hand, will rely on marketing hype and vague promises.
Be on high alert for any provider that:
- Promises a “Cure-All”: Real medicine is specific. Be deeply skeptical of any single treatment advertised to fix a laundry list of unrelated problems, from arthritis to Alzheimer’s.
- Uses Aggressive Advertising: Emotional testimonials and “miracle story” ads that sound too good to be true almost always are. Legitimate science is backed by data, not just anecdotes.
- Lacks Transparency: If they can’t clearly explain the science, show you data from studies, or give you a straight answer about risks and side effects, walk away.
- Charges for Unapproved Treatments: If a therapy isn’t FDA-approved or part of a formal, registered clinical trial, you have to ask why you’re being asked to pay thousands of dollars for an unproven experiment.
Your safety comes first. The goal isn’t just to understand the science of regenerative medicine; it’s to learn how to be an empowered and critical patient. By choosing providers who prioritize evidence over hype and operate with the highest ethical standards, you can navigate this incredible field with confidence.
Is Regenerative Medicine a Fit for You?
Understanding the science is one thing, but the next question is far more personal: Could one of these therapies actually work for you? The answer isn’t just about diagnosing a condition. It’s a deep dive into your unique health profile, a clear-eyed look at what these treatments can and cannot do, and an honest conversation about the financial investment.
Deciding to pursue regenerative medicine is a serious step. A qualified specialist won’t offer you a cookie-cutter solution. Instead, they’ll conduct a thorough evaluation to see if you’re a strong candidate, building a partnership based on transparency and realistic goals.
Who Is a Good Candidate?
Not everyone with joint pain or thinning hair is an ideal candidate for these therapies. A top-tier specialist will carefully assess several key factors before ever recommending a procedure. This isn’t about selling a treatment; it’s about ensuring the highest possible chance of a successful outcome based on your specific situation.
They’ll look closely at:
- Your Specific Condition and Its Severity: Early to moderate osteoarthritis, for example, often responds far better to PRP or stem cell therapy than advanced, bone-on-bone degeneration. The nature of the tissue damage is a critical starting point.
- Your Overall Health: Your body’s ability to heal is everything. Conditions like uncontrolled diabetes, active infections, or certain autoimmune diseases can interfere with the regenerative process and might make you a less suitable candidate.
- Previous Treatments and Surgeries: A specialist needs to know what you’ve already tried. If you’ve had multiple steroid injections or extensive surgery in the target area, it can change the biological environment and impact potential results.
- Lifestyle and Commitment: Your habits matter. Smoking, poor nutrition, or an inability to follow post-procedure rehabilitation protocols can completely undermine the success of a treatment. Your commitment to the healing process is a huge part of the equation.
The Bottom Line: A good candidate is someone whose medical condition aligns with what current evidence shows these therapies can help, and whose overall health provides a strong foundation for the body to do its repair work.
Setting Realistic Expectations
One of the most important conversations you’ll have with a specialist is about setting realistic expectations. Regenerative medicine is a powerful field, but it’s not a miracle cure. Dishonest clinics might promise to reverse aging or cure incurable diseases, but an ethical provider will ground the entire discussion in scientific reality.
Outcomes can vary dramatically from one person to the next. While one patient with knee arthritis might experience incredible pain relief and improved function, another with a nearly identical condition may only see modest improvement. The real goal is functional improvement and a better quality of life—not necessarily a complete reversal of your condition on an MRI.
The Financial Reality of Regenerative Medicine
Finally, you have to have a frank discussion about cost. Regenerative treatments are often expensive, with prices running from several thousand to tens of thousands of dollars, depending on the specific therapy and its complexity.
A major reason for this is that most insurance plans do not cover these procedures. Because many of these therapies are still considered investigational by insurers and the FDA, they are almost always paid for out-of-pocket. This financial reality has to be a central part of your decision. A reputable clinic will be completely transparent about all costs upfront, ensuring you can make an informed choice without any last-minute surprises.
How To Choose A Qualified Regenerative Specialist

This is, without a doubt, the most important decision you’ll make. The field of regenerative medicine is exploding, which has attracted a huge range of practitioners—some brilliant, others… not so much. Your job is to find a credible, experienced physician who puts patient safety and proven science above everything else.
Your health isn’t the place to cut corners. The provider you choose absolutely must be a board-certified physician in a relevant field, like orthopedics for joint pain or dermatology for skin issues. On top of that, they need specific, advanced training in the regenerative therapies they offer. This two-part qualification ensures they understand both your underlying condition and the science behind the treatment.
Vetting Your Physician
When you sit down for a consultation, it’s your time to interview them. Don’t be shy. Ask direct questions about their experience, where they source their biologics, and what evidence supports the specific protocol they’re recommending for you.
A truly trustworthy specialist will welcome these questions. They’ll have transparent, data-backed answers ready.
Key Takeaway: Run, don’t walk, from any clinic that promises a “cure-all” or uses high-pressure sales tactics. Ethical regenerative medicine is precise, personalized, and built on realistic outcomes—not exaggerated marketing hype.
Finding a doctor who meets this high bar can feel like searching for a needle in a haystack. This is where curated networks become invaluable. For instance, learning how to find top doctors near you through a vetted platform like Haute MD cuts through the noise. It connects you with pre-screened specialists who are known for their unwavering commitment to the highest standards of care, letting you move forward with genuine confidence.
Answering Your Questions About Regenerative Medicine
As you start to explore what regenerative medicine can do, it’s completely normal to have some practical questions. Let’s walk through the most common things patients ask, so you can move forward with a clear, confident understanding of the entire process.
How Long Does It Take To See Results?
This is probably the biggest point of confusion. Regenerative medicine isn’t like a steroid shot that masks pain for a few weeks. These therapies are designed to kickstart your body’s own, natural healing cascade, and that biological process simply takes time.
For something like a PRP or stem cell injection for an arthritic joint, you might feel some initial relief from inflammation within a few weeks. But the real magic—the actual tissue repair and rebuilding—happens over the long haul. Be prepared to wait three to six months, and sometimes longer, to appreciate the full benefit.
Patient Perspective: It’s best to think of regenerative therapy as planting a seed, not flipping a switch. The treatment gets things started, but the real growth happens gradually as your body takes over and does the heavy lifting.
Are Regenerative Procedures Painful?
Most patients are surprised by how well they tolerate these procedures. Since treatments like PRP or stem cell injections are minimally invasive, the discomfort is usually on par with a typical joint injection. We almost always use a local anesthetic to numb the area completely, making the procedure itself very manageable.
Afterward, it’s normal to have some soreness, swelling, or an aching sensation at the injection site for a few days. This is actually a good sign—it means your body is mounting the inflammatory response that signals the start of healing. Your physician will give you a clear plan to manage any post-procedure discomfort.
Why Doesn’t My Insurance Cover This?
This is the critical financial question, and the answer is straightforward. Most insurance carriers won’t cover regenerative therapies because the FDA still classifies many of them as investigational or experimental. Insurers need to see massive, multi-year clinical trials proving a treatment is the “standard of care” before they’ll agree to pay for it.
Because the field is still advancing so quickly, a lot of these cutting-edge treatments haven’t cleared that incredibly high bar for reimbursement yet. This means you should plan for these procedures to be an out-of-pocket investment. An open, transparent conversation with your doctor about the costs is an essential first step.
Finding a specialist who can answer your unique questions with honesty and expertise is the most important step. The Haute MD network is a premier resource, connecting discerning patients with the nation’s leading, board-certified physicians who are committed to evidence-based regenerative care. Find a trusted expert near you.

