The real difference between an internist and a primary care physician comes down to one thing: scope.
Internal medicine focuses strictly on adults, often diving deep into complex, chronic diseases. On the other hand, primary care offers comprehensive healthcare for patients of all ages, from newborns to the elderly. So, while an internist can be your primary care physician (PCP), not all PCPs are internists.
Unpacking The Key Distinctions

Although people often use the terms interchangeably, getting clear on their unique roles helps you pick the right doctor for your needs. Primary care is best seen as the central hub for your health—a broad field that includes several different specialists.
It helps to think of “primary care” as an umbrella term. Under that umbrella, you’ll find:
- Family Physicians: The true generalists, treating patients of every age.
- Pediatricians: Specialists focused exclusively on children’s health.
- Internists: Specialists focused exclusively on adult health.
So, while internal medicine falls under the primary care umbrella, it represents a very specific focus. Internists are specialists in preventing, diagnosing, and managing diseases in adults. Their training is intensely focused on complex adult physiology and how multiple medical conditions can interact. This makes them exceptionally skilled at managing chronic illnesses.
Key Insight: The fundamental difference is specialization. Internal medicine is a specialty zeroed in on adults, with a heavy emphasis on diagnosing and treating complex conditions. Primary care is a broader field providing continuous care for patients of all ages. You can explore more primary care data to see how these roles function within the larger healthcare system.
This deep specialization often makes internists the ideal choice for adults juggling one or more chronic conditions like diabetes, heart disease, or autoimmune disorders. In contrast, a family medicine doctor offers a much wider range of services—including pediatric and sometimes even obstetric care—making them perfect for families who want a single trusted physician for everyone.
Quick Comparison: Internal Medicine vs. Primary Care
For a quick breakdown, this table highlights the fundamental differences between the two fields at a glance, focusing on the most important distinctions.
| Attribute | Internal Medicine (Internist) | Primary Care Physician (PCP) |
|---|---|---|
| Patient Age | Adults only (18+) | All ages (infants to seniors) |
| Scope of Practice | Diagnosis and management of complex adult illnesses; preventative care | Comprehensive, continuous care for all ages; preventative health; routine check-ups |
| Common Settings | Outpatient clinics, hospitals (as hospitalists) | Primarily outpatient clinics |
| Typical Focus | Depth of knowledge in adult diseases | Breadth of knowledge across the entire lifespan |
Ultimately, both paths lead to highly skilled physicians, but their training and day-to-day focus are tailored to serve different patient needs.
Analyzing Physician training and Educational Paths
To really get the practical difference between internal medicine and family medicine, you have to look at how these doctors are made. After four grueling years of medical school, every new physician enters a residency program. This is where the real, hands-on training happens, and it’s this intense period that forges them into specialists.
For internists and family medicine docs, this is where their paths split, and that divergence shapes everything about how they practice medicine.
The Internal Medicine Residency Focus
An internal medicine residency is a three-year deep dive, focused exclusively on one thing: the adult patient. This isn’t a jack-of-all-trades program; it’s designed to build profound expertise in the complicated, often messy, interplay of diseases that affect adults.
The training is heavily weighted toward managing complex chronic conditions—think heart failure, diabetes, and tricky autoimmune disorders. A huge chunk of their residency is spent inside the hospital, learning to manage acutely ill patients and act as the quarterback for care involving multiple organ systems.
This curriculum is narrow by design, but it goes incredibly deep. Core components include:
- Hospital-Based Rotations: Residents spend a massive amount of time on general medicine wards, in intensive care units (ICUs), and in cardiac care units (CCUs). This is where they master the management of severe, life-threatening illnesses.
- Subspecialty Exposure: They rotate through the full gamut of adult subspecialties, from cardiology and endocrinology to rheumatology and gastroenterology. This gives them a robust understanding of specialized adult care, even if they don’t subspecialize themselves.
- Continuity Clinic: Alongside hospital work, they manage a panel of their own adult patients in an outpatient clinic. This teaches them the critical skill of handling long-term chronic disease over many years.
The entire structure is engineered to produce physicians who are not just caregivers, but true medical detectives for the mysteries of adult health.
An internist’s training is like becoming a specialist for the entire adult body. They are trained to diagnose and manage the most complex and puzzling conditions that affect adults, often acting as a consultant to other physicians.
The Family Medicine Residency Scope
In stark contrast, a family medicine residency offers a much broader, more panoramic view of medicine. It’s also a three-year program, but its goal is to create a versatile physician who can care for the entire family unit, from cradle to grave.
Their training spans the full spectrum of life. Instead of the adult-only focus of internal medicine, family medicine residents gain significant hands-on experience in several crucial, distinct areas.
- Pediatrics: They learn to manage everything from newborn wellness checks and developmental milestones to adolescent health issues.
- Obstetrics and Gynecology: This training often includes prenatal care, delivering babies, and managing women’s health concerns.
- Geriatrics: They also develop specific expertise in the unique health challenges that come with aging, from dementia to mobility issues.
This all-encompassing approach equips family medicine doctors to provide continuous, whole-person care. It makes them the perfect fit for families who want one trusted physician for everyone. Their training perfectly highlights the “breadth over depth” philosophy that truly separates them from their internal medicine colleagues.
Comparing the Scope of Medical Practice
While the training paths set the stage, the day-to-day reality of medical practice is where the differences between internists and primary care physicians truly come alive. It boils down to a classic trade-off: depth versus breadth. Each approach serves different patients in profoundly different ways.
An internist’s world is defined by a deep, almost forensic focus on adult health, especially when things get complicated. Think of them as the medical detectives for the adult body, expertly managing patients juggling multiple, often interacting, chronic diseases.
Their expertise truly shines when facing challenges like uncontrolled diabetes, congestive heart failure, or complex autoimmune disorders such as lupus or rheumatoid arthritis. This requires a granular understanding of adult physiology and pharmacology that is second to none.
The Internist as the Ultimate Problem-Solver
Internists are masters at diagnosing puzzling symptoms and orchestrating intricate treatment plans that often involve a team of specialists. Their hospital-heavy training makes them particularly skilled at managing severe illness and coordinating care for hospitalized adults, cementing their reputation as the go-to diagnosticians for the toughest cases.
Internists are often called the “doctor’s doctor.” Their specialized training equips them to untangle complex medical puzzles in adults, making them a crucial resource for both patients and other physicians facing diagnostic challenges.
This specific skill set is exactly why many adults with significant chronic illnesses choose an internist for their primary care. If this level of dedicated adult care appeals to you, exploring the role of concierge internal medicine doctors can offer more insight into this highly focused model. Their practice structure allows them to dedicate the necessary time to the nuances of adult disease.
Workforce data reflects this focus. In the U.S., general internal medicine physicians make up a substantial 34.5% of the primary care workforce, bringing years of specialized experience to the table—an invaluable asset when managing the complexities of adult health.
The Primary Care Physician as a Lifelong Health Quarterback
In sharp contrast, a primary care physician’s scope is defined by its remarkable breadth. Their role isn’t just about diagnosing illness; they are the central coordinators of a patient’s entire health journey, from their first days of life through their senior years.
A typical day for a family doctor involves a massive range of responsibilities:
- Preventative Care: Giving immunizations, ordering routine screenings like mammograms or colonoscopies, and providing critical lifestyle counseling.
- Acute Illness Management: Treating common issues like sinus infections, colds, and minor injuries for every member of a family.
- Chronic Disease Oversight: Handling the initial management of widespread chronic conditions like high blood pressure and asthma, and knowing precisely when to call in a specialist.
- Care Coordination: Serving as the main point of contact between different specialists and healthcare services, ensuring nothing falls through the cracks.
This “cradle-to-grave” approach builds incredibly deep, long-term relationships with patients and their families. It’s not uncommon for a family physician to give a baby their first shots, treat that same person for strep throat as a teenager, manage their blood pressure in middle age, and later, care for their aging parents.
This continuous relationship provides a powerful context for understanding a patient’s health over their entire life. Ultimately, the best choice depends on your needs: the deep, diagnostic expertise of an internist for complex adult issues, or the broad, lifelong coordination of a primary care physician.
Typical Patient Populations and Clinical Settings
Where a doctor practices and who they see every day tells you almost everything you need to know. The clinic environment and patient demographics are what truly separate internal medicine from primary care, creating two fundamentally different approaches to health.

An internist’s patient base is clear-cut: they exclusively treat adults. This sharp focus allows them to develop a deep, nuanced understanding of the complex diseases that show up in adulthood and evolve with age. But it’s their work environment that really sets them apart.
The Internist Environment: Bridging Two Worlds
Internists are medical chameleons, equally at home in an outpatient clinic and the fast-paced world of a hospital. This dual-threat capability is a huge differentiator. In the clinic, they function as primary care doctors, managing chronic conditions and preventive health for their adult patients over many years.
But many internists also practice as hospitalists—physicians who specialize in caring for hospitalized patients. This creates a powerful, almost seamless, continuity of care. Imagine your internist managing your hypertension in their office, and then personally directing your treatment if you’re ever admitted to the hospital for a related cardiac issue.
Key Takeaway: The ability for internists to work as hospitalists creates a critical bridge between outpatient and inpatient care. This ensures the doctor who knows your complex history best is the one guiding your treatment during a serious illness.
This constant exposure to the hospital environment makes them exceptionally skilled at diagnosing and managing acute, severe illnesses. It hones their diagnostic instincts, whether they’re in a routine check-up or standing in an emergency room.
The Primary Care Physician Setting: The Community Hub
Contrast that with the world of a primary care physician, especially a family medicine doctor. Their practice is planted firmly in the outpatient clinic, designed to be the central health hub for an entire community. They don’t just treat individuals; they often care for multiple generations of the same family.
A family doctor’s daily schedule is a cross-section of life itself. They might go from:
- Performing a wellness check on a newborn baby.
- Giving a school-aged child their vaccinations.
- Managing a teenager’s asthma.
- Counseling a middle-aged adult on lifestyle changes.
- Adjusting medications for an elderly patient with several chronic diseases.
This incredibly broad scope means their practice is built on long-term, trusting relationships. The family doctor knows the family history not because it’s in a chart, but because they’ve lived it alongside the family, caring for grandparents, parents, and children. Their focus is less on acute intervention and more on being a continuous, lifelong partner in health, making them a true cornerstone of the community.
How to Choose the Right Physician for Your Needs
Deciding between an internist and a primary care physician isn’t about which one is “better”—it’s about which one is better for you. The right choice really hinges on your specific life stage, current health challenges, and whether you’re managing care for just yourself or a whole family. It’s a decision that should line up with both your immediate needs and your long-term health goals.
For a young, healthy adult, the difference might seem subtle. But for someone managing a complex chronic illness like lupus or Crohn’s disease, an internist’s deep, specialized knowledge of adult pathology is a game-changer. Their entire training is geared toward untangling exactly these kinds of medical complexities.
This decision tree infographic can help you visualize how different patient scenarios map to the most suitable physician.
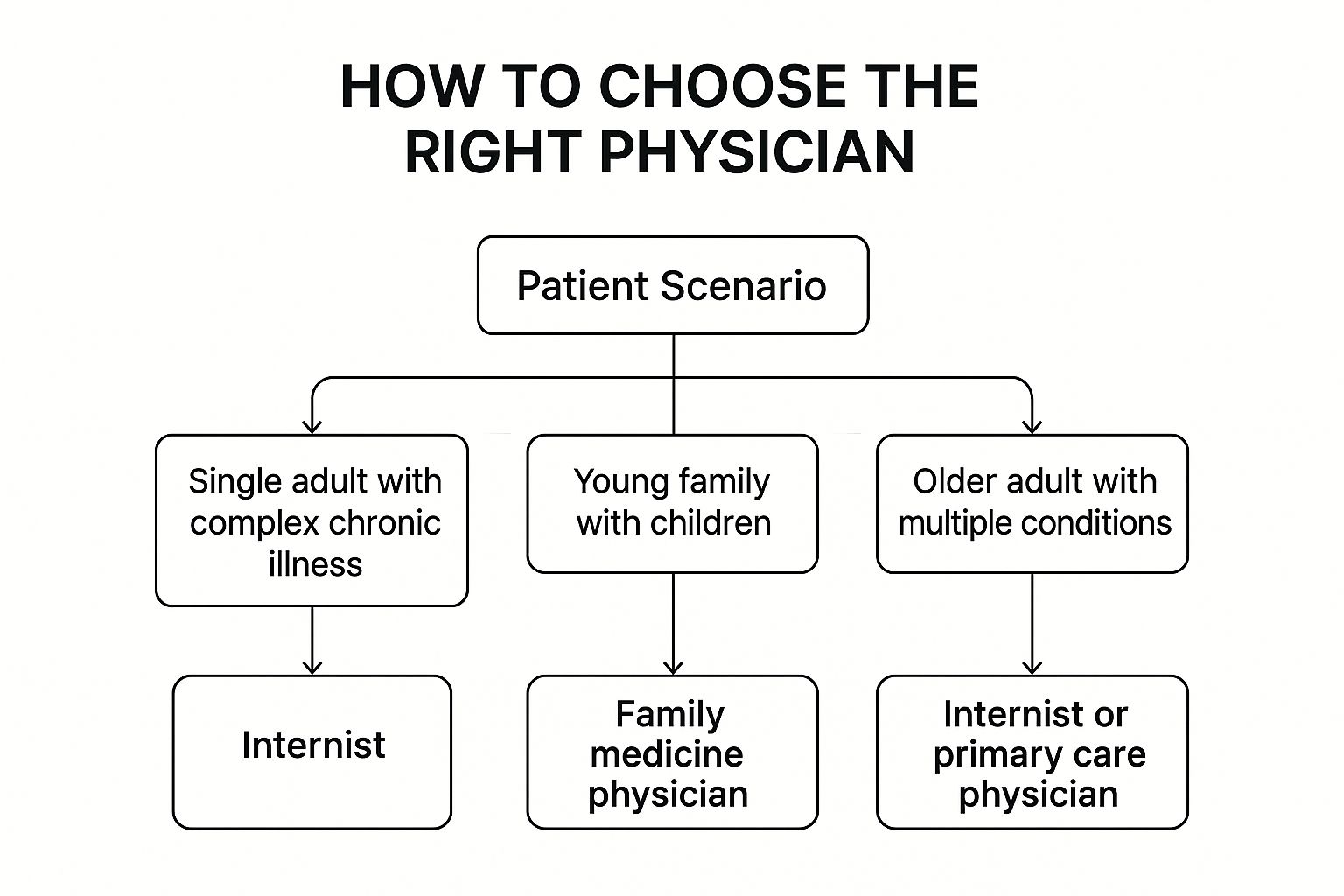
As the visualization makes clear, your personal health profile is the most critical factor. Whether you’re navigating a tough diagnosis or coordinating checkups for your kids, that context will point you to the right partner.
Scenarios for Choosing an Internist
An internist is often the ideal primary care physician for adults facing very specific health situations. Their focused training in adult medicine gives them a distinct edge in managing intricate health profiles and complex diagnostic puzzles.
You should seriously consider an internist if you are:
- An adult with one or more chronic conditions. If you have something like diabetes, heart disease, or hypertension, an internist’s expertise in how these diseases interact is invaluable.
- An older adult with multiple health issues. Geriatric care is a true cornerstone of internal medicine, which makes them incredibly adept at handling the complex, overlapping needs of aging patients.
- A patient with a hard-to-diagnose illness. Internists are renowned as the medical world’s diagnosticians, skilled at solving the complex puzzles that might stump other physicians.
Key Takeaway: An internist shines in situations that demand deep diagnostic skill and sophisticated management of adult-specific diseases. They are, first and foremost, specialists in the complexities of the adult body.
Situations Favoring a Family Medicine Doctor
While an internist offers incredible depth, a family medicine doctor provides exceptional breadth. This makes them a perfect fit for a whole different set of circumstances, where continuity of care for every member of a family is the top priority.
A family medicine doctor is likely your best choice if you:
- Have young children. They are fully trained in pediatrics and can manage your child’s health from infancy all the way through adolescence, which dramatically simplifies care for the whole family.
- Want a single doctor for your entire household. The convenience and peace of mind that come from having one trusted physician for yourself, your partner, and your kids simply cannot be overstated.
- Prefer a long-term relationship built on broad health oversight. Family doctors excel at preventative care and promoting wellness for patients at every single stage of life.
Choosing the right physician is a foundational step in taking control of your health. If you are ready to see who is out there, a great next step is to find a doctor in your area who aligns with your personal needs.
Making the Final Decision
To make your choice even clearer, the table below breaks down a few common situations and offers a direct recommendation. Think of it as a practical guide to match your personal health profile with the right medical expert.
Which Doctor Is Right for You? A Scenario-Based Guide
This table matches common patient scenarios and life stages with the most suitable type of physician to help you make an informed decision.
| Your Situation | Recommended Physician | Reasoning |
|---|---|---|
| A young family with two children | Family Medicine Physician | They are trained in pediatrics and adult care, providing a single point of contact for the entire family’s health needs. |
| A single adult with well-managed asthma | Either is suitable | For routine adult care without major complexities, both an internist and a family doctor are excellent choices. |
| An older adult with heart failure and diabetes | Internist | Their specialized training in complex, interacting adult diseases makes them uniquely qualified to manage this scenario. |
Ultimately, understanding the subtle yet significant difference between internal medicine and primary care empowers you to select a physician who can best serve as your trusted health partner for years to come.
Where Primary Care Fits in the Brodader Healthcare System
Understanding the clinical differences between internal medicine and family practice is one thing, but it’s just as important to see where these physicians fit into the massive U.S. healthcare machine. Both specialties are the bedrock of community health. They’re the first line of defense against illness and the navigators for a medical landscape that’s often overwhelmingly complex. Their impact goes far beyond any single patient visit.
It’s a well-established fact: strong primary care is directly linked to better health outcomes, lower death rates, and reduced healthcare costs. Communities with more primary care doctors are simply healthier. This makes the ongoing shortage of these physicians a genuine public health crisis.
Systemic Pressures and Their Toll
Both internists and family doctors are grappling with immense systemic pressures that directly impact patient care. They’re buried under heavy administrative burdens, facing staggering rates of professional burnout, and dealing with significant pay gaps compared to other medical specialties. These are the real-world factors that shape a doctor’s career path and the kind of practice they ultimately choose.
Key Insight: The financial and systemic hurdles in primary care reveal a stark reality in the healthcare landscape. Primary care physicians consistently earn less than specialists, a major driver of burnout and workforce shortages. The U.S. has a notably lower percentage of physicians in primary care compared to countries like Australia, which boasts a much higher density of these essential doctors.
These systemic failures have pushed many physicians to seek out alternative practice models—models that allow them more time with patients and a real chance to focus on preventive medicine. These newer approaches are designed to fix what’s broken in traditional care. Our guide comparing concierge medicine vs. traditional healthcare dives deeper into how these models are changing the game.
Ultimately, the role of primary care physicians—whether they’re internists or family doctors—cannot be overstated. They are the cornerstone of an effective, efficient, and equitable healthcare system. Supporting them isn’t just about supporting doctors; it’s about investing in the health of our entire community.
Common Questions, Answered
After digging into the core differences, a few practical questions usually pop up. Let’s clear those up so you can feel confident about choosing the right doctor for your health.
Can an Internist Be My Primary Care Physician?
Yes, absolutely. A general internist is perfectly trained to act as your primary care physician (PCP), but exclusively for adults. They are more than equipped to handle your overall health, from routine physicals to managing the full spectrum of adult illnesses.
The only real limitation is their patient population—they don’t see anyone under the age of 18. For an adult, especially one managing a chronic condition, an internist is often an outstanding choice for a primary doctor.
Think of an internist as a PCP who brings the comprehensive, preventive mindset of primary care and combines it with a specialist’s deep knowledge of complex adult diseases. It’s a uniquely powerful partnership for adult patients.
Do I Need a Referral to See an Internist?
It really depends on the situation. If you’re choosing an internist to be your main doctor—your PCP—you almost certainly do not need a referral. You can just call their office and schedule an appointment like you would with any other primary care provider.
However, things change if your current PCP is sending you to an internal medicine subspecialist. For instance, if you need to see a cardiologist for a heart issue or an endocrinologist for a thyroid problem, a referral is often necessary. This is usually dictated by the rules of your health insurance plan.
Should I Choose a Family Doctor or an Internist?
This decision comes down to your household’s needs. If you have children and want the simplicity of a single, trusted doctor for everyone in the family, a family medicine physician is the ideal choice. They provide that seamless continuity of care from infancy through adulthood.
But if you’re an adult without pediatric needs in your household, an internist is a superb option. This is particularly true if you’re navigating chronic or complex health issues, where their specialized focus on adult medicine provides a significant layer of expertise. Both are excellent primary care choices, just tailored for different stages of life.
At Haute MD, we connect discerning patients with the nation’s top-tier physicians, from leading internists to elite specialists. Find a trusted, vetted expert who aligns with your health goals by exploring our network. Visit Haute MD today.

