When most people hear the word ‘neurosurgeon,’ their minds immediately jump to complex, high-stakes brain surgery. While that’s certainly a critical part of the job, it’s only a fraction of the full picture. These highly specialized doctors diagnose and surgically treat conditions affecting the entire nervous system—the brain, the spinal cord, and the vast network of nerves running throughout your body.
What Does a Neurosurgeon Treat?
A neurosurgeon is the specialist you turn to when a problem in the nervous system might require a surgical solution. Think of them as master technicians for the body’s most intricate and essential communication network.
While a neurologist diagnoses and manages conditions with medication and other therapies, a neurosurgeon steps in when a structural problem needs a physical fix. Their work is incredibly broad, covering everything from emergency trauma care to resolving chronic, debilitating pain.

At its core, their job is about solving physical problems that disrupt the nervous system. These issues often fall into a few key categories:
- Structural Abnormalities: This could be a herniated disc in the spine pressing on a nerve root or a tumor growing within the brain.
- Traumatic Injuries: They are on the front lines of treating damage to the head or spine from a serious accident.
- Vascular Problems: Think of an aneurysm, which is a weak, bulging spot on a blood vessel in the brain that poses a risk of rupture.
- Nerve Compression: A classic example is carpal tunnel syndrome, where a major nerve in the wrist gets pinched, causing pain and numbness.
The Scope of Neurosurgical Care
A neurosurgeon’s expertise isn’t confined to a single area. Their practice is built on a profound understanding of the entire nervous system’s anatomy and how it all functions together. Because these conditions are so complex, finding the right specialist is a critical first step. If you’re looking for world-class care, it’s essential to research your options and find a doctor with proven experience treating your specific condition.
A huge misconception is that a referral to a neurosurgeon automatically means you’re headed for the operating room. In reality, a massive part of their job is diagnosis and recommending the best path forward—and that path often starts with non-surgical options.
To give you a clearer sense of their work, let’s break down the main areas where a neurosurgeon’s skills are applied.
Primary Areas of Neurosurgical Treatment
The table below provides a quick overview of the major categories of conditions and the parts of the body a neurosurgeon treats. It helps illustrate just how wide-ranging their specialty truly is.
| Area of the Nervous System | Common Conditions Treated |
|---|---|
| Brain | Tumors, aneurysms, traumatic brain injury, hydrocephalus, stroke |
| Spine | Herniated discs, spinal stenosis, fractures, scoliosis, tumors |
| Peripheral Nerves | Carpal tunnel syndrome, ulnar nerve entrapment, nerve injuries |
| Vascular System | Arteriovenous malformations (AVMs), carotid artery disease |
| Pain Syndromes | Trigeminal neuralgia, complex regional pain syndrome (CRPS) |
As you can see, the field goes far beyond just the brain, addressing issues from the top of your head down to the nerves in your hands and feet. This comprehensive approach is what makes their expertise so vital for so many different medical challenges.
Treating the Brain’s Most Complex Conditions
The brain is the body’s command center. It’s an impossibly complex and delicate organ, orchestrating every thought, movement, and feeling we experience. When something goes wrong inside this intricate network, a neurosurgeon’s precision and skill are often the last line of defense, becoming absolutely critical for restoring function and preserving life.
One of the most urgent scenarios they face is a traumatic brain injury (TBI). These are often the devastating result of a sudden, violent impact to the head from a car accident or a serious fall. In these moments, a neurosurgeon has to act immediately to manage swelling, stop any bleeding, and relieve the crushing pressure building inside the skull to prevent irreversible damage.
The scale of this problem is staggering. TBIs affect an estimated 55 to 69 million people across the globe every year, making prompt and expert surgical care essential for improving a patient’s chances. To truly grasp this worldwide health challenge, you can learn more about the global burden of traumatic brain injury30412-1/fulltext).
Of course, neurosurgery isn’t limited to acute trauma. Neurosurgeons also step in to address conditions that develop more slowly within the brain’s delicate structures.
Addressing Brain Tumors and Growths
Hearing you have a brain tumor is terrifying, but this is precisely where a neurosurgeon’s expertise brings clarity and a path forward. Their work involves removing both cancerous (malignant) and non-cancerous (benign) growths from incredibly sensitive areas.
The goal is always the same: remove as much of the tumor as possible without harming the surrounding tissue that controls essential functions like speech, memory, or movement. It’s a task that demands unbelievable precision, often relying on advanced imaging and microsurgical techniques to navigate the brain’s geography.
Managing Vascular and Fluid-Related Issues
The brain’s health is completely dependent on a steady supply of blood and the proper circulation of cerebrospinal fluid (CSF). When these systems fail, a neurosurgeon is called in to perform highly specialized repairs.
- Cerebral Aneurysms: Think of a weak, bulging spot on the wall of a tire. An aneurysm is just like that—a fragile bubble on a blood vessel that could burst and cause a life-threatening bleed. Neurosurgeons can repair these weak spots with tiny clips or coils, preventing a catastrophe.
- Arteriovenous Malformations (AVMs): These are essentially tangled, abnormal knots of blood vessels that disrupt normal blood flow and carry a high risk of hemorrhage. Surgery can be used to remove or block off these dangerous tangles.
- Hydrocephalus: Sometimes called “water on the brain,” this is a build-up of excess cerebrospinal fluid that creates dangerous pressure. A neurosurgeon can implant a device called a shunt, which acts as a drainage system to relieve the pressure.
It’s a common myth that neurosurgeons only perform massive, open operations. The reality is that many modern procedures, especially for vascular issues like aneurysms, are minimally invasive. They are often performed by navigating through blood vessels to reach the brain, avoiding a large incision altogether.
Restoring Function in Movement Disorders
Finally, a significant part of a neurosurgeon’s work involves correcting functional disorders, where the brain’s electrical signaling has gone haywire. Conditions like Parkinson’s disease or essential tremor can cause debilitating shaking and a devastating loss of motor control.
Through a procedure known as Deep Brain Stimulation (DBS), a neurosurgeon can implant a tiny electrode into a very specific part of the brain. This device, which works like a pacemaker for the brain, sends out electrical impulses that help regulate the abnormal signals, restoring smoother, more controlled movement for the patient.
This kind of intervention shows how neurosurgery goes far beyond just saving lives—it dramatically improves the quality of life for people living with chronic, and often debilitating, neurological conditions.
Mastering the Health of the Spine and Spinal Cord

While neurosurgery often brings the brain to mind, a huge part of a neurosurgeon’s world revolves around the spine. This isn’t just a stack of bones; it’s the body’s central support pillar and the armored conduit for the spinal cord—the superhighway connecting your brain to literally everything else.
When something goes wrong with this critical structure, the consequences can be debilitating. A surprising number of people discover that their back or neck pain is a neurosurgical issue. Why? Because the spine is fundamentally a neurological structure. Any problem with the bones (vertebrae) or the cushions (discs) can directly impact the spinal cord and its delicate nerve roots.
Relieving Nerve Compression and Pain
One of the most frequent reasons someone ends up in a neurosurgeon’s office is for a “pinched” nerve. This compression can trigger excruciating pain, weakness, numbness, or a pins-and-needles sensation that travels down an arm or leg.
Think of your spinal cord as the main data cable for a building, with nerve roots branching off to power different floors and rooms. When a disc bulges or a bone spur grows, it’s like a heavy piece of furniture getting pushed against one of those smaller wires. The signal gets interrupted, and the lights in that room start to flicker or go out completely.
The neurosurgeon’s job is to find what’s causing the pressure and remove it, letting the nerve signal flow freely again.
Two classic culprits are:
- Herniated Discs: The gel-like discs between your vertebrae act as shock absorbers. When one ruptures or bulges, that gel can press directly onto a nerve root. This is the underlying cause of most cases of sciatica, that searing pain that shoots from the back down the leg.
- Spinal Stenosis: This is simply a narrowing of the spinal canal. Over time, ligaments can thicken and bone spurs can form, slowly “choking” the space available for the spinal cord and nerves. For patients, this often means severe pain when walking or standing for even short periods.
The goal of surgery here isn’t just about fixing a mechanical problem. It’s about decompressing the nerves. By meticulously creating more space, the surgeon can relieve the pressure, which in turn alleviates the pain and helps restore function so patients can get back on their feet.
Correcting Spinal Instability and Deformity
Beyond pinched nerves, neurosurgeons also tackle major structural failures that threaten the spine’s stability. These are high-stakes situations where surgery is often needed to stabilize the column and protect the spinal cord from catastrophic injury.
A traumatic injury, like one from a bad fall or a car accident, can cause spinal fractures. In these emergencies, a neurosurgeon’s expertise is critical. They work to realign the broken vertebrae and often use medical-grade hardware like titanium screws and rods to build an internal scaffold, holding everything in place while the bone heals. This isn’t just about fixing a broken bone; it’s about preventing paralysis.
Other complex conditions that demand this level of skill include:
- Spinal Tumors: Growths can arise from the vertebrae or even inside the spinal canal, placing dangerous pressure on the spinal cord.
- Scoliosis and Deformities: While many spinal curvatures are mild, severe cases can progress, causing chronic pain, nerve damage, and sometimes even impacting lung function.
- Spondylolisthesis: This condition occurs when one vertebra slips forward on the one below it, creating instability and often pinching the nerves at that level.
For many of these larger structural problems, a neurosurgeon may perform a spinal fusion. This procedure essentially welds two or more vertebrae together into a single, solid bone, eliminating painful motion and providing permanent stability. It’s a complex and delicate operation, but it can be life-changing for patients with severe spinal disorders.
Relieving Pain from Peripheral Nerve Disorders
A neurosurgeon’s world isn’t confined to the brain and spinal cord. Their expertise extends all the way down the body’s intricate electrical wiring—the peripheral nerves. These are the critical data cables branching out from the central nervous system, controlling every movement you make and relaying every sensation you feel. When these nerves get pinched, damaged, or entrapped, a neurosurgeon can often step in to fix the problem.
Think of a peripheral nerve as a delicate fiber-optic cable. If it gets kinked or compressed, the signal becomes weak, distorted, or flat-out painful. This is exactly what’s happening in conditions like carpal tunnel syndrome, one of the most common problems neurosurgeons address.
The median nerve gets squeezed in a narrow channel in the wrist, leading to that all-too-familiar numbness, tingling, and weakness in the hand. A neurosurgeon can perform a straightforward yet incredibly effective procedure to release the tight ligament pressing on the nerve, giving it the space it needs to function properly again. The relief can be almost immediate.
Addressing Nerve Injuries and Entrapment
But nerve problems aren’t just limited to the wrist. Neurosurgeons are masters of microsurgery, equipped to treat a whole host of nerve entrapment syndromes and traumatic injuries all over the body.
This is painstaking work, often involving repairing or decompressing these vital structures under a high-powered microscope.
Common examples include:
- Ulnar Nerve Entrapment: You know that “funny bone” nerve? It can get compressed at the elbow, causing numbness and weakness in your ring and little fingers. A surgeon can move the nerve to a better-protected position.
- Peroneal Nerve Injury: This nerve, located near the knee, can be damaged in an accident, leading to “foot drop”—an inability to lift the front of your foot.
- Nerve Lacerations: After a deep cut severs a nerve, a neurosurgeon can meticulously stitch the delicate ends back together, creating a bridge for the nerve fibers to regrow and restore function over time.
The Next Frontier: Functional Neurosurgery
Beyond fixing structural problems, a highly specialized field called functional neurosurgery is changing the game for patients with complex disorders. This isn’t about repairing a cut or releasing a pinched nerve; it’s about fundamentally recalibrating the nervous system’s faulty signals to dramatically improve quality of life.
It’s a groundbreaking approach for people who have run out of options.
Functional neurosurgery doesn’t just remove a problem—it modulates the nervous system’s response to it. By using targeted electrical stimulation, surgeons can effectively turn down the volume on chronic pain signals or correct the misfiring circuits that trigger seizures and tremors.
Procedures like deep brain stimulation (DBS), which are well-known for treating movement disorders like Parkinson’s, can be adapted to manage severe, unrelenting pain. By implanting a tiny electrode, a neurosurgeon can intercept and disrupt the pain signals before they ever reach the brain. This technology offers profound hope for patients battling conditions like epilepsy or chronic pain that has resisted every other therapy, showcasing just how much neurosurgery can do to restore a person’s daily life.
Understanding When You Should See a Neurosurgeon
Figuring out if a particular ache or symptom is serious enough for a neurosurgeon can feel like a guessing game. Most of the time, the path starts with your primary care doctor or a neurologist. They’ll run initial tests and, if needed, make the referral to the right specialist. You won’t be left to figure it out alone.
That said, there are definitely “red flag” symptoms that should have you calling your doctor right away. Think of things like persistent back pain that shoots down your leg (sciatica), crippling headaches that come with vision problems or weakness, or a sudden loss of strength after an injury. These are clear signs that something needs a much closer look.
It’s critical to remember that a referral to a neurosurgeon doesn’t automatically mean surgery is on the table. Far from it. These specialists are diagnosticians first and surgeons second. They often start with conservative, non-surgical treatments, like highly specific physical therapy or targeted pain management injections.
Neurologist vs. Neurosurgeon: What Is the Difference?
One of the most common points of confusion for patients is the difference between a neurologist and a neurosurgeon. They both treat the nervous system, but their roles are fundamentally different. A neurologist diagnoses and manages conditions medically, while a neurosurgeon steps in to provide surgical fixes for structural problems.
A simple way to think about it is that a neurologist is like an electrician who diagnoses faulty wiring in a house, while a neurosurgeon is the specialist who physically repairs or replaces that wiring when needed.
This decision tree helps illustrate how a general symptom like nerve pain can branch out into different diagnoses, ultimately guiding whether you end up seeing a neurologist or a neurosurgeon.
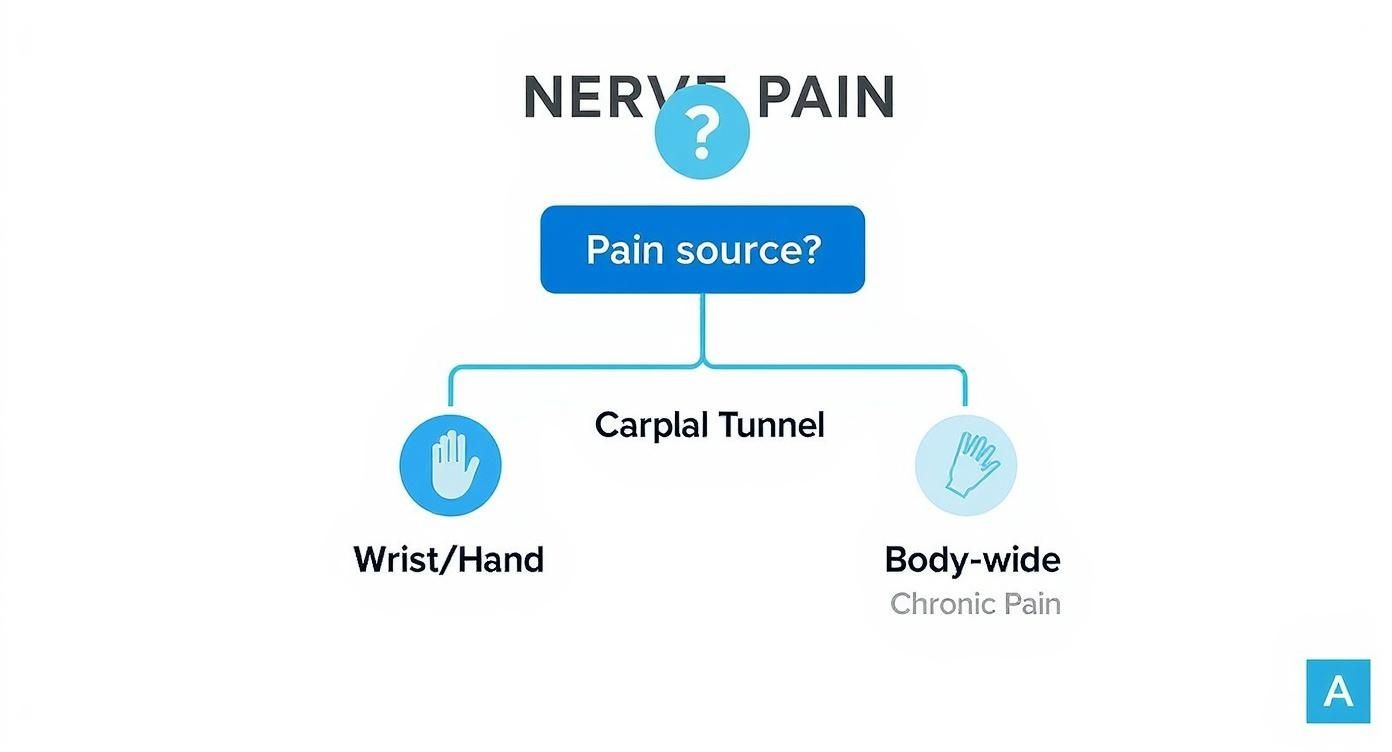
As the graphic shows, pinpointing the source of your pain is the first step in figuring out what’s really going on—and what kind of specialist you need. For anyone serious about getting top-tier care, connecting with the right expert from the start is essential. Our guide on how to find the best neurosurgeons in New York is a great resource for navigating this process.
To make the distinction even clearer, here’s a direct comparison of their roles and responsibilities.
Neurologist vs. Neurosurgeon Key Differences
| Aspect | Neurologist | Neurosurgeon |
|---|---|---|
| Primary Role | Diagnoses and manages neurological disorders with medication and non-invasive therapies. | Diagnoses and treats neurological conditions with surgical interventions. |
| Approach | Medical management (medication, lifestyle changes, therapy). | Surgical and non-surgical management of structural issues. |
| Performs Surgery | No | Yes |
| Common Conditions | Migraines, epilepsy, multiple sclerosis, stroke management. | Brain tumors, herniated discs, spinal fractures, aneurysms. |
Understanding this key difference helps set clear expectations. While both specialists are crucial for brain and spine health, knowing who does what ensures you’re on the fastest path to the right kind of treatment.
When most of us think of neurosurgery, we picture state-of-the-art hospitals in major cities. The reality for much of the world, however, couldn’t be more different. The desperate need for neurosurgical expertise reveals a staggering global health crisis that extends far beyond the developed world.
Every single year, an estimated 22.6 million people face neurological problems that require a neurosurgeon. For nearly 13.8 million of them, surgery is a necessity to treat devastating conditions like traumatic brain injuries, strokes, and brain tumors. This isn’t just a statistic; it’s a massive, unmet human need. For a closer look at the data behind this challenge, you can review the executive summary on essential neurosurgical care.
Nowhere is this gap more apparent than in low- and middle-income countries.
The World Health Organization paints a grim picture: some African nations have just a single neurosurgeon for several million people. This scarcity means a child with a treatable condition like hydrocephalus or an adult with a head injury from an accident can face a life of disability—or worse.
This global perspective forces us to see neurosurgery not as a niche specialty, but as a critical line of defense in saving lives and preventing lifelong disability on an enormous scale.
Your Top Questions About Neurosurgery, Answered
Stepping into the world of neurosurgery can feel intimidating, and it’s natural to have questions. Getting clear, straightforward answers is the first step toward feeling in control of your health. Let’s tackle some of the most common concerns patients have.
Do I Need a Referral to See a Neurosurgeon?
Yes, in almost all cases, you’ll need a referral. Think of it as a crucial first step in your care pathway. This referral usually comes from your primary care physician or a neurologist who has already done an initial evaluation.
This process is in place for a good reason. It makes sure that a neurosurgeon is the right specialist for your specific problem before you even book an appointment. Your referring doctor will typically order preliminary tests, like an MRI or CT scan, so the neurosurgeon has all the necessary information for a productive first visit.
Does Seeing a Neurosurgeon Mean I’m Definitely Having Surgery?
Not at all. This is probably the biggest misconception out there. Consulting with a neurosurgeon is about getting an expert diagnosis and a complete treatment plan, not just a ticket to the operating room.
Neurosurgeons are masters of the entire nervous system, and their first priority is always to explore the least invasive, most effective options. Surgery is a powerful tool, but it’s one of many.
Often, the best path forward involves conservative treatments, such as:
- Physical Therapy: To build strength, improve function, and support the affected area.
- Medication Management: For controlling pain and reducing inflammation at the source.
- Targeted Injections: To deliver powerful relief directly where it’s needed most.
Surgery only enters the conversation when these conservative approaches haven’t provided relief, or if a condition poses a direct or worsening threat to your health.
A neurosurgical consultation is fundamentally a diagnostic meeting. It’s your chance to get an elite opinion on what’s causing your symptoms and to understand every possible treatment path—both surgical and non-surgical.
The key is finding the right expert to guide you through this process. If you’re looking for a specialist who aligns with your needs, it can be helpful to review some proven ways to find top-rated physicians near me.
At Haute MD, we connect you with the nation’s leading specialists who are vetted for their expertise and commitment to patient outcomes. Discover a network of elite physicians dedicated to providing you with world-class care. Find your trusted specialist at https://www.hauteliving.com/hautemd.

