
An immunologist is a highly specialized physician who diagnoses and manages disorders of the body’s complex defense network. They’re the experts you turn to when this system goes haywire—either by overreacting to harmless substances (allergies), mistakenly attacking your own body (autoimmune diseases), or being too weak to fight off infections (immunodeficiencies).
Your Immune System’s Expert: The Role of an Immunologist
Think of your immune system as a highly trained internal security force. Its mission is to identify and neutralize real threats like bacteria, viruses, and other pathogens. An immunologist is like the strategic commander of this force, holding a deep, nuanced understanding of its every function, strength, and vulnerability.
Their expertise becomes absolutely critical when this system malfunctions in one of three ways.
Sometimes, the security force becomes overzealous, misidentifying harmless things like pollen, pet dander, or peanuts as dangerous invaders. This is the root of allergies and hypersensitivity reactions. Other times, the system’s targeting goes haywire, launching a “friendly fire” assault against your own healthy cells and tissues, which is the hallmark of autoimmune conditions.
Finally, an immunologist steps in when this defense system is inherently weak or compromised, a state known as immunodeficiency. In these cases, patients become highly susceptible to frequent or severe infections that a healthy body would easily defeat.
The scope of their work is massive. Allergic conditions alone affect huge portions of the population; for instance, allergic rhinitis (hay fever) impacts about 7.8% of adults in the U.S., and it’s estimated that 1 in 20 children has a food allergy.
This graphic breaks down the three core areas of an immunologist’s focus.
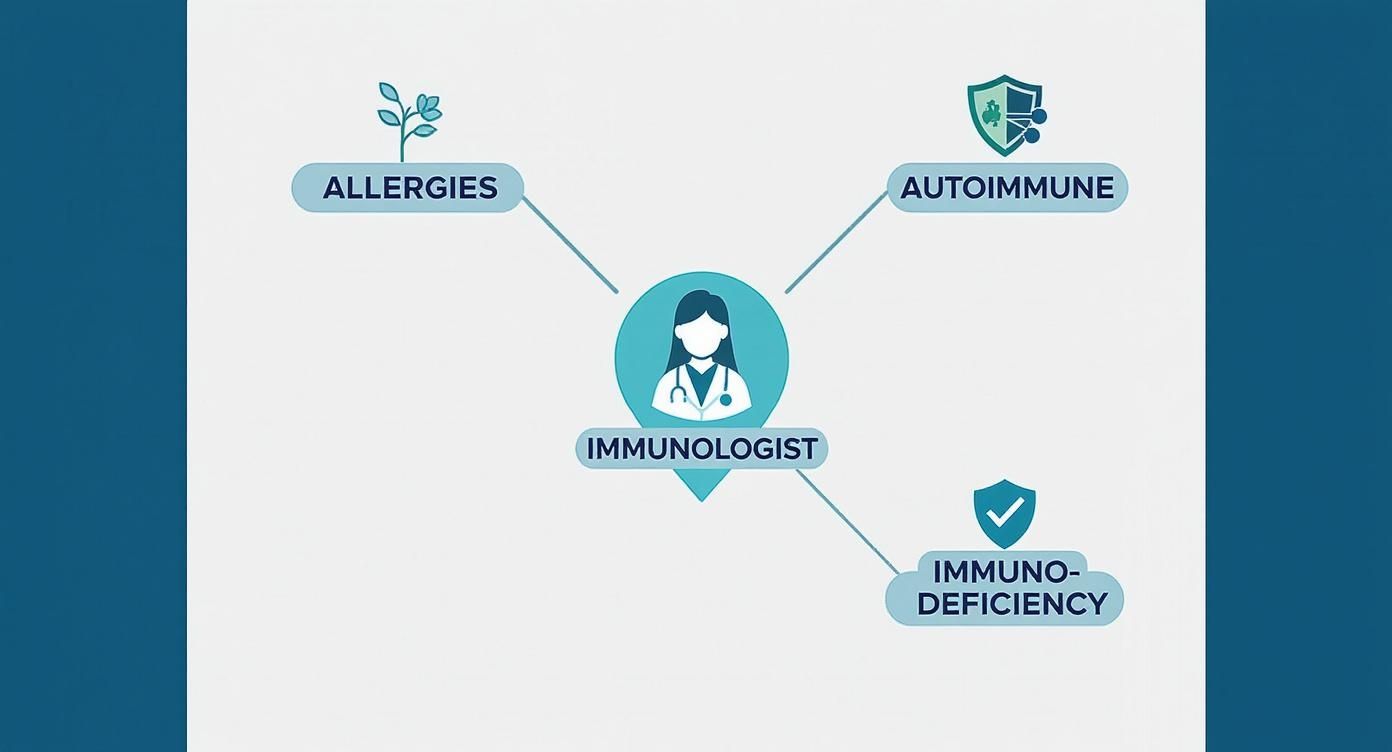
As the visualization shows, an immunologist’s role is centered on correcting these three fundamental types of immune system errors. Let’s take a closer look at the specific conditions they manage.
Conditions Commonly Treated by an Immunologist
To give you a clearer picture, this table breaks down the main categories of disorders an immunologist handles, along with some common examples you might recognize.
| Category of Disorder | What It Means | Common Examples |
|---|---|---|
| Autoimmune Diseases | The immune system mistakenly attacks the body’s own healthy cells and tissues. | Rheumatoid Arthritis, Lupus (SLE), Celiac Disease, Multiple Sclerosis (MS), Type 1 Diabetes |
| Hypersensitivities / Allergies | An exaggerated or inappropriate immune response to a harmless substance. | Allergic Rhinitis (Hay Fever), Food Allergies (e.g., peanut, milk), Asthma, Eczema (Atopic Dermatitis), Hives |
| Immunodeficiencies | The immune system is weakened, making it difficult to fight off infections. | Common Variable Immunodeficiency (CVID), Severe Combined Immunodeficiency (SCID), HIV/AIDS |
| Autoinflammatory Syndromes | The innate immune system causes episodes of inflammation without an infection or autoimmune trigger. | Familial Mediterranean Fever (FMF), Periodic Fever Syndromes |
Navigating these complex conditions requires a specialist who can accurately diagnose the problem and create a precise, personalized treatment plan. You can learn more about this medical specialty and find top-tier physicians in our network of allergy and immunology experts.
Navigating Autoimmune Disease When the Body Attacks Itself
One of the toughest challenges an immunologist tackles is autoimmune disease, a situation where the body’s own defense system gets confused and attacks healthy tissue. Imagine your immune system as a highly trained security team. Its job is to spot and eliminate genuine threats. But in autoimmune disease, that team starts targeting your own cells—a case of “friendly fire” that can cause devastating, body-wide damage.
This internal assault is behind more than 100 chronic and often debilitating conditions. The damage can show up anywhere. In Rheumatoid Arthritis, it’s the joints. In Lupus, it can be the skin, kidneys, brain, and joints all at once. For people with Multiple Sclerosis, the immune system chews away at the protective coating around nerves, while in Celiac Disease, it’s gluten that triggers an attack on the small intestine.
The Immunologist as Medical Detective
Pinning down an autoimmune diagnosis is notoriously tricky. The symptoms are often vague, they come and go, and they can easily be mistaken for something else entirely. This is where an immunologist steps in, acting like a medical detective. They meticulously piece together clues from your personal history, physical exams, and highly specific blood tests that hunt for autoantibodies—the rogue proteins that are actually driving the attack.
An autoimmune disorder happens when the body’s security system can’t tell the difference between “self” and “other.” It mistakes your own healthy cells for foreign invaders and launches an attack. Managing this case of mistaken identity is the core of an immunologist’s work.
Recognizing the early warning signs is a huge step toward getting things under control. If you’re dealing with a strange mix of symptoms that don’t seem to add up, reviewing an autoimmune symptoms checklist can help you spot potential patterns to discuss with a specialist.
These diseases are becoming alarmingly common. A massive study involving 22 million people revealed that autoimmune conditions now impact roughly one in ten people globally. Some experts are even calling it an epidemic, which highlights just how critical specialized immunological care has become. You can read the full research about these findings here.
Crafting a Long-Term Management Strategy
So, once the diagnosis is clear, what’s the game plan? An immunologist’s job isn’t just to mask the symptoms. The real goal is to get the immune system to stand down—to modulate its response without shutting it down completely.
This often requires a sophisticated toolkit of medications designed to calm the overactive immune system. The main players include:
- Corticosteroids: These are the fast-acting heavy hitters used to quickly crush severe inflammation during a flare-up.
- Immunosuppressants: These medications take a broader approach, dialing down the entire immune response to give the body a break.
- Biologics: This is where treatment gets really precise. Biologics are advanced therapies engineered to block the specific molecules or pathways that are fueling the inflammation.
The immunologist’s expertise lies in tailoring these treatments to the individual. It’s a constant balancing act—controlling the disease while preserving enough immune function to fight off actual infections. This delicate, ongoing management is the key to protecting organ function and giving patients back their quality of life.
Taming Allergies and Hypersensitivity Reactions

Allergies are one of the most common battlegrounds where immunologists step in. We’ve all seen them: the seasonal sneezing, the hives from a mystery food, the wheezing around a friend’s cat. These aren’t just minor annoyances; they’re the result of an immune system in overdrive.
Essentially, your body is making a huge mistake. It’s flagging a harmless substance—like pollen, peanuts, or pet dander—as a dangerous invader and launching an all-out war. The job of an immunologist is to calm this hypersensitive response and restore order.
Their approach goes way beyond just telling you to take an over-the-counter antihistamine. It starts with precision diagnostics to identify the exact culprits. This isn’t guesswork. It’s a detailed investigation using tools like skin prick tests (where tiny amounts of allergens are introduced to the skin) or specific blood tests that measure the enemy combatants: IgE antibodies.
A Deeper Approach to Allergic Conditions
Once the triggers are locked down, an immunologist crafts a personalized strategy. The goal isn’t just to manage the symptoms but to fundamentally change the immune system’s misdirected behavior. They are experts in a whole spectrum of conditions that spring from this root cause of immune overreaction.
Common conditions an immunologist takes on include:
- Severe Asthma: Managing the chronic, smoldering inflammation in the airways that is so often tied to allergic triggers.
- Eczema (Atopic Dermatitis): Treating this frustrating inflammatory skin condition, which frequently has a strong allergic component.
- Anaphylaxis: Creating emergency action plans and long-term strategies for those facing life-threatening reactions to foods, medications, or insect stings.
- Chronic Sinusitis: Digging into the root cause of recurrent sinus infections, which are often fueled by underlying, untreated allergies.
For many patients, the ultimate goal is not just to dodge triggers for the rest of their lives. It’s about retraining the immune system so it no longer overreacts. This is where advanced therapies become a true game-changer, offering a path to long-term relief instead of a lifetime of symptom management.
This is precisely why an immunologist’s care is so vital. Instead of just patching up the damage, they target the core malfunction in the immune system.
One of the most powerful tools in their arsenal is allergen immunotherapy, known more commonly as allergy shots or drops. This is a brilliant piece of biological engineering. By exposing your body to gradually increasing doses of your specific allergen, the treatment slowly teaches your immune system to tolerate the substance instead of attacking it.
Think of it as a desensitization bootcamp for your immune cells. Over time, this controlled exposure retrains the system, leading to a massive reduction in symptoms and a real, lasting improvement in quality of life. It’s the difference between constantly reacting and achieving genuine tolerance.
Strengthening Defenses Against Immunodeficiency

While we often hear about allergies and autoimmune diseases—conditions driven by an overactive immune system—immunologists also manage the exact opposite problem: immunodeficiency. This is when the body’s defenses are too weak, leaving a person dangerously exposed.
Think of your immune system as a fortress wall. With immunodeficiency, that wall has critical gaps, leaving the body vulnerable to invaders. This weakness often shows up as recurrent, severe, or unusual infections. It’s the person who gets pneumonia again and again, suffers from constant sinus infections, or struggles with illnesses that just won’t go away. When these patterns emerge, an immunologist is needed to figure out why the defenses are failing.
Primary vs. Secondary Immunodeficiency
Immunologists generally sort these conditions into two main buckets, each with a very different origin story.
- Primary Immunodeficiencies (PI): These are the ones you’re born with. They are genetic, meaning some crucial component of the immune system was missing or dysfunctional from the start.
- Secondary (or Acquired) Immunodeficiencies: These conditions develop later in life. They’re caused by outside factors that damage the immune system over time, like certain medications (chemotherapy is a common one), chronic diseases, or infections.
An immunologist’s expertise covers a huge range of these disorders. For instance, Common Variable Immunodeficiency (CVID) is one of the more prevalent types, where a lack of necessary antibodies leads to repeated infections. On the other end of the spectrum is Severe Combined Immunodeficiency (SCID), a far more serious condition affecting critical T cells and B cells, which is often caught during newborn screening.
Diagnosing these conditions requires a deep dive into blood tests and sometimes genetic analysis to pinpoint the exact weakness. You can discover more insights about how these conditions are treated on acaai.org.
Rebuilding the Body’s Shield
When a patient has an immunodeficiency, the immunologist’s goal is to reinforce their weakened defenses. It’s a proactive strategy.
For many patients, especially those with antibody deficiencies, a cornerstone of treatment is immunoglobulin (Ig) replacement therapy.
This therapy is like giving the body a borrowed shield. It involves administering concentrated antibodies collected from healthy donors, giving the patient the ammunition they need to fight off infections when their own system can’t produce it.
By providing this protective boost, immunologists can dramatically reduce how often their patients get sick and how severe those illnesses become. Their work isn’t just about treating sickness as it comes—it’s about building a stronger defensive foundation to help their most vulnerable patients lead healthier lives.
When to See an Immunologist Key Signs to Watch For
Figuring out when your symptoms point to an immune system problem isn’t always straightforward. While your primary doctor is the right place to start, certain red flags should tell you it’s time to bring in a specialist.
The first major clue is often a pattern of persistent or recurring health issues that just don’t get better with standard treatments. This can signal an underlying issue with your body’s defense systems—whether they’re working overtime, not working hard enough, or simply attacking the wrong targets. Recognizing these patterns is the crucial first step toward getting an accurate diagnosis.
Key Indicators for a Specialist Visit
If any of the following situations sound familiar, a conversation with an immunologist is a logical next step. These are common signs that a deeper dive into your immune health is necessary.
- Recurrent Infections: Are you constantly battling colds or other bugs? More than four new ear infections or two serious sinus infections within a single year can be a serious warning sign of an underlying weakness in your immune defenses.
- Uncontrolled Asthma or Allergies: When standard medications aren’t enough to manage your asthma or you’re dealing with allergies that never seem to go away, an immunologist can offer far more advanced diagnostics and treatments. You can learn more about managing severe symptoms in this guide to acute asthma exacerbation treatment.
- Severe Reactions: A single, severe, body-wide reaction to something like an insect sting or a specific food demands expert evaluation. An immunologist can help you understand the trigger and create a plan to prevent a future life-threatening episode.
A family history of primary immunodeficiency is another critical reason to seek an expert opinion. Genetic predispositions can significantly raise your risk, making proactive screening and management essential for your long-term health.
Answering Your Questions About Seeing an Immunologist
Stepping into the world of medical specialists can feel like learning a new language. But figuring out who does what—and how to see them—doesn’t have to be complicated. Let’s clear up some of the most common questions people have before their first immunologist visit.
Allergist vs. Immunologist: What’s the Difference?
You’ve probably heard both terms, and the overlap is a major source of confusion. Here’s the simple answer: in the United States, every board-certified allergist is also a fully trained immunologist. Their training covers the entire spectrum of the immune system.
So why the two different titles? It often comes down to the doctor’s day-to-day focus.
- An allergist primarily concentrates on hypersensitivity reactions—think seasonal allergies, food allergies, asthma, and hives.
- An immunologist might see all of those same patients but also manages the more complex side of the field, like autoimmune diseases and immunodeficiency disorders.
Think of it as a specialty within a specialty. The title they use simply reflects where they concentrate their expertise.
The bottom line is that an allergist has all the training of an immunologist. You’re in qualified hands either way; the title just gives you a hint about the main focus of their practice.
How Do I Get a Referral to an Immunologist?
For most people, the path to a specialist starts with a conversation with their primary care physician (PCP). Your PCP is your healthcare quarterback, the one who first evaluates your symptoms and looks at the big picture.
If they spot a pattern that points to an immune system issue—maybe you’re getting sick constantly, your asthma is out of control, or you have symptoms suggesting an autoimmune condition—they’ll make the referral. This step is crucial, as it ensures you land in the right specialist’s office and is often required for your insurance to cover the visit.
Before your PCP appointment, get your story straight. Jot down a detailed list of your symptoms, when they started, and what makes them better or worse. The clearer the picture you can paint, the easier it is for your doctor to connect the dots.
What Should I Expect During My First Visit?
Your first appointment is less of an exam and more of a deep dive into your personal health story. The immunologist will want to know everything: your medical history, your family’s medical history, and a minute-by-minute account of the symptoms that brought you to their door. Be prepared for detailed questions.
After a thorough discussion, they’ll perform a physical exam. From there, the real detective work begins with diagnostic testing tailored to your situation. This could include:
- Blood tests to hunt for specific antibodies or measure your immune cell counts.
- Skin prick tests to pinpoint environmental or food allergens.
- Breathing tests (spirometry) to evaluate your lung function if asthma is on the table.
This initial visit is all about gathering clues. The goal is to build a precise diagnosis that leads to an equally precise and effective treatment plan.
When you’re dealing with a complex immune condition, finding an elite specialist is non-negotiable. At Haute MD, we connect you with the nation’s leading, board-certified immunologists known for their deep expertise and patient-centered approach. Explore our network of trusted physicians today.

