
Autoimmune diseases, affecting over 24 million people in the U.S. alone, occur when the body’s immune system mistakenly attacks its own healthy tissues. This internal conflict can manifest as a bewildering array of symptoms that often mimic other conditions, making diagnosis a complex and lengthy journey. From persistent fatigue that sleep can’t fix to mysterious rashes and joint pain, these signs can be subtle yet significant.
Understanding these signals is the first critical step toward gaining clarity and seeking the right medical guidance. This comprehensive autoimmune symptoms checklist is specifically designed to help you recognize potential patterns, organize your concerns, and have more informed, productive conversations with your healthcare professionals. It serves as a structured guide to help you articulate your experiences with precision.
We will break down eight of the most common signs, grouped by the body systems they impact, from dermatological changes to neurological disturbances. For each symptom, we will provide clear descriptions and highlight key indicators that warrant a specialist’s attention. Our goal is to provide an actionable framework, empowering you to navigate your health journey with greater confidence and purpose. This checklist is not a diagnostic tool, but a powerful resource for self-advocacy and a starting point for a deeper medical investigation. By systematically evaluating your symptoms, you can better partner with your physician to uncover the root cause and find the most effective path forward.
1. Chronic Fatigue and Exhaustion
Topping our autoimmune symptoms checklist is chronic fatigue, a profound and persistent state of exhaustion that is far more severe than simple tiredness. Unlike the fatigue you might feel after a long day, autoimmune-related exhaustion is a hallmark symptom that doesn’t improve with rest. It stems from the body’s ongoing immune response, where systemic inflammation consumes vast amounts of energy, leaving you feeling perpetually depleted.
This isn’t just feeling sleepy; it is a debilitating exhaustion that significantly interferes with daily life, professional responsibilities, and personal commitments. For example, a person with Lupus might find themselves needing lengthy afternoon naps just to get through the day, while someone with Rheumatoid Arthritis may sleep for over 12 hours and still wake up feeling completely unrested. This symptom is a critical red flag because it signals that the body is in a constant state of high alert, diverting resources to fight a perceived internal threat.
Key Characteristics of Autoimmune Fatigue
The defining feature of this type of fatigue is its unresponsiveness to conventional remedies like sleep or caffeine. It often includes a phenomenon known as post-exertional malaise (PEM), where even minor physical or mental exertion can trigger a “crash” or a significant worsening of symptoms that can last for days. This is a critical distinction from standard tiredness. For instance, a patient with Multiple Sclerosis (MS) might be unable to finish a full workday due to this overwhelming energy depletion, a direct consequence of the nervous system’s inflammatory burden.
To help distinguish this systemic symptom from everyday tiredness, the following summary box outlines its core features.
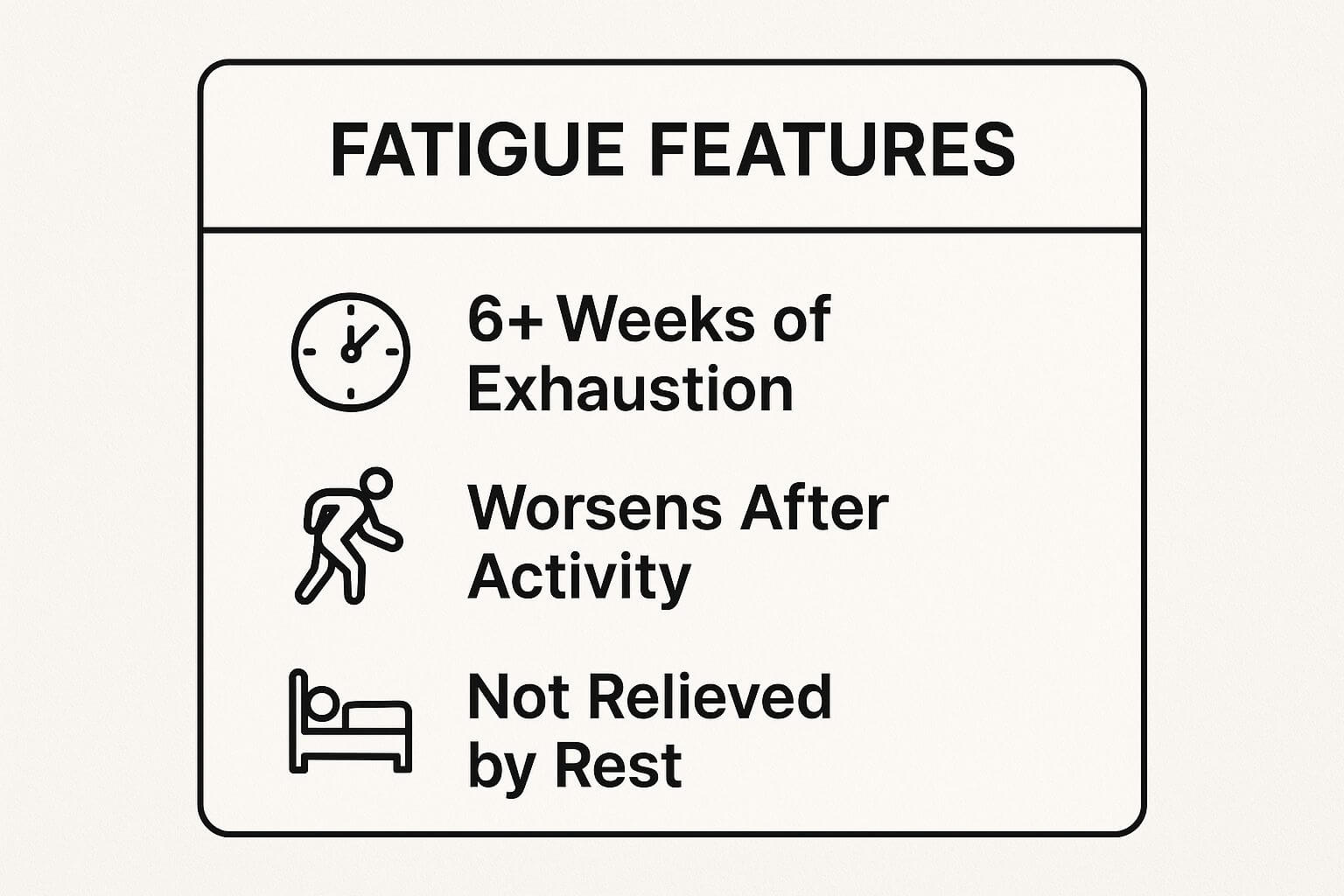
As the visualization highlights, fatigue that persists for over six weeks, is not relieved by rest, and worsens after activity is a significant indicator that requires medical evaluation.
Actionable Steps for Management
Managing this level of exhaustion requires a proactive and strategic approach. It is essential to work with a medical professional to rule out other potential causes, such as anemia, thyroid dysfunction (even in treated Hashimoto’s), vitamin deficiencies, or sleep apnea.
Once other causes are excluded, consider implementing the following strategies:
- Keep a Fatigue Diary: Document your energy levels on a scale of 1-10 throughout the day. Note activities, food, and sleep patterns to identify potential triggers and patterns of PEM.
- Practice Energy Pacing: Treat your energy like a bank account. Break large tasks into smaller, manageable segments with scheduled rest periods in between to avoid “energy debt.”
- Consult an Occupational Therapist: These specialists can provide personalized strategies for activity management and help you modify your environment to conserve energy effectively.
- Prioritize Sleep Hygiene: Maintain a consistent sleep-wake schedule, create a cool, dark, and quiet sleep environment, and avoid stimulants like caffeine or screen time before bed.
2. Joint Pain and Swelling (Arthralgia)
A prominent entry on any autoimmune symptoms checklist is arthralgia, or joint pain, which often progresses to include visible swelling and stiffness. This symptom arises when the immune system erroneously targets the synovial lining of the joints, triggering an inflammatory cascade. Unlike mechanical joint pain from an injury, autoimmune-related joint issues are often symmetrical, affecting the same joints on both sides of the body, such as both wrists or both knees.
This persistent inflammation can cause significant discomfort, limit mobility, and, if left unmanaged, lead to permanent joint damage. For instance, a person with Rheumatoid Arthritis may experience painful, swollen knuckles that make simple tasks like buttoning a shirt difficult, while someone with Ankylosing Spondylitis might feel profound stiffness in their lower back, especially in the morning. This symptom is a critical indicator because it points directly to systemic inflammation rather than localized wear and tear.

Key Characteristics of Autoimmune Arthralgia
The defining feature of autoimmune joint pain is its inflammatory nature. It is typically accompanied by prolonged morning stiffness that lasts for more than an hour and often improves with gentle movement, only to worsen again with rest. The pain may also be migratory, moving from one joint to another, as is sometimes seen in Lupus. In conditions like Psoriatic Arthritis, the joint inflammation can be accompanied by dactylitis, or “sausage digits,” where an entire finger or toe becomes swollen.
To help differentiate this systemic symptom from other types of joint pain, the video below provides a deeper look into the mechanisms of autoimmune arthritis.https://www.youtube.com/embed/wr7MInAA1yU
As the video explains, symptoms like symmetry, prolonged stiffness, and involvement of multiple joints are significant red flags that warrant a comprehensive medical investigation.
Actionable Steps for Management
Effectively managing inflammatory joint pain requires a partnership with a rheumatologist to diagnose the underlying condition and initiate appropriate medical treatment. To gain a better understanding of how top medical experts approach these conditions, you can explore resources that feature some of the top doctors who treat arthritis.
In conjunction with medical care, consider implementing these supportive strategies:
- Create a Symptom Log: Document which joints are affected, the severity of pain on a 1-10 scale, and the duration of morning stiffness. Take photos of visibly swollen joints to track changes for your physician.
- Use Temperature Therapy: Apply cold packs to acutely swollen and inflamed joints for 15-20 minutes to reduce swelling. Use warm compresses or a warm shower to ease stiffness, especially in the morning.
- Maintain Gentle Movement: Engage in low-impact, range-of-motion exercises like swimming or gentle yoga. This helps maintain joint flexibility and strengthens supporting muscles without exacerbating inflammation.
- Utilize Assistive Devices: When experiencing a flare, use tools like jar openers, ergonomic keyboards, or walking aids to reduce stress on affected joints during daily activities.
3. Skin Rashes and Lesions
Skin manifestations are often one of the first and most visible indicators on an autoimmune symptoms checklist. These are not ordinary skin irritations; they are abnormal changes like rashes, lesions, hives, or discoloration that arise when the immune system mistakenly targets and attacks healthy skin cells and tissues. This inflammation can present in highly specific ways, providing crucial visual clues that can help guide a diagnosis for an underlying systemic condition.
This symptom is a critical red flag because the skin often acts as a window to internal inflammation. For example, the classic malar or “butterfly” rash across the cheeks and nose is a hallmark sign of Systemic Lupus Erythematosus, often appearing after sun exposure. Similarly, the thick, scaly plaques of Psoriasis on elbows and knees are a direct result of an overactive immune response accelerating skin cell growth. Other distinct examples include the purple-red heliotrope rash on the eyelids seen in Dermatomyositis or the tight, thickened skin patches characteristic of Scleroderma.
Key Characteristics of Autoimmune Skin Issues
The defining feature of autoimmune-related skin conditions is their persistence, specific patterns, and frequent association with other systemic symptoms. Unlike a simple allergic reaction that resolves quickly, these rashes can be chronic, recurrent, or change in appearance over time. They are often triggered or worsened by specific factors like sunlight (photosensitivity), stress, or illness. For instance, a person with autoimmune thyroid disease might develop patches of depigmented skin, known as Vitiligo, that progressively spread.
To help distinguish these systemic symptoms from common dermatological issues, the following summary box outlines their core features.
As the visualization highlights, rashes that are symmetrical, triggered by UV light, or accompanied by other systemic symptoms like joint pain or fatigue warrant a comprehensive medical evaluation.
Actionable Steps for Management
Managing autoimmune skin manifestations requires a dual approach that addresses both the skin itself and the underlying immune dysregulation. It is essential to consult a dermatologist, who may perform a skin biopsy to confirm a diagnosis and rule out other conditions.
Once diagnosed, consider implementing these targeted strategies:
- Document and Track Changes: Photograph any rashes or lesions with date stamps to monitor their progression, size, and color. Keep a detailed log of potential triggers, including sun exposure, stress levels, new foods, or medications.
- Prioritize Sun Protection: Photosensitivity is a common trigger. Use a broad-spectrum SPF 50+ sunscreen daily, even on overcast days, and wear UPF-protective clothing, wide-brimmed hats, and sunglasses during outdoor activities.
- Adopt a Gentle Skincare Routine: Avoid harsh soaps, exfoliants, and products with fragrances or alcohol that can irritate compromised skin. Instead, opt for gentle, hydrating cleansers and fragrance-free moisturizers to support the skin barrier. For more insights on building a protective routine, you can explore skincare essentials recommended by medical experts.
- Seek Dermatological Consultation: For any persistent, unusual, or worsening skin changes, a board-certified dermatologist is the best resource. They can provide an accurate diagnosis and prescribe appropriate treatments, from topical steroids to systemic medications.
4. Brain Fog and Cognitive Dysfunction
Next on our autoimmune symptoms checklist is brain fog, a frustrating and often misunderstood constellation of cognitive issues. This is not simple forgetfulness; it is a pervasive mental cloudiness that includes difficulty concentrating, memory problems, mental confusion, and slowed thinking. This symptom arises directly from systemic inflammation and the immune system’s misdirected attack, which can impact the brain and central nervous system, disrupting normal neurological function.
This cognitive dysfunction can be as debilitating as any physical symptom, severely impacting professional performance, personal relationships, and the ability to manage daily tasks. For instance, a person with Sjögren’s syndrome may find themselves unable to follow a conversation or retain information from a book they just read. Similarly, someone with Hashimoto’s thyroiditis might struggle with significant memory lapses or an inability to find the right words, a direct result of the inflammatory process affecting their cognitive pathways.
Key Characteristics of Autoimmune Brain Fog
The hallmark of autoimmune-related brain fog is its link to disease activity and inflammation levels. It often feels like a mental “sludge” that makes clear thinking feel impossible. This cognitive impairment can fluctuate, worsening during a flare-up and sometimes improving during periods of remission. It’s a critical sign that the body’s inflammatory response is directly impacting the nervous system.
A patient with Lupus, for example, might forget important appointments or frequently misplace items, not due to carelessness, but because of neurologically-based cognitive deficits. This is a far cry from occasionally forgetting where you put your keys; it’s a persistent impairment.
Actionable Steps for Management
Addressing brain fog requires a multi-faceted approach aimed at reducing inflammation and supporting cognitive function. It is crucial to discuss these symptoms with your doctor to ensure they are properly attributed to your autoimmune condition and not another underlying issue.
Once confirmed, integrating the following strategies can help you regain mental clarity:
- Implement Organizational Systems: Use digital calendars, smartphone reminders, and detailed to-do lists to offload cognitive burdens. Keep a dedicated notebook for important information.
- Break Down Complex Tasks: Divide large projects or cognitively demanding activities into smaller, more manageable steps. This prevents overwhelm and makes tasks feel more achievable.
- Practice Strategic Scheduling: Identify your “peak” cognitive hours and schedule your most mentally intensive tasks during these periods. Reserve low-energy times for simpler activities.
- Minimize Environmental Distractions: Create a quiet, organized workspace. Use noise-canceling headphones or apps that block distracting websites to help you focus.
- Request Workplace Accommodations: If brain fog impacts your job, consider discussing reasonable accommodations with your employer, such as flexible hours, a quieter workspace, or written instructions.
5. Recurring Fever and Unexplained Temperature Fluctuations
Another critical entry in our autoimmune symptoms checklist is the presence of recurring or persistent low-grade fevers without an obvious infection. These temperature fluctuations happen because the immune system’s chronic activation triggers a systemic inflammatory response. This process, involving inflammatory cytokines, directly impacts the hypothalamus, the brain’s thermostat, leading to a higher body temperature set point.
This isn’t the typical high fever you get with the flu; it’s often a subtle, persistent low-grade fever (e.g., 99.5-101°F or 37.5-38.3°C) that lingers for weeks or comes in waves. For example, a person with Lupus may experience these low-grade fevers as a primary sign of a disease flare, while someone with Adult-onset Still’s Disease might have dramatic daily fever spikes that coincide with a rash. This symptom is a major red flag as it indicates widespread, systemic inflammation, signaling that the body is actively fighting itself.
Key Characteristics of Autoimmune Fever
The defining feature of an autoimmune-related fever is its origin: it is a fever of unknown origin (FUO) driven by inflammation, not infection. Consequently, it won’t respond to antibiotics and often correlates directly with the level of autoimmune disease activity. Unlike a fever from a common cold that resolves in a few days, this type of fever can persist indefinitely until the underlying inflammation is controlled.
For instance, a patient with vasculitis might present with a stubborn fever as their main symptom before a diagnosis is even considered. Similarly, individuals with inflammatory bowel disease (IBD) often run a low-grade fever during active intestinal inflammation. Distinguishing this symptom from an infectious process is a crucial diagnostic step.
Actionable Steps for Management
Effectively managing and understanding these fevers requires careful tracking and medical partnership. It is vital to consult with a physician, typically a rheumatologist, to systematically rule out underlying infections, malignancies, or other causes of fever.
Once an infectious cause is excluded, the following strategies can provide clarity and relief:
- Keep a Fever Diary: Meticulously track your temperature at consistent times each day (e.g., morning, afternoon, evening). Note any associated symptoms like chills, rash, joint pain, or fatigue to help your doctor identify patterns.
- Correlate with Activity: In your diary, log activities, stress levels, and diet to see if any specific triggers correlate with temperature spikes or disease flares.
- Rule Out Infections First: Always seek medical evaluation for a new or persistent fever. Your doctor will likely run blood tests (like CRP and ESR), cultures, and possibly imaging to ensure no infection is present, which is especially important if you are on immunosuppressive medication.
- Prioritize Comfort and Hydration: During feverish episodes, stay well-hydrated, wear light clothing, and use cool cloths to manage discomfort. Your doctor may recommend specific anti-inflammatory medications to help manage both the fever and the underlying disease activity.
6. Digestive Issues and Gastrointestinal Symptoms
Next on our autoimmune symptoms checklist are persistent digestive issues, which are far more than occasional indigestion. Because a significant portion of the body’s immune system resides in the gut, the gastrointestinal (GI) tract is a common site for autoimmune attacks. These symptoms can range from abdominal pain and bloating to chronic diarrhea, constipation, and unexplained food sensitivities, signaling that the immune system is mistakenly targeting the digestive system itself.
This isn’t just a reaction to a bad meal; it’s a chronic state of gut inflammation and distress that profoundly impacts quality of life. For instance, an individual with Celiac disease experiences severe intestinal damage and malabsorption from gluten, while someone with Crohn’s disease may suffer from debilitating abdominal cramps, urgent diarrhea, and weight loss. These symptoms serve as a critical red flag, indicating that the immune system is disrupting the body’s fundamental ability to process nutrients and eliminate waste.
Key Characteristics of Autoimmune GI Symptoms
The defining feature of autoimmune digestive issues is their chronic and often relapsing-remitting nature. Unlike a stomach bug that resolves in a few days, these symptoms persist, flare up unpredictably, and are often linked to specific triggers or systemic inflammation. They frequently accompany other autoimmune signs, like joint pain or fatigue, pointing to a body-wide process rather than an isolated gut problem.
A person with Sjögren’s syndrome might experience severe acid reflux and difficulty swallowing due to reduced saliva and enzyme production, while someone with autoimmune gastritis could develop a Vitamin B12 deficiency leading to neurological symptoms. Ignoring persistent GI distress, especially with signs like blood in the stool or unintentional weight loss, can delay the diagnosis of serious conditions.
Actionable Steps for Management
Addressing autoimmune-related GI symptoms requires a partnership with a medical professional to ensure an accurate diagnosis and rule out other causes. Before self-diagnosing or starting restrictive diets, it’s crucial to get a clear picture of what’s happening internally. A primary care doctor or internist can be a starting point for this investigation. If you are unsure about the best specialist to see, understanding the difference between internal medicine and primary care explained can help guide your decision.
Once you have a professional on board, consider these targeted strategies:
- Keep a Food and Symptom Diary: Meticulously track your food intake, beverage consumption, stress levels, and GI symptoms (e.g., bloating, pain, bowel movements) to identify patterns and potential triggers.
- Get Tested Before Eliminating Foods: If Celiac disease is suspected, it is critical to get tested before removing gluten from your diet, as eliminating it can lead to false-negative results.
- Work with a Registered Dietitian: Seek a dietitian specializing in autoimmune or GI conditions to help you navigate a medically supervised elimination diet or create a balanced, anti-inflammatory eating plan.
- Discuss Diagnostic Procedures: Do not hesitate to ask your doctor about the need for an endoscopy or colonoscopy. These procedures are often essential for accurately diagnosing conditions like Crohn’s disease, Ulcerative Colitis, or Celiac disease.
7. Dry Eyes and Dry Mouth (Sicca Symptoms)
Next on our autoimmune symptoms checklist are persistent dry eyes and a dry mouth, collectively known as Sicca symptoms. This condition arises when the immune system mistakenly targets and damages the moisture-producing lacrimal (tear) and salivary glands. While it may sound like a minor annoyance, this symptom is a significant indicator of systemic inflammation and is a classic hallmark of conditions like Sjögren’s syndrome.
This isn’t just occasional dryness from a dry room; it is a chronic, uncomfortable state that can severely impact quality of life. For example, a person with Sjögren’s syndrome might find it impossible to eat dry foods like crackers without constantly sipping water. Similarly, someone with Lupus or Rheumatoid Arthritis may develop secondary Sjögren’s and experience such severe dry eye that wearing contact lenses becomes intolerable. The resulting reduction in protective saliva and tears can lead to serious complications, including corneal damage, oral infections, and rapid dental decay.
Key Characteristics of Autoimmune Dryness
The defining feature of Sicca symptoms is their persistence and resistance to simple remedies. The dryness is often accompanied by a gritty or sandy sensation in the eyes or a “cotton-mouth” feeling that makes speaking and swallowing difficult. This symptom complex is a critical red flag because it points directly to targeted glandular destruction by the immune system, a common mechanism in autoimmune diseases like Sjögren’s, Rheumatoid Arthritis, and Scleroderma.
To help distinguish this systemic issue from everyday dryness, the following points outline its core features:
- Dryness is persistent, lasting for more than three months.
- Eyes may feel gritty, burn, or have increased light sensitivity.
- Mouth feels sticky, making it difficult to swallow or speak.
- There’s an increased need to drink liquids, especially while eating.
- It is often accompanied by other systemic symptoms like fatigue and joint pain.
Actionable Steps for Management
Managing Sicca symptoms requires a dedicated approach to restore moisture and protect the affected tissues from long-term damage. Working closely with an ophthalmologist and a dentist is crucial for preventing irreversible complications like vision loss and tooth decay.
Once an autoimmune cause is identified, consider implementing these targeted strategies:
- Hydrate Externally and Internally: Use preservative-free artificial tears multiple times a day and apply a thicker, moisturizing eye ointment at bedtime. Constantly sip water and always carry a water bottle.
- Stimulate Saliva Production: Chew sugar-free gum or suck on sugar-free lozenges to encourage salivary flow. Saliva substitutes and oral rinses can also provide significant relief.
- Optimize Your Environment: Use a humidifier in your bedroom and office to add moisture to the air, which can soothe dry eyes and nasal passages.
- Protect Your Dental Health: Due to reduced saliva, dental hygiene is paramount. Use a high-fluoride toothpaste and mouth rinse, and maintain rigorous check-ups with your dentist to catch cavities early.
- Seek Advanced Medical Care: Discuss options like prescription eye drops (e.g., cyclosporine) or procedures like punctal plugs with your ophthalmologist to help conserve your natural tears.
8. Unexplained Hair Loss (Alopecia)
Another revealing sign on the autoimmune symptoms checklist is unexplained hair loss, a condition medically known as alopecia. This goes far beyond typical shedding, manifesting as diffuse thinning, distinct bald patches, or even complete hair loss. This occurs when the immune system mistakenly attacks healthy hair follicles or when widespread systemic inflammation disrupts the natural hair growth cycle, pushing more follicles than usual into the shedding phase.
The visible nature of this symptom makes it particularly distressing and can significantly impact self-image and emotional well-being. For some individuals, it is one of the first and most alarming indicators that something is wrong internally. For example, a person with Lupus may experience significant hair thinning during a flare-up, which often improves during remission. Similarly, Alopecia Areata is a direct autoimmune attack that creates characteristic round, smooth bald patches on the scalp, beard, or other parts of the body.
Key Characteristics of Autoimmune Hair Loss
Autoimmune-related hair loss is defined by its root cause: a dysfunctional immune response. Unlike genetic pattern baldness, it is often tied to disease activity. For instance, Hashimoto’s thyroiditis frequently leads to overall thinning of scalp hair, eyebrows, and eyelashes due to its impact on thyroid hormones, which regulate the hair cycle. This symptom is a critical clue, signaling an internal inflammatory process that requires a thorough medical investigation.
Distinguishing this from other causes of hair loss is vital. The following summary box clarifies its primary features.
As the visualization demonstrates, hair loss that is sudden, patchy, or coincides with other systemic symptoms like fatigue or joint pain is a strong indicator that warrants a consultation with a specialist.
Actionable Steps for Management
Addressing autoimmune-related hair loss requires a dual approach: managing the underlying condition and supporting hair regrowth. It is crucial to work with a healthcare provider, often a dermatologist or rheumatologist, to get an accurate diagnosis.
Once the cause is identified, consider these proactive strategies:
- Document and Monitor: Take clear photos of your scalp and any affected areas regularly to track the progression of hair loss. This documentation provides valuable data for your doctor.
- Request Specific Lab Tests: Ask your physician to check thyroid function (a full panel including TSH, Free T3, Free T4, and thyroid antibodies), iron levels (especially ferritin), and vitamin D, as deficiencies can exacerbate hair loss.
- Gentle Hair Care Routine: Avoid harsh chemical treatments, high-heat styling tools, and tight hairstyles that pull on the follicles. Use gentle, sulfate-free shampoos and minimize washing frequency to reduce physical stress on the hair.
- Ask for a Dermatology Referral: If the diagnosis is unclear, a dermatologist can perform a scalp biopsy to examine the hair follicles and determine the specific cause of the alopecia. This can be instrumental in tailoring an effective treatment plan.
Autoimmune Symptom Checklist Comparison
| Symptom | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Chronic Fatigue and Exhaustion | Moderate – requires tracking and clinical evaluation | Low to moderate – diaries, OT consultation possible | Variable; symptom relief and activity pacing possible | Patients with persistent, unexplained fatigue | Early recognition aids diagnosis; guides pacing |
| Joint Pain and Swelling (Arthralgia) | Moderate to high – needs clinical and imaging tests | Moderate – imaging, blood tests, physical therapy | Good with treatment; prevents joint damage | Symmetrical joint inflammation and stiffness | Visible, measurable; responds well to therapy |
| Skin Rashes and Lesions | Low to moderate – visual assessment and dermatology consult | Low to moderate – clinical exams, biopsy if needed | Often improves with topical/systemic therapy | Visible autoimmune skin manifestations | Early diagnosis; photographic documentation |
| Brain Fog and Cognitive Dysfunction | Moderate – requires cognitive testing and monitoring | Moderate – cognitive assessments and rehabilitation | Potential improvement with disease management | Cognitive symptoms impacting daily functioning | Recognized symptom; cognitive rehab can help |
| Recurring Fever and Temperature Fluctuations | Moderate – requires consistent temperature tracking and medical evaluation | Moderate – temperature logs, lab work, imaging | Variable; may respond to immunosuppressive treatment | Unexplained low-grade or periodic fevers | Objective and measurable; indicates disease activity |
| Digestive Issues and Gastrointestinal Symptoms | Moderate to high – requires diagnostic testing and dietary assessment | Moderate to high – endoscopy, dietitian support | Often good with diet and treatment modifications | Chronic GI symptoms with suspected autoimmune origin | Assessable with tests; nutrition-focused interventions |
| Dry Eyes and Dry Mouth (Sicca Symptoms) | Moderate – requires specialized eye and saliva tests | Moderate – Schirmer’s test, antibody panels, specialist visits | Symptom management possible; prevents complications | Persistent dryness affecting eyes and mouth | Highly specific symptoms; multiple management options |
| Unexplained Hair Loss (Alopecia) | Moderate – requires dermatologic evaluation and labs | Moderate – blood tests, biopsy, dermatology treatments | Variable; some reversible, others slow to improve | Visible hair loss with autoimmune suspicion | Visible symptom; multiple treatment avenues available |
From Checklist to Conversation: Your Next Steps to Clarity
Navigating the complex landscape of your health can feel like piecing together a difficult puzzle, especially when symptoms are vague, intermittent, and seemingly unrelated. The autoimmune symptoms checklist you have just reviewed is designed not as a diagnostic tool, but as a powerful organizational framework. Its primary purpose is to help you identify and articulate patterns in your own body, transforming abstract feelings of being “unwell” into concrete data points that can guide a productive medical investigation.
Recognizing your experience in the descriptions of chronic fatigue, persistent joint pain, mysterious skin rashes, or debilitating brain fog is a critical first step. It validates your concerns and shifts the narrative from one of uncertainty to one of empowered inquiry. This checklist serves as your initial evidence-gathering tool, allowing you to move beyond simply enduring symptoms to actively documenting and understanding them.
Synthesizing Your Symptom Data
The true value of this checklist emerges when you use it to build a comprehensive health narrative. It is one thing to know you experience hair loss; it is another to correlate it with periods of intense digestive distress or a low-grade fever. The interconnectedness of these symptoms is often the key that unlocks a correct diagnosis. Autoimmune conditions are systemic by nature, meaning the body’s misguided immune attack can manifest across multiple organ systems.
Your role now is to become the primary historian of your own health. The next actionable step involves meticulous documentation. Consider creating a dedicated symptom journal, either in a physical notebook or a digital app. For each symptom from the checklist that resonates with you, record the following:
- Frequency and Duration: How often does the symptom occur, and how long does it last? Is it constant or does it come and go?
- Severity: On a scale of 1 to 10, how does it impact your daily life?
- Triggers and Mitigating Factors: What seems to make it worse (stress, certain foods, lack of sleep)? What, if anything, makes it better?
- Associated Symptoms: When you experience joint pain, do you also notice increased fatigue or a skin rash?
This detailed log is not just a collection of complaints; it is a high-value dataset that a skilled clinician can use to identify subtle patterns indicative of a specific autoimmune process.
Partnering with the Right Medical Expert
Armed with your documented observations, the next crucial step is to engage with a medical professional. However, not all clinical pathways are created equal, especially when dealing with the diagnostic complexities of autoimmunity. The journey to a diagnosis can be notoriously long and frustrating, often involving multiple specialists and inconclusive tests. This is where partnering with a top-tier, board-certified expert becomes a non-negotiable part of a successful strategy.
For discerning individuals who value precision, efficiency, and a proactive approach to health, seeking a specialist in rheumatology, immunology, or functional medicine is paramount. These experts are trained to look at the body as an integrated system and are often more familiar with the nuanced presentations of autoimmune disease. An experienced physician will not dismiss your documented symptoms but will see them as invaluable clues. They will use your autoimmune symptoms checklist and journal as a starting point for a targeted diagnostic workup, which may include advanced bloodwork, imaging, and other specialized tests.
Ultimately, this journey is about moving from a state of questioning to a state of knowing. This checklist is your launchpad. It empowers you to stop second-guessing your own experience and start a meaningful, evidence-based conversation with a medical partner who can provide the clarity and a personalized treatment plan you deserve. Your health is your most valuable asset; investing in the right expertise to protect it is the most critical decision you can make.
When your health demands the highest level of expertise, finding the right specialist shouldn’t be left to chance. The Haute MD network provides exclusive access to a curated directory of the nation’s most respected, board-certified physicians, including leading rheumatologists and immunologists who specialize in complex autoimmune conditions. Explore our network to connect with a practitioner who can provide the definitive answers and sophisticated care you deserve at Haute MD.

